Vikas Pandey, Kaivan Shah, Nilesh Pandav, Meghraj Ingle, Aniruddha Phadke, Prabha Sawant
Department of Gastroenterology
Lokmanya Tilak Municipal Medical College &
Lokmanya Tilak Municipal General Hospital,
Sion Mumbai, India
Corresponding Author:
Dr. Vikas Pandey
Email: drvikas_pandey@rediffmail.com
48uep6bbphidvals|1371 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Acute or chronic pancreatitis is associated with complications like pseudocyst, pancreatic necrosis, splenic vein thrombosis, pancreatic ascites and pleural effusion. Rarely do we find a patient presenting with cardiac tamponade and gross pericardial effusion due to a pancreaticopericardial fistula. Here we report a case of pancreaticopericardial fistula complicating alcoholic chronic pancreatitis, managed successfully by ERCP and stenting.Surgery, generally considered treatment of choice, was avoided.
Case report
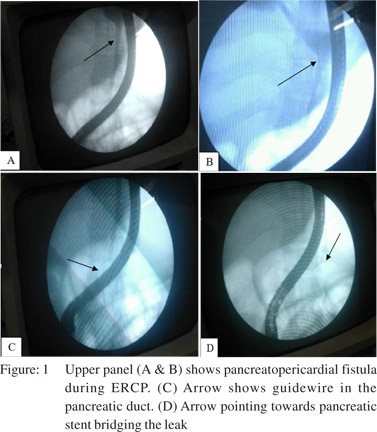
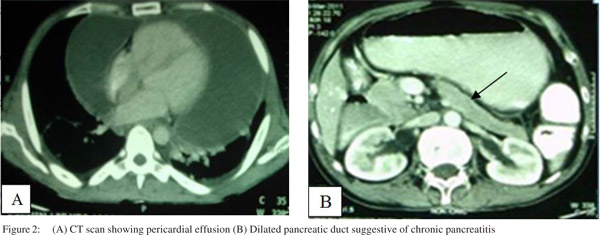
A 38-year-old male patient presented to the emergency department with a 2-day history of severe breathlessness, chest pain and abdominal pain. His symptoms had gradually progressed over 1month with dyspnea progressing from NYHA class 1 to class 4.Hewas admitted in medical intensive care unit with hypotension, tachycardia, pallor, and tachypnea. Examination revealed muffled heart sounds, elevated JVP, normal respiratory examination. Abdominal examination revealed epigastric tenderness and shifting dullness. His hemoglobin was 9.8g/dL, TLC 15,000,serum creatinine 0.7mg/dL, BUN 8mg/dL, random sugar 84mg/dL, total protein 5.6g/dL and serum albumin 2.9g/dL and normal serum electrolytes. Serum bilirubin, SGPT, SGOT, prothrombin time with INR were normal. Bedside X-ray chest revealed water bottle shape heart which was suggestive of pericardial effusion. Urgent pericardiocentesis was performed and 1000mL fluid removed. The next day the patient again complained of dyspnea, CT thorax revealed gross pericardial effusion with collapse of right atrium and right ventricle. Patient was retapped and percutaneous drain left in situ. Ultrasound abdomen showed mild to moderate ascites, heterogenous pancreas with prominent pancreatic duct. His past history revealed multiple episodes of severe abdominal pain for which he was admitted twice, and managed conservatively. The patient was consuming 1-2quarters of country liquor/day. Serum amylase, ascitic and pericardial fluid amylase levels assessment and CECT abdomen, were advised. Ascitic fluid analysis revealed low SAAG with high protein, and ascitic and pericardial fluid amylase were high (2500-3000IU/L).CECT abdomen revealed dilated MPD (main pancreatic duct), pseudocyst in head region extending upto epigastrium and communicating with collection under the dome of diaphragm and with pericardial effusion. ERCP was performed, pancreaticogram revealed pancreatic dye leaking into the posterior mediastinum and communicating with the pericardial cavity thus forming an effusion. Pancreatic sphincterotomy was done and 5Fr×12 cm stent was deployed bridging the leak. Post stenting the patient improved with gradual disappearance of ascites and pericardial effusion with no further tapping required. The patient was subsequently discharged and stent removed after 2months during which repeat pancreatogram was performed which showed no leak. Patient is in our follow up and is doing well.
Discussion
Pancreatic leak into the serosal cavity resulting in pleural effusion and ascites occurs in 3-5% of patients with chronic pancreatitis and 6-14% of patients with pancreatic pseudocyst[1].Postulated mechanisms in chronic pancreatitis are either due to pseudocyst communication with the serosal cavity or due to duct disruption. Pancreaticopleural and pancreaticopericardial fistulas are considered rare complications of chronic pancreatitis. The mechanism of pericardial effusion is not clear. Earlier it was believed to be due to pancreatic enzyme-induced chemical pericarditis and pleurisy. Cameron proposed that anterior duct disruption produces effusion and ascites whilst posterior duct dispurtion communicates retroperitoneally with the posterior mediastinum to produce pericardial effusion.[2]
The presenting symptoms can be variable depending on the location and size of the communication. Thus, patients may present with dyspnea, chest pain, palpitations, or cardiogenic shock. Our patient presented with progressive dyspnea and chest pain with intermittent abdominal pain.It was only when his pericardial effusion was analysed and found to have elevated amylase concentration, pancreatic origin was suspected.
Initial pericardial tapping, antibiotics, NJ feeding and octreotide followed by surgery in the form of lateral pancreaticojejunostomy has been considered the appropriate protocol.[3] Another report described an adult patient who underwent an elective Roux-en-Y pancreatico-jejunostomy without complication and remained symptom-free two years after the surgery.[4] In our case we have successfully managed the case with pancreatic endotherapy. To the best of our knowledge there are no published reports of successful endotherapy in pancreaticopericardial fistula. Even in recent case report pancreaticopericardial fistula did not respond to endotherapy.[5] The long term result of such management is not known and needs to be validated. The success of endotherapy depends on passing the guidewire across the leak, absence of tight strictures and deployment of appropriate length stent. We recommend ERCP and stenting in the initial management of such patients.
References
- Prakash K (2012). Pancreatic Ascites and Pleural Effusion, Pancreatitis - Treatment and Complications, Prof.Luis Rodrigo (Ed.), ISBN: 978-953-51-0109-3.
- Cameron JL. Chronic pancreatic ascites and pancreatic pleural effusions. Gastroenterology. 1978;74:134–40.
- Balasubramanian P, Jeyamani R, Govil S, Chacko A, Kurian G, Subhash HS,et al. Pancreatico-pericardial ûstula: a rare complication of chronic pancreatitis. Indian J Gastroenterol. 2004;23:31–2.
- Ching SS, Rao MM, Ali A, et al.: Chronic pancreatitis complicated by pancreaticopericardial fistula. Surgical Practice. 2007;11:130–3
- Sommer CA, Wilcox CM. Pancreatico-pericardial fistula as a complication of chronic pancreatitis. F1000 Res. 2014;3:31.
|