|
Jayant Kumar Ghosh1, Sundeep Kumar Goyal1, Manas Kumar Behera1, Manish Kumar Tripathi1, Vinod Kumar Dixit1, Ashok Kumar Jain1, Ramchandra Shukla2
Department of Gastroenterology1
and Radiodiagnosis2,
Institute of Medical Sciences,
Banaras Hindu University,
Varanasi - 221005,
India
Corresponding Author:
Dr. Jayant Kumar Ghosh
Email: drjayantkg@yahoo.co.uk
Abstract
Background: Amebic liver abscess (ALA) is a common and serious problem in our country. There are only a few controlled trials on the efficacy and advantages of combination therapy with percutaneous needle aspiration and pharmacotherapy, over pharmacotherapy alone for amebic liver abscess.
Material and Methods: This study was conducted to compare the efficacy of two different treatment modalities i.e. drug treatment alone vs. drug treatment and aspiration of abscess cavity in patients with small (up to 5 cm) and large (5 cm to 10 cm) size ALA. This is one of the largest single center, prospective, randomized studies comparing the efficacy of aspiration in ALA.
Results: (i) Mean body temperature, liver tenderness, total leukocyte count (TLC), serum alanine aminotransferase (ALT) and liver span were significantly decreased in the aspiration group on days 8 and 15 as compared to non-aspiration group especially in large abscess (5cm to 10 cm). (ii) Abscess cavity maximum diameter decreased significantly in aspiration group on days 8 and 15, and 1 month & 3 months in large abscess (5cm to 10 cm).
Conclusions: (i) Needle aspiration along with metronidazole hastens clinical improvement especially in large (5 cm up to 10 cm) cavities in patients with ALA. (ii) Aspiration is safe and no major complications occurred. (iii) Hence, combination therapy should be the first choice especially in large ALA (5 cm to 10 cm)
|
48uep6bbphidvals|1363 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Amebic liver abscess (ALA) is a common and serious problem encountered in our country. ALA is the most common extraintestinal manifestation of E. histolytica infection.[1]
Management of this disease includes the administration of anti-amebic drugs, e.g. metronidazole, and, occasionally, aspiration of the abscess cavity. The routine use of aspiration remains debatable and has generated considerable controversy amongst clinicians. There are only a few controlled trials on the efficacy and advantages of percutaneous needle aspiration over medical treatment only for amebic liver abscess.[2] This study was conducted to compare the efficacy of two different treatment modalities i.e. drug treatment alone vs. drug treatment plus aspiration of abscess cavity in patients with ALA among small (upto 5 cm) and large (5 cm to 10 cm) size ALA.
Material and methods
This was a prospective, randomized study performed at the Department of Gastroenterology, Sir Sunderlal Hospital Banaras Hindu University, Varanasi, from January 2012 to July 2013. This is one of the largest institutes in the Purvanchal (Eastern) region of North India catering to a population of almost 20 million.
The end-points were subsidence of fever and liver tenderness, normalization of total leukocyte count (TLC), alanine aminotransferase (ALT) and liver span. Intensity of liver tenderness (LT) was recorded as per the criteria suggested by Lamont and Pooler (1958).[3] These parameters were recorded on days 1, 8 and 15. Abscess cavity maximum diameter was recorded by ultrasonography (USG) on day 1, day 8, day 15, 1 month, and 3 months to look for radiological resolution of abscess. USG examination was done in the Department of Radiodiagnosis, Sir Sunderlal hospital, Banaras Hindu University, Varanasi by sector transducer 4 MHz and the abscess cavity was measured in two planes and the maximum diameter in any one plane was recorded. The study was performed after university ethics committee clearance. The diagnosis of ALA was made on the basis of Sherlock’s (1993) parameters.[4] ALA was confirmed by USG of liver as per Rall’s criteria 5 along with the demonstration of specific antiamebic antibodies in the serum by the ELISA method, antigen detection; and pus staining and pus culture. Antigen detection was done by TechLab E. histolytica II test developed and marketed by TechLab (Blacksburg VA 24060 U.S. only, 1-800- TECHLAB).[6] A total of 194 patients more than 18 years of age with a confirmed diagnosis of right liver lobe ALA were included in this study as per the criteria described above.
