Gaurav PS Gahlot1, Maitrayee Roy1, Hemant Jain2, Nihar Ranjan Dash2, Madhusudhan KS3, Vaishali Suri1, Rajni Yadav1, Prasenjit Das1
Departments of Pathology1,
Gastrointestinal Surgery2
and Radiodiagnosis3,
All Indian Institute of Medical Sciences,
New Delhi, India
Corresponding Author:
Dr Prasenjit Das
Email: prasenaiims@gmail.com, dr_prasenpgi@yahoo.co.in
48uep6bbphidvals|1373 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Extraskeletal osteosarcoma (ESOS) is an uncommon malignant mesenchymal neoplasm constituting 1% of all soft tissue sarcomas[1] and 2-4 % of all osteosarcomas (OS). Though the primary skeletal OS is a common bone tumor of the first andsecond decades, ESOS has been reported in the elderly (60-70 years).1 Allan’s criteria for diagnosis of ESOSinclude: the tumor, (1) to be ofsoft tissue origin without any attachment to bone/periostium, (2) to have a uniform sarcomatous morphology without carcinomatous area and (3) shouldproduce malignant osteoid, bone or cartilaginous matrix.[2] The present article reports a primary ESOS of gall bladder (GB) in a 72 year old female . To the best of our knowledge this is the second case of the primary ESOS of the GB.[3] A written informed consent was taken in the index case.
Case report
A 72 year old diabeticfemale with coronary artery disease, bronchial asthma, hemiparesis and depression,presentedwith off and on pain on the right hypochondrium, radiating to the ipsilateral sub-scapular region for last 3 years,with loss of appetite and weight (lost10 kgsover 10 months). She had jaundice 2 years back, which resolved spontaneously.Onlocal examination and contrast enhanced computer tomogram (CECT) a distended GB with heterogeneous soft tissue within the lumen anddilated common bile duct (CBD) was noted without calcification or extra-luminal extension (Figure 1A). Magnetic resonance cholangiopancreatography (MRCP) also showed similar filling defects in the GB and lower CBD (Figure 1B).
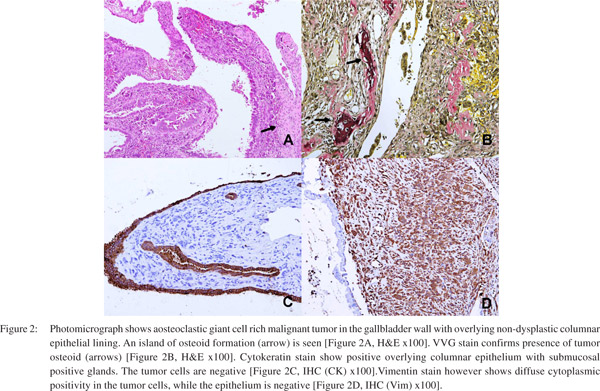
Radiologically, possibilities considered were: empyema with sludge and calculi or hydatid cyst with rupture. Carcinoma was not considered, as no definite wall thickening or soft tissue extension seen. Ultrasound guided fine needle aspiration cytology (FNAC) showed a few highly atypical cells, suggestive of a malignant tumor. The patient underwent cholecystectomy with partial CBD excisionas it was adherent to the duodenum and on per-operative frozen section examination a positive CBD margin was identified. No lymph node was identified. Grossly a polypoidal friable growth measuring 4.5x4x0.2 cms was identified near fundus of GB, involving the CBD, with attached liver bed measuring 3.2x1.5cms and a free liver margin of 2.1 cms. Microscopically, a pleomorphic malignant tumor infiltrating the wall of GB with overlying normal epithelial lining was seen. Within the tumor, numerous osteoclastic giant cells were noted with significant nuclear pleomorphism and foci of osteoid formation by the malignant cells, as confirmed by Verhoeff- Van Gieson stain (arrows) (Figure 2A& 2B). The proximal CBD margin was also involved by the tumor cells.
Immunohistochemistry (IHC) showed positivity for osteopontinand vimentinin the tumor cells andnegativity for pan-CK, CK19, myogenin and desmin (Figure 2C & D). The overlying epithelium was, however positive for CK. Histopathological (HPE) diagnosis of an ESOS (osteoblastic variant) of GB was made. Postoperative period was uneventful and positron emission topography (PET) showed no systemic
uptake and she was further advised for close follow up (Figure1C & D).

