Rachel M. Gomes, couponrxsms.com discount Nilesh H. Doctor
Department of Surgical Gastroenterology,
Jaslok Hospital and Research Centre,
Mumbai, India
Corresponding Author:
Dr. Nilesh Doctor
Email: drnileshbela@gmail.com
Abstract
Introduction: Reconstructive hepatico-jejunostomy is recommended for major bile duct injuries (BDIs) during cholecystectomy. Complications of biliary leak, cholangitis, bleeding, anastomotic strictures and biliary cirrhosis remain a major concern affecting a patient’s outcome after surgery. The aim of this study was to analyse the results of surgical repair of major BDIs at our institution and identify predictors for the development of major complications.
Methods: A retrospective study of 57 patients with major BDI after cholecystectomy referred to a tertiary hepato-biliary centre from July 1999 to July 2011 and subsequently managed with reconstructive bilio-enteric anastomosis was performed.
Results: Of 57 patents 35 (61.4 %) were primary referred. 22 (38.6 %) were secondary referred, of which 17 were for correct reconstructive surgery performed elsewhere and 5 were following attempted endoscopic management. 17 (29.8 %) had local and systemic perioperative complications. 13 (22.8%) had major complications (bile leak, bleed, stricture and/or biliary cirrhosis). No association was found between age, type of cholecystectomy, type of injury, vascular injury and occurrence of major complications. Secondarily referred patients after therapeutic interventions (p=0.010) and reconstructive surgery after repair performed by nonspecialists suffered an increased incidence of major complications (p=0.032). Secondary referral was also an independent predictor of major complications (p=0.024).
Conclusion: Early referral of patients with no previous intervention to a tertiary hepato-biliary center and specialist surgical repair is recommended for improved outcome after reconstructive hepatico-jejunostomy for major BDIs during cholecystectomy.
|
48uep6bbphidvals|1360 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Managing BDI after cholecystectomy continues to be a major challenge and requires a multi disciplinary approach between surgeons, gastroenterologists and radiologists. The recommended treatment for major bile duct injury (BDI) after cholecystectomy is hepatico-jejunostomy performed between the confluence of bile ducts and a Roux loop of intestine. Surgical repair of BDI has slowly evolved over time and remains technically challenging even for the experienced surgeon. It has associated morbidity affecting a patient’s short and long term outcomes. This morbidity includes lifethreatening complications of biliary leak, sepsis, cholangitis, bleeding, anastomotic strictures and biliary cirrhosis with portal hypertension and end-stage liver disease. Numerous factors influence the results of treatment.
The aim of this study was to analyse the outcome after surgical repair of major BDIs at our institution and identify predictors for the development of major complications.
Patients and methods
Study Population
A retrospective analysis of a prospective database of all patients referred with a major BDI following cholecystectomy and treated surgically by the senior author at the Jaslok Hospital and Research center during a 12 year period from July 1999 to July 2011 was performed.
Major BDI included all transections or partial lacerations of the common hepatic duct, common bile duct, or major segmental ducts at the portahepatis.
Minor leaks from the cystic duct or gallbladder bed were excluded. Patients with benign bile duct strictures from trauma or inflammatory processes and malignant bile duct strictures were excluded.
The type of BDI was defined by imaging (computed tomography (CT) with vascular reconstruction, magnetic resonance cholangio-pancreatography (MRCP), endoscopic retrograde cholangio-pancreatography (ERCP), percutaneous transhepatic cholangiography (PTC)) and surgical recognition.