Exclusion criteria: i) Left lobe ALA, ii) Right lobe ALA with cavity diameter more than 10 cm, iii) Impending rupture, iv) Any complications i.e. rupture, sepsis, renal failure, v) Pregnant women, vi) Patients with prior anti-amebicidal treatment, and vii) Patients with primary or secondary immunodeficiency. Randomisation was done according to random number table.Group 1: Patients who had received drug treatment only (oral metronidazole; 800 mg t.i.d. X 14 days) (Non-aspiration group) (n=98) Group 2: Patients who had received combination therapy i.e. drug treatment (oral metronidazole; 800 mg t.i.d. X 14 days) AND aspiration of ALA (Aspiration group) (n=96) In Group 1, USG guided puncture with a fine lumbar puncture needle (23G) was performed to obtain a small quantity (3-5 mL) of abscess fluid for microbiological examination, culture and sensitivity. In Group 2, as much as possible, abscess fluid was aspirated by a large bore lumbar puncture needle (16G) under USG guidance.
Patients were further subdivided: Subgroup 1a: Nonaspiration group with abscess cavity maximum diameter up to 5 cm (n=51) ;Subgroup 1b: Non-aspiration group with abscess cavity maximum diameter was 5 cm and up to 10 cm (n=47) Subgroup 2a: Aspiration group with abscess cavity maximum diameter up to 5 cm (n=46); Subgroup 2b: Aspiration group with abscess cavity maximum diameter was 5 cm and up to 10 cm (n=50). None of the patients was admitted in the hospital for treatment of ALA.
Statistical analysis
Observations were recorded and analysis was done using SPSS v.16. Independent t-Test and paired t-Test were used for continuous variables. Chi square test and Fisher’s exact test were used for categorical variables. P-value <0.05 was considered as statistically significant.
Results
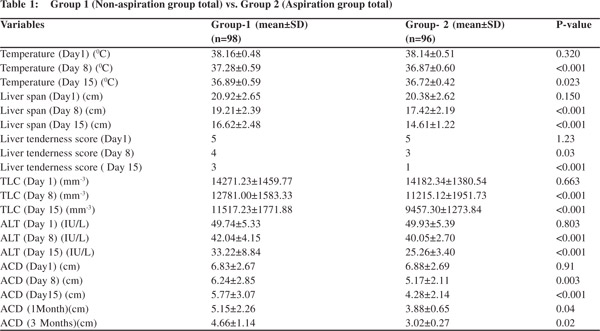
A) Group 1 ( Non-aspiration group total) vs. Group 2 (Aspiration group total) (Table-1) Mean body temperature, liver tenderness, total leukocyte count (TLC) , serum alanine aminotransferase (ALT) and liver span were significantly decreased in aspiration group (Group 2) on day 8 and day 15 as compared to non-aspiration group (Group 1). Abscess cavity maximum diameter decreased significantly in aspiration group on day 8, 15 and 1 month and 3 months. (B) Sub-group 1a (non-aspiration; abscess cavity maximum diameter up to 5 cm) vs. sub-group 2a (aspiration; abscess cavity maximum diameter up to 5cm) (Table-2)
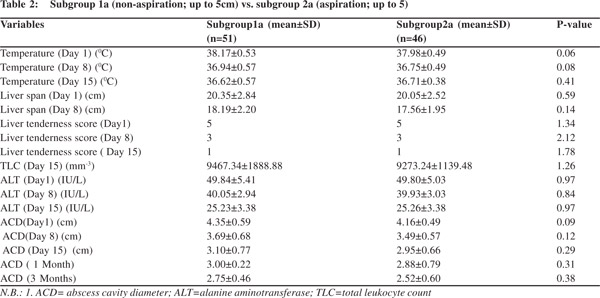
Mean body temperature, liver tenderness, TLC, ALT and liver span did not show any significant difference among the two sub-groups on day 8 and 15. Abscess cavity maximum diameter did not show any significant decrease among the two sub-groups on day 8, 15 and 1 month & 3 months. (C) Sub-group 1b (non-aspiration; abscess cavity maximum diameter 5 to 10cm) vs. sub-group 2b (aspiration; abscess cavity maximum diameter 5 to 10cm) (Table-3)
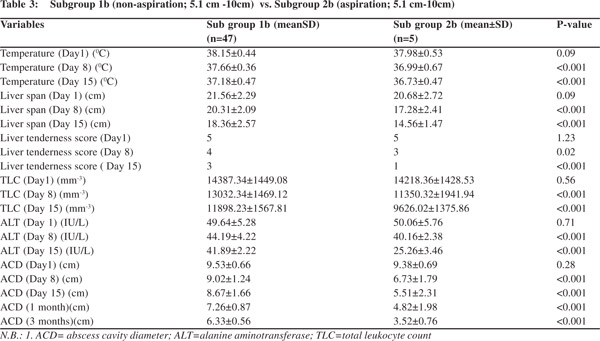
Mean body temperature, liver tenderness, TLC, ALT and liver span decreased significantly in Sub-group 2b on day 8 and 15. Abscess cavity maximum diameter decreased significantly in Sub-group 2b on day 8, 15 and 1 month and 3 months.
Complications
No major complications occurred in any patient.
Discussion
Amebic liver abscess (ALA) is frequently encountered in the tropics and is a major public health problem in our country.[7]