Discussion
ESOS was first described by Wilson in 1941. Primary ESOS is a rare high grade sarcoma that arises from deeper soft tissueswith male predominance (1.9:1). The exact etiologyis unknown, however, two theories have been described: (a) tissue residue theory (embryogenic mesoblastic rest) and (b) metaplastic theory (of the interstitial fibroblastsby radiation exposure, trauma, surgery, etc.).[4]
As radiological features are nonspecific, a HPE examination is mandatory for diagnosis.[4,5] Six histological subtypes, similar to those of the skeletal OS are: (1) osteoblastic, (2) fibroblastic, (3) chondroblastic, (4) teleangectatic, (5) small cell and (6) well differentiated Os.In the index case the diagnosis of osteoblastic ESOS was made due to the presence of abundant osteoidina tumor with histology similar to the classical OS. Amongst the intra-abdominal ESOS, kidney, followed by the retroperitoneum and mesentery are other reported sites. Differential diagnosis are benign myositis ossificans, mature teratoma or calcified paragangliomas. Amongst the malignant tumors, undifferentiated giant cell rich carcinoma, sarcomatoid carcinoma with osteoclast like giant cells, carcinomsarcoma, dedifferentiated liposarcoma, extra skeletal mesenchymal chondrosarcoma, malignant mesenchymoma and malignant fibrous histiocytomas are to be considered in GB.[4,6,7] The “reverse zoning phenomenon”of ESOS, i.e. centrally placed osteoid and peripheral spindle cell proliferation, can differentiate from the “zoning phenomenon” of myositis ossificans (periphery with most mature component).[6] Histologically this was a malignant tumor and lack of CK positivity in the tumor cells, with vimentin expression and negativity for other markers made us to rule out carcinosarcoma or sarcomatoid carcinomas. De-differentiation was not identified. Considering all features, a diagnosis of ESOS was confirmed. To the best of our knowledge, this is the second report of this entity.[3]
The treatment ofchoice in ESOS is wide/ radical/ simple surgical resection, depending on the location and extent of lesion. However, high rates of recurrence (45%) and metastases (65%) results in short median survival time of 2 years, with 5- year overall survival rate of <37%.[4,9] Other known prognostic factors are: tumor size>5 cms in diameter, elderly age group and serum alkaline phosphatase levels. Lung (60%), followed by the regional lymph nodes, heart, bone and soft tissuesare the most preferred site for metastases of ESOS.[4,9] Though efficacy is not fully established, the survival rate may be improved by post-operative radiotherapy or chemotherapy, especially in young adults, as seen in well differentiated ESOS, with a reduced recurrence rate of 28%, in comparison to the 48% recurrence in surgically excised tumors without radiotherapy.[10] As rarely reported, there is no prognostic or therapeutic data available for the primary ESOS of GB. Though in the present case, the CBD margin was positive, however, in view of patient’s old age and other co-morbidities, the patient was kept on close follow up and further not subjected to adjuvant treatment.
Conclusion
Primary ESOS of GB is an extremely rare tumor,with its predilection for elderly patients and atypical radiological findings. However, intra-abdominal ESOS is not so uncommon; so in an elderly patient with atypical radiological features and aggressive clinical course, this tumor should be considered in the differential diagnoses. Possibility of metastasis should always be ruled out and individualistic treatment should be tried, to build knowledge on these tumors.
References
- Bane BL, Evans HL, Ro JY, Carrasco CH, Grignon DJ, Benjamin RS, Ayala AG. Extraskeletal osteosarcoma. A clinicopathological review of 26 cases. Cancer. 1990;65:2762–70.
- Allan CJ, Soule EH. Osteogenic sarcoma of the somatic soft tissues. Clinicopathologic study of 26 cases and review of literature. Cancer. 1971;27:1121–33.
- Olgyai G, Horvath V, Banga P, Kocsis J, Buza N, Olah A. Extraskeletal osteosarcoma located in the gallbladder. HPB (Oxford). 2006;8:65–6.
- Lee JS, Fetsch JF, Wasdhal DA, Lee BP, Pritchard DJ, Nascimento AG. A review of 40 patients with extraskeletal osteosarcoma. Cancer. 1995;76:2253–9.
- Choudur HN, Munk PL, Nielson TO, Ryan AG. Primary mesenteric extraskeletal osteosarcoma in the pelvic cavity. Skeletal Radiol. 2005;34:649–52.
- Weiss SW, Goldblum JR. Extraskeletal osteosarcoma. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss’s soft-tissue tumors, 4th ed. St. Louis: Mosby; 2001.
- Choi JE, Chung HJ, Yoo WJ, Chung MH, Sung MS, Lee HG, et al. Retroperitoneal malignant mesenchymoma: a case of mesenchymal mixed tumor with osteosarcoma, leiomyosarcoma, liposarcoma and fibrosarcoma. Korean J Radiol. 2002;3:264–6.
- Sordillo PP, Hajdu SI, Magill GB, Golbey RB. Extraosseousosteogenic sarcoma. A review of 48 patients. Cancer. 1983;51:727–34.
- AhmadSA, Patel SR, Ballo MT, Baker TP, Yasko AW, Wang X, et al. Extraosseous osteosarcoma: response to treatment and longterm outcome. J Clin Oncol. 2002;20:521–7.
- Goldstein-Jackson SY, Gosheger G, Delling G, Berdel WE, Exner GU, Jundt G, et al, Cooperative Osteosarcoma study Group Coss. Extraskeletal osteosarcoma has a favorable prognosis when treated like conventional osteosarcoma. J Cancer Res Clin Oncol. 2005;131:520–6.
|