BDIs were then categorized according to the Strasberg classification. Presence of vascular injury was recorded. Based on the therapeutic interventions attempted at the referring center two groups were defined. Primary referred patients were defined as those who had not undergone any therapeutic intervention at the referring center. Secondary referred patients presented following surgical, endoscopic or radiologic interventions. Based on the timing and type of surgery three operative groups were defined. Early primary repair consisted of patients with no prior surgical intervention operated within 3 weeks of the injury and late primary repair consisted of patients with no prior surgical intervention operated following 3 weeks of the injury. Delayed secondary repair were patients who were referred for reconstructive surgery for correction of intended final reconstructive surgical repair performed elsewhere. Complications within 30 days of procedure were defined as short-term complications and after this as long-term complications. Complications specific for hepatico-jejunostomy were defined as minor (e.g. abscesses, wound infection and cholangitis) and major (anastomotic leakage, postoperative bleeding, anastomotic strictures or biliary cirrhosis).
Surgical management consisted of a Roux-en-Y hepaticojejunostomy.
The biliary reconstruction of transected bile ducts (type E injuries) was performed by an end-to-side Roux-en-Y hepatico-jejunostomy according to the Hepp–Couinaud technique. A Roux-en-Y loop of at least 40 cm length was used carefully, avoiding tension at the anastomosis. After excision of any scar tissue, a mucosa-to-mucosa one-layer anastomosis was created with absorbable 4-0 suture PDS using the interrupted technique. The anastomosis was always done at the confluence of the two ducts and after opening the entire extent of the horizontal length of the left hepatic duct. The hilar plate was lowered to facilitate this step. This ensured a wide anastomosis even when the duct was small and non-dilated. The posterior row of sutures was placed first and tied only after all had been placed. This helped to ensure deep accurate placement as the intestine and the bile duct remained far apart. The anterior row was similarly placed. Trans-hepatic stents were placed only in selected cases. Drains to the anastomosis were placed routinely.
After discharge, patients were followed with regular liver function tests and ultrasound scan of the biliary tree. This was done annually in patients who remained asymptomatic. Further imaging was done when biochemistry was abnormal or patients developed symptoms of cholangitis.
Demographics, prior intervention, preoperative imaging, Strasberg’s classification of BDI, presence of vascular injury, type and timing of surgical reconstruction, short-term and long-term complications and mortality were analysed.
Data analysis
Univariate analysis was performed using the Chi square test (when appropriate the Fischer test) for the presence of risk factors for the occurrence of major complications. Multivariate analysis was performed using binary logistic regression to look for independent association of risk factors detected on univariate analysis. P values of <0.05 were considered statistically significant. Statistical analysis was performed using SPSS v.20.0 (Chicago, IL, USA) software for Windows.
Results
Study population
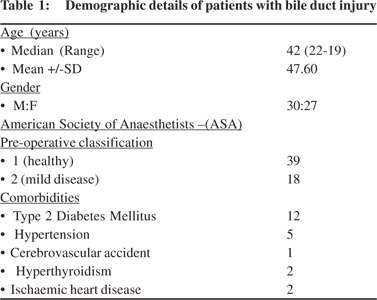
The study population comprised of 57 referred patients, 30 men (52.6 %) and 27 women (47.4 %) with a median age of 42 years (range, 22 to 79 years), treated surgically for major BDIs after cholecystectomy during a 12-year period. 39 patients were of ASA class 1,18 patients were of ASA class 2 with none of ASA class 3 or 4. 12 patients had diabetes mellitus, 5 had hypertension, 1 had an old cerebrovascular accident, 2 had hyperthyroidism and 2 had ischemic heart disease. Patient demographics are listed in Table 1.
