Intestinal obstruction is one of the most common surgical emergencies, with various underlying causes, of which internal hernias account for 0.6% to 5.8% of small bowel obstructions1. Internal hernia is the protrusion of viscus through an intraabdominal aperture without traversing the fascial planes. Internal hernia could be a congenital or acquired type. Congenital internal hernia, though named congenital, has an average age of presentation of 30-50 years, and the mean age is 38.5 years. Para-duodenal hernias account for 50% of all congenital hernias, of which left para-duodenal hernias are more common (70% of all para-duodenal hernias)1. Typically, patients with para-duodenal hernias present with symptoms of intestinal obstruction and have a history of intermittent obstruction and associated vague abdominal pain2. The malrotation of the midgut and failure of fusion of mesentery to parietal peritoneum create a hernial defect. Para-duodenal hernia can lead to bowel obstruction, ischemia, and perforation and has a high mortality rate of 30-50%.4
Herein, we report a case series of three patients with left para-duodenal hernias, all presenting as intestinal obstruction with bowel ischemia.
Case Series
Case 1
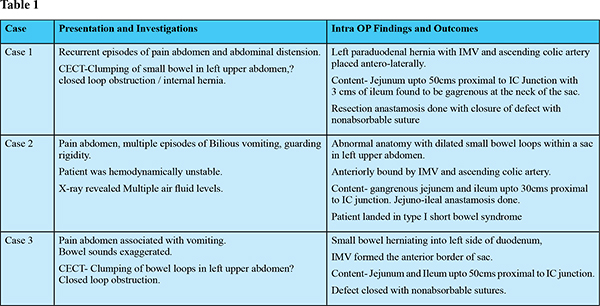
A 35-year-old male presented to casualty with symptoms of abdominal pain, distension, constipation, and obstipation for 3 days. There was history of similar episodes in the past for which he was hospitalized once. The patient was conscious and oriented. His pulse rate was 97/min, blood pressure was 130/70 mmHg, and SpO2 was 98% on room air. Abdominal examination revealed diffuse tenderness all over the abdomen and distension. Bowel sounds were sluggish. Ultrasound abdomen and pelvis revealed dilated bowel loops with sluggish peristalsis. Contrast Enhanced CT scan revealed clumping of the small bowel loops over left upper abdomen and closed loop obstruction, likely internal hernia (para-duodenal hernia) (Figure 1,2). The patient was taken up for exploratory laparotomy. The intraoperative findings were a hernial sac with inferior mesenteric vein (IMV) and ascending left colic artery placed anterio-lateral to the sac. The afferent limb of the hernia was 4th part of the duodenum, and the efferent limb was the terminal ileum. The neck of the sac was narrow, causing obstruction and gangrene of ileum, which was about 50 cm proximal to the ileo-cecal junction, and the gangrenous bowel was 3 cm in length. The gangrenous bowel was resected, and end to end anastomosis was done (Figure 3).
The mesenteric defect was closed with a non-absorbable suture to prevent further herniation. The post-operative period was uneventful, and the patient is on follow-up.
Case 2
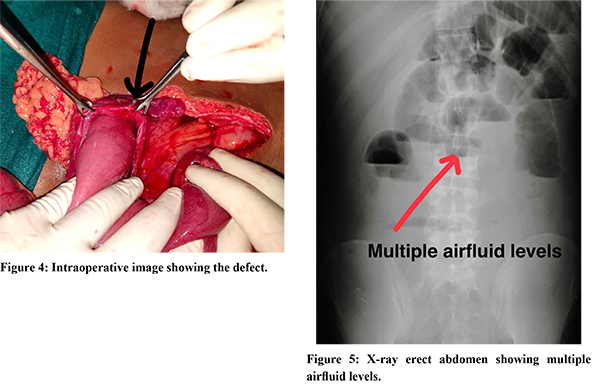
A 15-year-old male presented to the casualty with symptoms of abdominal pain, constipation, obstipation and bilious vomiting for 5-6 episodes over 4 days. On examination, patient was conscious and oriented. His pulse rate was 120/min, blood pressure was 90/60 mmHg and SpO2 was 94% on room air. Abdominal examination revealed distension, diffuse tenderness, guarding, and rigidity. Bowel sounds were absent. Despite adequate resuscitation, vital signs did not improve. He was started on inotropic support. His routine investigations revealed a total leucocyte count of 35,000 cells/mm3, hemoglobin of 10 g/dL, and hypokalemia (3.0 mEq/dL). X-Ray erect abdomen and pelvis revealed multiple air-fluid levels and clumping of bowel loops in the left upper quadrant. Ultrasound abdomen showed diffuse distension with sluggish peristalsis. The patient was taken up for an emergency exploratory laparotomy. Intraoperative findings revealed dilated loops of small bowel within a hernial sac in the left upper abdomen. The hernia appeared to protrude through the mesentery of the large bowel and incorporated a large segment of bowel from the duodenum to 40 cm proximal to ileo-cecal junction (Figure 4,5). The sac was opened near the neck to reduce the contents, and the small intestine was found to be gangrenous, 200 cm proximal to ileo-cecal junction.Around 150 cm of small bowel was gangrenous, which was resected, and ileo-ileal anastomosis was done. The mesenteric defect was closed to prevent further recurrences. The postoperative period was uneventful; the patient was discharged and is doing well.