Most patients present acutely, with toxic features and large abscess cavities, many require hospitalization and emergency management. Treatment options for uncomplicated right lobe ALA are: i) pharmacotherapy with anti amebicidal agents like metronidazole, ii) combination therapy including both pharmacotherapy and aspiration, and iii) surgical.[8]
We found significant overall improvement in mean body temperature, liver tenderness, liver span, TLC, and ALT on days 8 and 15 in Groups 1 and 2. On sub-group analysis for smaller abscess (1a vs. 2a) none of the parameters showed any significant difference between the two sub-groups. However, in another sub-group analysis for larger abscess (1b vs.2b); it was found that body temperature , liver tenderness, liver span and normalisation of TLC and ALT were all significantly decreased in Sub-group 2b on day 8 and 15. Abscess cavity maximum diameter decreased significantly in Sub-group 2b on day 8,15 and 1 month & 3 months.
In a recent Cochrane review published in 2009, in which seven low quality randomized trials were included, authors concluded that therapeutic aspiration in addition to metronidazole to hasten clinical or radiologic resolution of uncomplicated ALA can’t be supported or refuted by the present evidence.[2] Van Allan et al (1992) undertook a prospective randomized trial in 41 patients of ALA to test the potential benefit of therapeutic aspiration.[9] The authors observed a marginal reduction in levels of subjective pain and tenderness following therapeutic aspiration . However, Van Allan et al (1992) did not find any significant difference in body temperature reduction in the two groups. Sharma et al (1989) also did not find any significant difference in pain and fever in the two groups on days 8 and 15.10 Sharma et al 1989; and Tandon et al 1997 reported normalisation of liver span on days 8 and 15 in the aspiration group.[10,11] Sharma et al 1989 found that chemotherapy alone was as effective as routine needle aspiration and concluded that chemotherapy alone should be the preferred mode of therapy for ALA.10 However, Ramani et al reported more rapid clinical response in the aspirated group, particularly in uncomplicated ALA with larger (>6cm) abscess cavities.[12]
Freeman et al (1990) conducted a study in 36 patients to study the effect of percutaneous needle aspiration on healing or resolution time.[13] Their results were similar to our observations in that the authors had demonstrated a more rapid clinical response in the aspirated group, particularly for patients with lesion size > 6cm. We also found faster USG resolution of abscess cavity in the aspiration group especially in large abscesses (diameter 5 cm up to 10 cm). Ralls et al (1983) had shown lack of correlation in clinical improvement with ultrasonographic resolution.[14] Changes in lesion size or characteristics was clinically irrelevant as many asymptomatic successfully treated patients had lesions that had increased in size on follow-up scans.[15] We also found radiologically detectable abscess cavities through 1 month and 3 months but clinically improved patients. Thus, it is indeed difficult to correlate clinical recovery with ultrasonographic resolution of amebic liver abscess[15]. Needle aspiration was determined safe in our study which corroborates with the work of previous authors.[11,13]
The strengths of this study are : a) one of the largest RCTs on the efficacy of aspiration in ALA , b) First of its kind which did sub-group analyses among small and large abscess cavities and pharmacotherapy and combination therapy simultaneously in a single study.