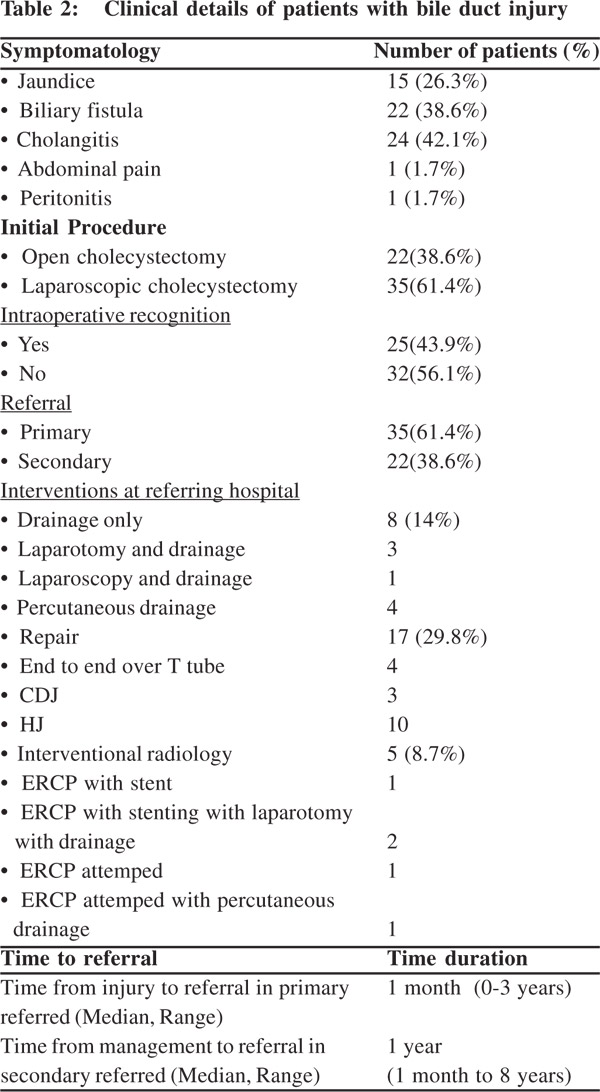
Patient clinical details and type of injury are listed in Tables 2 and 3 respectively.
Initial procedure and recognition of bile duct injuries
Of the 57 cases an open cholecystectomy was performed in 22 and a laparoscopic cholecystectomy in 35. The injury was recognized intra-operatively at the index surgery by the primary surgeon in 25 cases (43.9 %). At referral, 15 patients presented with jaundice, 22 with a biliary fistula, 24 with cholangitis, 1 with abdominal pain and 1 with peritonitis.
Referral of patients and interventions performed
Of 57 patients 35 (61.4 %) were primary referrals. Of these in 8 patients with a biliary leak only drainage with no attempt toward reconstruction was performed. 3 were laparotomy with drainage, 1 was a laparoscopy with drainage and 4 were percutaneous drainage. In primary referrals the median time from injury to referral was 1 month (range 0-3 years). 22 (38.6 %) were secondary referrals, of which 17 were to correct reconstructive surgery performed elsewhere and 5 were after prior attempted endoscopic management. Of the 17 repairs 4 were end-to-end ductal anastomosis over a T tube, 3 were choledocho-jejunostomies and 10 were hepaticojejunostomies.
Of 5 patients with endoscopic intervention three had an ERCP with stenting, of which two still needed a laparotomy with drainage for biliary leak. Two had unsuccessful attempts at ERCP with stenting of which one needed percutaneous drainage. In secondary referred the median time from intervention to referral was 1 year (Range: 1 month to 8 years).
Bile Duct Injuries According to the Strasberg classification
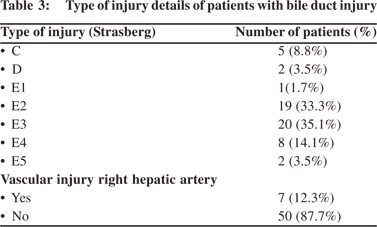
According to Strasberg’s classification of bile duct injuries there were 5 patients with a Type C, 2 with type D ,1 with Type E1, 19 with type E2 , 20 with Type E3 , 8 with type E4 and 2 with type E5. 7 patients were identified to have concomitant right hepatic artery injury.
Hospital stay
The median length of stay after definitive repair was 12 days (Range 7-31 days).
