|
Laxman G. Jessani1, Satish Nayak2, PreethI Lingam2, Vinay Devraj1, Sarojini Parameswaran2, Ram Gopalakrishnan1, V Ramasubramanian1,
Department of Infectious Diseases1and Gastroenterology2
Apollo Hospital, Chennai, India
Corresponding Author:
Dr. Laxman G. Jessani
Email: laxmanj27@gmail.com, laxmanj_27@yahoo.com
48uep6bbphidvals|1374 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Transjugular intrahepatic portosystemic shunt (TIPS) is commonly used for the decompression of portal hypertension. TIPS infection, also known as ‘endotipsitis’, is a rare but serious complication of TIPS insertion.[1] To date approximately 42 cases of ‘endotipsitis’ have been described. To the best of our knowledge this is the first case report of endotipsitis caused by an extremely drug-resistant Klebsiella pneumoniae (XDR).[2]
Case report
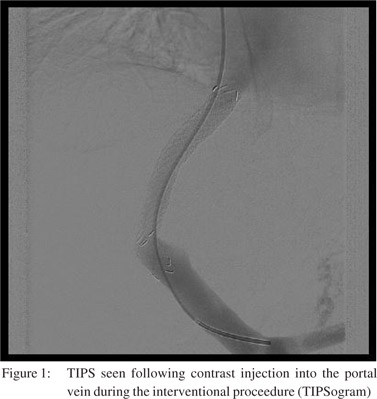
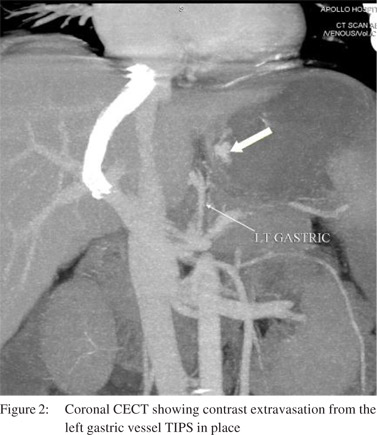
A 28-year-old man with decompensated chronic alcohol-related liver disease was admitted with upper gastrointestinal bleeding. He had no history of hospitalization in the previous 6 months. He underwent TIPS insertion due to variceal bleeding which did not respond to endoscopic variceal ligation. Three days post TIPS procedure he developed ARDS with leukocytosis, hyperbilirubinemia, elevated aminotransferases, hypoalbuminemia, coagulopathy and septic shock. Two sets of blood cultures grew extremely drug resistant (XDR) Klebsiella pneumoniae (resistant to all antibiotics tested including carbapenems, colistin, and tigecycline). Workup, including urine culture, transthoracic echocardiography, chest radiography, abdominal imaging, and diagnostic paracentesis, failed to localize the source of the bacteremia. He initially improved with a combination of multiple antibiotics (imipenem, colistin, tigecycline, chloramphenicol, amikacin, ciprofloxacin and fosfomycin). However he had re-bleeding: Doppler ultrasound did not show any thrombus and CT angiogram revealed left gastric artery bleeding for which embolisation was performed. His TIPS was re-examined via transjugular route to look for any thrombus. Stent patency was confirmed; however in view of the recurrent bleed, TIPS stent dilatation with balloon was done. After transient improvement he again developed fever, worsening of sepsis and persistent XDR Klebsiella bacteremia with the same antibiotic-resistance pattern, seven days after the initial blood culture positivity without any other source of infection. Endotipsitis was diagnosed based on the time frame of infection, presence of the TIPS serving as a potential nidus of infection in the absence of other source of infection. Liver transplantation was planned but before a donor was identified, he deteriorated and expired despite multiple antibiotic courses and supportive care.
Discussion
Endotipsitis i.e. persistent TIPS infection, first described by Sanyal and Reddy in 1998[1] has an overall incidence that varies from 1.7 - 5.1%.[3] Endotipsitis can occur as an early infection if occurring within 120 days of TIPS procedure or late infection if occurring after this period. These differ in terms of the causative agents and pathogenesis.[3] Although the clinical presentation of endotipsitis is variable, fever is a constant feature. Worsening jaundice, increasing ascites, recurrent variceal bleeding and shock are also described and attributed to TIPS occlusion. Laboratory findings include leukocytosis, anemia, hyperbilirubinemia, elevated aminotransferases, hypoalbuminemia and coagulopathy similar to our case. The exact diagnostic criteria of endotipsitis are still being debated.[4] The “gold standard” for diagnosis of tipsitis is removal of stent and culturing the stent which is possible only during liver explants at time of transplantation or autopsy. Tissue cultures obtained from direct endothelial biopsy performed from within the TIPS[5] is not widely available and is not required for the definitive diagnosis of endotipsitis. “Definite infection” as described by Sanyal & Reddy is defined as clinically significant continuous bacteremia (fever and multiple positive blood cultures) along with vegetation or thrombi inside the TIPS. “Probable infection”, as in our patient, is defined as sustained bacteremia and unremitting fever in a patient with apparently normal TIPS without any other identifiable source of infection 1. De Simone et al[6] described stricter criteria to define sustained bacteremia as two blood cultures drawn 4-12 h apart that were positive for the same organism without another identifiable source of bacteremia. Later Armstrong and MacLeod[3] put forth a more specific standardized definition requiring sustained bacteremia in a patient with a TIPS device, with or without thrombus, plus no other identifiable infective focus, after an exhaustive workup. They defined sustained bacteremia as two or more blood cultures positive for the same organism, the first and last being separated by 7 days or more.
Our case fulfils the above definitions
TIPS stenosis or thrombosis, a strong risk factor is reported in 47% cases as demonstrated by ultrasound, doppler-imaging or other methods [4]. In our case doppler ultrasound and TIPS revision was done to assess TIPS patency or TIPS-biliary fistula. Other tests included negative urine, tracheal secretions, and ascitic fluid cultures. Chest radiographs, CT abdomen and angiogram, transthoracic echocardiography, upper and lower gastro-intestinal endoscopy were done to rule out deep-seated infections.
Removal of shunt continues to be the “gold standard” treatment of endotipsitis; however, treatment is essentially medical therapy as per culture, because TIPS is irremovable without liver transplantation. In the literature, medical treatment was ineffective in the eradication of infection in 10 cases, all of who died (seven with definite endotipsitis and three with probable endotipsitis).[4]
Reference
- Sanyal AJ, Reddy KR. Vegetative infection of transjugular intrahepatic portosystemic shunts. Gastroenterology. 1998;115:110–5.
- Paterson DL, Doi Y. A step closer to extreme drug resistance (XDR) in gram-negative bacilli. Clin Infect Dis.2007;45:1179–81.
- Armstrong PK, MacLeod C. Infection of transjugular intrahepatic portosystemic shunt devices: three cases and a review of the literature. Clin Infect Dis. 2003;36:407–12.
- Mizrahi M, Adar T, Shouval D, Bloom AI, Shibolet O. Endotipsitis-persistent infection of transjugular intrahepatic portosystemic shunt: pathogenesis, clinical features and management. Liver Int. 2010;30:175–83.
- Dobbins BM, Kite P, Catton JA, Wilcox MH, McMahon MJ. In situ endoluminal brushing: a safe technique for the diagnosis of catheter-related bloodstream infection. J Hosp Infect. 2004;58:233–7.
- DeSimone JA, Beavis KG, Eschelman DJ, Henning KJ. Sustained bacteremia associated with transjugular intrahepatic portosystemic shunt (TIPS). Clin Infect Dis. 2000;30:384–6.
|