In summary, needle aspiration along with metronidazole hastens clinical improvement especially in large (5 cm to 10 cm) abscesses in patients with ALA. Needle aspiration is safe and no major complications occurred. Hence, combination therapy should be the first choice especially in large ALA (5 cm to 10cm).
References
- Sharon LR. Amoebiasis and infections with free living amoebas. In Harrison’s Principles of Internal Medicine. Fauci AS, Braunwald E et al (eds.0.14th edition, McGraw Hill Companies Inc. USA 1998;1176–80.
- Chavez-Tapia NC, Hernandez-Calleros J, Tellez-Avila FI, Torre A, Uribe M. Image-guided percutaneous procedure plus metronidazole versus metronidazole alone for uncomplicated amoebic liver abscess (Review). Copyright © 2009 The CochraneCollaboration. Published by JohnWiley & Sons, Ltd.
- Lamont NM,Pooler NR. Hepatic amoebiasis. Quart J Med. 1958;27:389–412.
- Sherlock S, Dooley J. Liver infection. In: Diseases of liver and biliary system. 9th ed. London Blackwell 1993; 471–477.
- Ralls PW, Barnes PF, Radin DR, Colletti P, Halls J. Sonographic features of amebic and pyogenic liver abscesses: a blinded comparison. AJR Am J Roentgenol. 1987;149:499–501.
- Haque R, Mollah NU, Md. Ali IK, Alam K, Eubanks A, Lyerly D, et al. Diagnosis of Amebic Liver Abscess and Intestinal Infection with the TechLab Entamoeba histolytica II Antigen Detection and Antibody Tests. J Clin Microbiol. 2000;38:3235–9.
- Sharma MP,Ahuja V. Amoebic Liver Abscess. JIACM. 2003;4:107–11.
- Sharma MP, Ahuja V. Management of amoebic liver abscess. Arch Med Res. 2000;31:S4–5.
- Van Allan RJ, Katz MD, Johnson MB, Laine LA, Rails PW. Uncomplicated Amebic liver abscess: prospective evaluation of percutaneous therapeutic aspiration. Radiology. 1992;183:827–30.
- Sharma MP, Rai RR, Acharya SK, Samant Ray JC, Tandon BN, Needle aspiration of amoebic liver abscess. Br Med J. 1989;299:1308–9.
- Tandon A, Jain AK, Dixit VK, Agarwal AK, Gupta JP. Needle aspiration in large amoebic liver abscess. Trop Gastroenterol. 1997;18:19–21.
- Ramani A, Ramani R, Kumar MS, Lakhkar BN, Kundaje GN. Ultrasound guided needle aspiration of amoebic liver abscess. Postgrad Med J. 1993;69:381–3.
- Freeman O, Akamaquna A, Jarikre LN. Amoebic liver abscess: the effect of aspiration on the resolution or healing time. Ann Trop Med Parasitol. 1990;84:281–7.
- Ralls PW, Colletti PM, Quinn MF, Halls J. Sonographic findings in hepatic amoebic abscess. Radiology. 1982;145:123–6.
- Sharma MP, Dasarathy S, Verma N, Saksena S. Long term follow up of amoebic liver abscess: clinical and ultrasound patterns of resolution. Trop Gastroenterol. 1995;16:24–8.
|