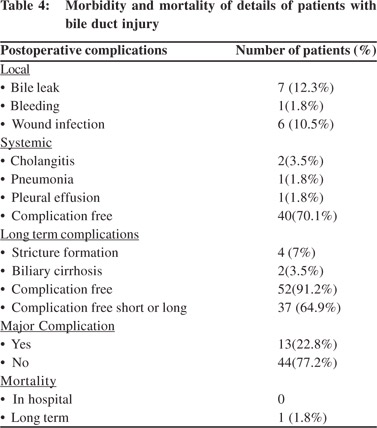
Patient morbidity and mortality details are listed in Table 4.
Short-term complications and mortality
Of the 57 patients who underwent biliary reconstruction, no deaths occurred in the postoperative period. Of the patients with local complications 7 patients had a bile leak postoperatively which was managed conservatively in all cases. 1 patient had bleeding from a pseudo-aneurysm of the right hepatic artery managed by angio-embolization and 8 patients had wound infection. Of patients with systemic complications 2 patients hadcholangitis, 1 patient developed pleural effusion and 1 patient developed pneumonia. 40 patients remained free of local or systemic complications.
Long-term complications and mortality
Follow-up ranged from 36 to 120 months (median, 84 months) as of July 2014. All patients, barring one were alive by July 2014. This death occurred because of liver failure secondary to biliary cirrhosis.[5] patients developed an anastomotic stricture needing dilatation and 2 developed biliary cirrhosis. 52 patients had no late complications.
Analysis of risk factors for the occurrence of major complications after BDI repair
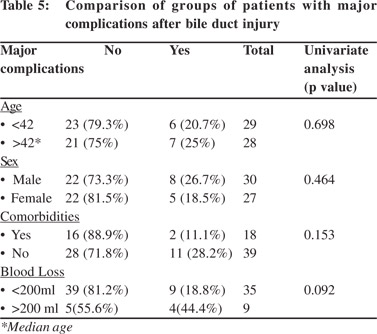
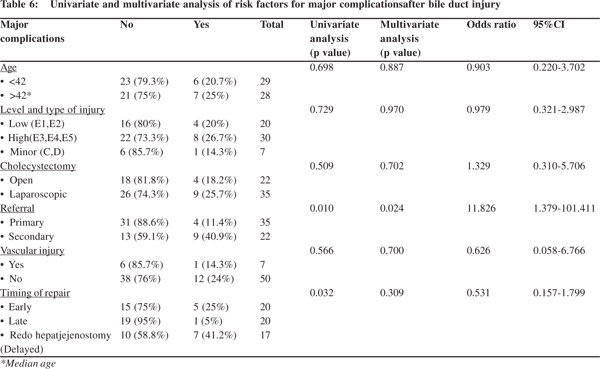
Comparison details are listed in Tables 5 and 6.13 patients (22.8%) had major short or long term complications (bile leak, bleed, stricture and/or biliary cirrhosis). The two groups with and without major complications were similar in age, sex, ASA status, presence of comorbidities and blood loss during surgery. No association was found between age, type of cholecystectomy, type of injury, vascular injury and occurrence of major complications. Secondary referred patients after therapeutic interventions (p=0.010) and reconstructive surgery for intended final reconstructive repair performed elsewhere (p=0.032) were associated with a significantly increased incidence of major complications. Secondary referral was also an independent predictor of major complications (p=0.024).
Discussion
BDI following cholecystectomy still remains a major challenge. Severe injuries such as bile duct transection or recurrent strictures need reconstructive surgery. Surgical repair can be complicated by biliary leak, sepsis, cholangitis, bleeding, anastomotic strictures and biliary cirrhosis with portal hypertension and end-stage liver disease. BDIs may hence lead to prolonged morbidity, high costs, and an impaired quality of life.[1–3] An optimization of the management strategy can reduce these complications.
This article describes a consecutive series of 57 patients undergoing reconstructive surgery for bile duct injury operated at our institution over 12 years. In this series, 13 (22.8%) patients had 1 or more major complication (bile leak, bleed, stricture and/or biliary cirrhosis) affecting the short and/or long outcome. We analysed possible predictors influencing the occurrence of major complications in this study. The index cholecystectomy was performed by the open technique in 22 patients and laparoscopically in 35 patients.