Case 3
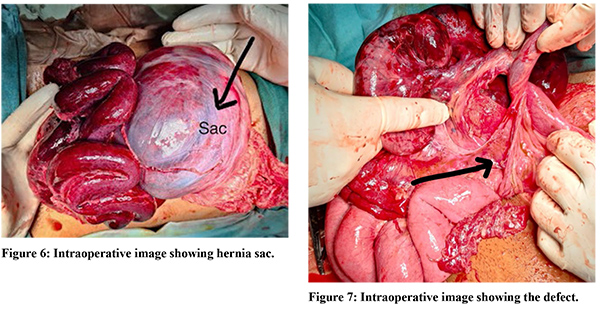
A 25-year-old female patient presented to the casualty with complaints of pain abdomen, associated with nausea and bilious vomiting (3 episodes) for 2 days. History of similar complaints of vague abdominal pain was present. On examination, the patient was conscious-oriented, febrile, and had pulse rate of 110/min, blood pressure of 90/65mmHg and SpO2 of 96% on room air. Abdominal examination revealed diffuse tenderness, guarding, and rigidity. Bowel sounds were exaggerated. Patient was resuscitated adequately with intravenous fluids. Routine blood investigations showed hemoglobin of 10 g/dL and total leucocyte count of 15,000 cells/mm3. X-Ray erect abdomen and ultrasound were inconclusive; hence, a contrast-enhanced CT scan was done, which revealed a left-sided clumping of small intestine with distorted vascular anatomy likely a closed-loop obstruction or para-duodenal hernia. An exploratory laparotomy was planned, and intraoperative findings revealed a hernial sac on left upper abdomen, displacing the IMV, and left colic artery anterolaterally. The neck of the sac was identified, and the contents, which started proximally at jejunum and extended distally up to terminal ileum, were reduced,. About 50 cm of bowel was gangrenous, 100 cm proximal to the ileo-cecal junction. Resection and anastomosis was done. The mesenteric defect was closed.The postoperative period was uneventful, and the patient was discharged (Figure 6,7; Table 1).
Discussion
Para-duodenal hernia, also known as mesocolic hernia, occurs due to embryonal peritoneal anomalies and associated abnormal intestinal rotation4. Typically, patients present with symptoms of vague abdominal pain with or without symptoms of obstruction. Left para-duodenal hernia occurs due to the herniation of intestinal loops into a potential space known as the Landzert Fossa, which failed to obliterate. The left para-duodenal hernia is posterior to the inferior mesenteric vein and left branch of the middle colic artery and is situated to the left of fourth part of the duodenum. It occurs in 2% of the population3. The small bowel becomes entrapped between the mesocolon and the posterior abdominal wall, forming the anterior wall of the hernia sac6. It is a rare condition, and to establish the diagnosis, an experienced radiologist, anda high index of suspicion is required. About 50% patients are associated with a lifetime risk of obstruction and strangulation.
High rate of mortality necessitates early diagnosis and precise surgical management. The surgical intervention involves identification of the hernial sac and the defect, reduction of the contents, checking for the viability of the bowel, and avoiding injury to the vasculature. A downward incision of the ring will avoid injury to the inferior mesenteric vein. Awareness of the vascular anterior border of the aperture during repair is imperative. The defect should always be closed either continuously or in an interrupted manner, preferably using non-absorbable sutures. Surgical aspects include timely intervention, as the outcome largely depends on appropriate management at the right time. All our cases underwent exploratory laparotomy. The postoperative period was uneventful, and all the cases were discharged without further complications.
References
- Yeo, Charles J, David W. McFadden, Steven R. DeMeester, Jeffrey B. Matthews, James W. Fleshman. Shackelford’s surgery of the alimentary tract,8th ed. Philadelphia, PA : Elsevier, [2019].
- Takeyama N, et al. CT of internal hernias. Radiographics. 2005;25(4):997.
- Husain A, et al. Internal Hernia through Paraduodenal Recess with Acute Intestinal Obstruction: A Case Report. Indian J Surg. 2012;74(4):354–5.
- Shadhu, K., Ramlagun, D. & Ping, X. Para-duodenal hernia: a report of five cases and review of literature. BMC Surg 18, 32 (2018).
- Al-Khyatt W, et al. Acute intestinal obstruction secondary to left paraduodenal hernia: a case report and literature review. World J Emerg Surg Wjes. 2013;8(1):1–5
- Bartlett, Marshall K. M.D.; Wang, Chiu-an M.D.; Williams, Willis H. M.D.. The Surgical Management of Paraduodenal Hernia. Ann Surg. 168(2):p 249-254, August 1968.