As the incidence of BDIs is higher in laparoscopic cholecystectomy (0.1-0.2% vs. 0.4 -0.6%) and tends to be more severe the technique of index cholecystectomy may indirectly affect the outcome after surgical repair in these patients.[4,5] Series reporting long term results after BDI repair following open cholecystectomy have shown similar results to those after laparoscopic cholecystectomy.[6–9] We did not observe any effect of cholecystectomy technique affecting outcome in this study.
There were 22 patients above the age of 42 years. Older age was not associated with occurrence of major complications after surgical repair as noted in a few studies.[10] However it has been reported that even with successful management, quality of life is decreased and survival impaired, especially in elderly patients.[11]
The injury was recognized intra-operatively in 25 cases (43.9 %) similar to other studies where the majority of biliary injuries are not recognized during the initial cholecystectomy.[9] After diagnosing injury, 22 of 57 (38.6 %) were referred following prior surgical or endoscopic intervention to correct the injury.
These patients had a significantly higher incidence of major complications following reconstructive surgery in comparison to those directly referred without any intervention. Also on analysis this was found to be the only independent predictor of the occurrence of major complications. These findings are similar to other studies that show that the outcome for reconstructive surgery in a specialized center is influenced by the referral pattern.[12]
In the major BDIs, a Roux-en-Y hepatico-jejunostomy (HJ) is the preferred method of repair as was performed in all patients in this study. Repair in the presence of peritonitis is associated with poor outcome.[13] Our practice was to initially control sepsis via radiologic intervention or laparotomy/laparoscopy and antibiotics and operate on patients at a later date (4-6 weeks), after their index admission when the associated collections and inflammation had subsided. The optimal timing of surgical repair remains controversial. Early surgical reconstruction performed several days to within 3 weeks after injury, on nondilated bile ducts and inflamed tissues is thought more difficult with poorer short and long-term outcomes. However many authors have failed to identify early repair as an individual risk factor.[12,14,15] In this series, early repair within 3 weeks was associated with the lowest incidence of major complications, as reported in some other series also.[16] Patients with late repairs and repeat surgeries were associated with significantly higher incidence of major complications though timing of repair was not an independent predictor of outcome.
17 patients in this series were reoperated for failed repairs previously performed by a non specialist. Reports suggest that upto 75% of primary surgeons attempt to repair the injury themselves.[2] Prior reconstructive surgery by the initial surgeon was found to be associated with an increased incidence of complications though it was not found to be an independent predictor in our series. Stewart and Way showed that the outcome of a surgical repair after BDI is successful in 94% of the patients if performed in a specialized center, whereas only 17% are successful when operated on by the initial surgeon.[17] A multicenter report by Woods et al, reported a similar rate of failure (94%) following repair prior to specialist referral.[18] Also, the number of attempted repairs before referral was a significant predictor of poor outcome.[19]
Other prognostic factors for successful repair of iatrogenic BDI include the level of injury and absence of injury to the right hepatic artery. It has long been recognized that higher the location of injury or stricture, the more difficult is the repair and the greater is the recurrence rate.[12,13] Though we did not observe an association between level of injury and outcome, the relatively small number of patients within each injury sub-type makes it difficult to compare.
The right hepatic artery lies behind the common hepatic duct at the usual level of transection, and is vulnerable to injury. The outcome in patients with major bile duct injuries combined with arterial disruptions is considered worse than in patients with an intact blood supply of the bile ducts.[13]
There was no increase in complication rate seen in this series in patients with right hepatic artery injury. Stewart et al reported that biliary injuries repaired by the primary surgeon are associated with a higher incidence of postoperative abscess bleeding, hemobilia, hepatic ischemia, and the need for hepatic resection but a similar increase in the complication rate was not seen in patients treated by hepato-biliary surgeons.[20]
In conclusion, referral to a tertiary centre after therapeutic interventions was an independent negative predictor of outcome. Reconstructive surgery after repair performed by nonspecialists had a worse outcome. Our findings thus support early referral of patients to a tertiary hepato-biliary center after bile duct injury without intervention and specialist surgical repair.
References
- Kaman L, Behera A, Singh R, Katariya RN. Management of major bile duct injuries after laparoscopic cholecystectomy. Surg Endosc. 2004;18:1196–9.
- Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290:2168–73.
- Boerma D, Rauws EA, Keulemans YC, Bergman JJ, Obertop H, Huibregtse K, et al. Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: a prospective analysis. Ann Surg. 2001;234:750–7.
- Roslyn JJ, Binns GS, Hughes EF, Saunders-Kirkwood K, Zinner MJ, Cates JA. Open cholecystectomy. A contemporary analysis of 42,474 patients. Ann Surg. 1993;218:129–37.
- Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–25.
- Csendes A, Diaz C, Burdiles P, Nava O, Yarmuch J, Maluenda F, et al. Indications and results of hepaticojejunostomy in benign strictures of the biliary tract. Hepatogastroenterology. 1992;39:333–6.
- Sutherland F, Launois B, Stanescu M, Campion JP, Spiliopoulos Y, Stasik C. A refined approach to the repair of postcholecystectomy bile duct strictures. Arch Surg Chic Ill 1960. 1999;134:299–302.
- Tocchi A, Costa G, Lepre L, Liotta G, Mazzoni G, Sita A. The long-term outcome of hepaticojejunostomy in the treatment of benign bile duct strictures. Ann Surg. 1996;224:162–7.
- Lillemoe KD, Martin SA, Cameron JL, Yeo CJ, Talamini MA, Kaushal S, et al. Major bile duct injuries during laparoscopic cholecystectomy. Follow-up after combined surgical and radiologic management. Ann Surg. 1997;225:459–68.
- Fullum TM, Downing SR, Ortega G, Chang DC, Oyetunji TA, Van Kirk K, et al. Is laparoscopy a risk factor for bile duct injury during cholecystectomy? JSLS J Soc Laparoendosc Surg Soc Laparoendosc Surg. 2013;17:365–70.
- Moore DE, Feurer ID, Holzman MD, Wudel LJ, Strickland C, Gorden DL, et al. Long-term detrimental effect of bile duct injury on health-related quality of life. Arch Surg. 2004;139:476–82.
- De Reuver PR, Grossmann I, Busch OR, Obertop H, van Gulik TM, Gouma DJ. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Ann Surg. 2007;245:763–70.
- Schmidt SC, Langrehr JM, Hintze RE, Neuhaus P. Long-term results and risk factors influencing outcome of major bile duct injuries following cholecystectomy. Br J Surg. 2005;92:76–82.
- Thomson BNJ, Parks RW, Madhavan KK, Wigmore SJ, Garden OJ. Early specialist repair of biliary injury. Br J Surg. 2006;93:216–20.
- Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005;241:786–792.
- Perera MTPR, Silva MA, Hegab B, Muralidharan V, Bramhall SR, Mayer AD, et al. Specialist early and immediate repair of post-laparoscopic cholecystectomy bile duct injuries is associated with an improved long-term outcome. Ann Surg. 2011;253:553–60.
- Stewart L, Way LW. Bile duct injuries during laparoscopic cholecystectomy. Factors that influence the results of treatment. Arch Surg Chic Ill 1960. 1995;130:1123–9.
- Woods MS, Traverso LW, Kozarek RA, Tsao J, Rossi RL, Gough D, et al. Characteristics of biliary tract complications during laparoscopic cholecystectomy: a multi-institutional study. Am J Surg. 1994;167:27–34.
- Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stricture. Patterns of recurrence and outcome of surgical therapy. Am J Surg. 1984;147:175–80.
- Stewart L, Robinson TN, Lee CM, Liu K, Whang K, Way LW. Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2004;8:523–30.
|