48uep6bbphidcol2|ID
48uep6bbphidvals|3056
48uep6bbph|2000F98CTab_Articles|Fulltext
Endoscopic retrograde cholangiopancreatography (ERCP) is commonly performed minimally invasive therapeutic procedure for pancreaticobiliary disorders.1 Even though considered as relatively safe procedure, ERCP is associated with high potential complications requiring prolonged hospital stay, invasive intervention, morbidity and risk of mortality.
Risk of complications associated with ERCP ranges from 3-10% with mortality risk of 0.33% and commonly reported complications are post-ERCP pancreatitis, bleeding, perforation, infection and sedation related events.2 Less common complication like hepatic hematoma have been reported as case reports and its true incidence is not known.3 Hepatic hematoma even though rare, carries significant morbidity and mortality risk of around 10%.4 We report a case of hepatic sub capsular and parenchymal hematoma, developed post ERCP for choledocholithiasis, which was successfully managed conservatively without any complications.
Case Report
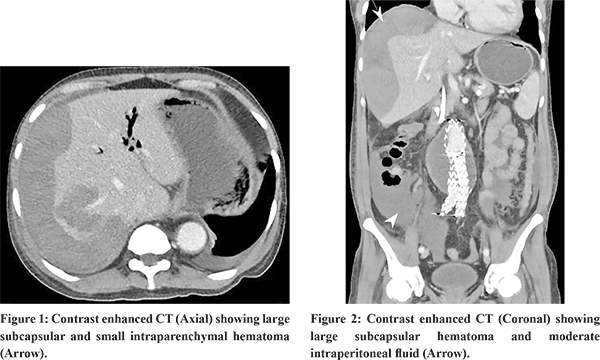
68 year old male, known case of abdominal aortic aneurysm, post aortic stenting in 2016, ischemic heart disease, post percutaneous transluminal coronary angioplasty (PTCA) in 2019, diagnosed as acute calculous cholecystitis in 2019 planned for interval cholecystectomy but deferred due to poor cardiac function, presented with history of sudden onset of upper abdominal pain worsening with food intake for 2 days. On examination, he was hemodynamically stable, febrile and had mild tenderness in epigastric and right hypochondrium. On evaluation his hemogram showed mild leucocytosis, normal hematocrit. His liver function tests showed alanine transaminase (ALT) 311.0 IU/L, aspartate transaminase (AST) 625 IU/L, alkaline phosphatase (ALP) 352IU/ml and serum bilirubin 2.7 mg/dl. His serum amylase level was 1061 U/ml and serum lipase was >300 U/L and renal function tests were normal. His ultrasound abdomen showed cholecystolithiasis with normal proximal bile duct and lower bile duct obscured by bowel gas. In view of clinical suspicion of biliary pancreatitis, MRCP was done which showed cholecystolithiasis, choledocholithiais with dilated common bile duct with central IHBRD with focal acute pancreatitis. Based on clinical, laboratory and radiological parameters, clinical diagnosis of biliary pancreatitis was made. Patient was managed with IV hydration, analgesics and antibiotics. With conservative management patient was pain free and hemodynamically stable. As the patient was on dual antiplatelet (clopidogrel and ecosprin), clopidogrel was stopped. After 5 days of stopping clopidogrel patient underwent ERCP, biliary sphicterotomy, stone extraction and biliary stenting. Procedure and immediate post procedural period was uneventful. After 12 hours of ERCP procedure patient complained ofsevere right hypochondriac pain with tachycardia and hypotension (90/60 mmHg). His blood investigation showed a drop in haemoglobin (from 12g/dl to 5.1g/dl) with leucocytosis. CECT abdomen showed 13.5 cm hematoma in subcapsular and segment 7 of the liver (Figure 1 & 2). Patient was managed conservatively with blood transfusion, intravenous (IV) antibiotics and analgesics. He improved with conservative management and there was no further drop in haemoglobin. Patient was discharged after 5 days with stable haemoglobin and no pain and fever. At follow up after 4 weeks, patient’s haemoglobin improved to 10g/dl. Patient is planned for interval cholecystectomy followed by stent removal.
Discussion
Bleeding is one of the most feared complication of therapeutic ERCP in the earlier days. With the advances in equipment and expertise, it has become relatively uncommon complication of ERCP and mostly limited to sphincterotomy site. In experienced hands, bleeding or hematoma involving the liver, spleen, intestinal wall or abdominal cavity are extremely rare.
Sub capsular hepatic hematoma is an exceptionally rare complication, only few case reports are available in medical literature. Etiology of hepatic hematoma is not completely understood, proposed mechanisms include guide wire induced trauma to intrahepatic small calibre vessels, traction injury by balloon during stone extraction leading to rapture of bile ductules or vessels.3
According to guidelines, ERCP with sphincterotomy is considered as a procedure with an intermediate risk of bleeding; clopidogrel should be stopped 5 days prior and aspirin can be continued without increased risk of bleeding.5 In our case even though he did not have any bleeding from sphincterotomy site, we feel development of hepatic hematoma might be contributed by aspirin along with the previously proposed hypothesis.
In literature, most common presenting features of hepatic hematoma were abdominal pain (91.7%), followed by anaemia (43.8%), hypotension (29.8% and fever (20.8%).3,4 The symptoms usually develop few hours after ERCP (mean 46.8h), but in few cases delayed presentation as late as 15 days has been reported. Presence of these clinical features along with laboratory features like drop in haemoglobin/, leucocytosis should arise suspicion of this rare post- ERCP complication. However confirmation is done by radiological imaging (ultrasonography, computed tomography-CT and magnetic resonance imaging-MRI). CT or MRI is more accurate in confirming the diagnosis including the size, site and parenchymal extension. Hepatic hematoma most commonly developed in right lobe (95.1%) and mean size was 116 mm x 93 mm. Left lobe HH and multiple hematomas are rare. In our case, he had typical clinical features of bleeding (abdomen pain, hypotension and drop in haemoglobin) and radiological feature confirmed right lobe hematoma.
Management of HH should be decided by a multidisciplinary team (gastroenterologist, interventional radiologist and surgeon) and should be tailored according to clinical picture. In literature majority were successfully managed conservatively (38.3%), followed by percutaneous drainage in 31.9%, embolization in 14.9% and surgery in 25% cases.3,4 In 10.4% cases combined approach was needed. Conservative management is advisable in hemodynamically stable patients and percutaneous drainage/embolization for hemodynamically unstable patients. Surgery should be considered in presence of signs of peritonitis or failure to improve on conservative management. These patients carry high risk of mortality (~10%), anaemia and need for surgery were independent factors for mortality. Early recognition of this complication and timely management with IV antibiotics, blood transfusion was associated with favourable outcomes. Death is mainly due to hypovolemic shock in 75% and to sepsis in the remaining patients.
In conclusions, HH is a rare, but potentially lethal complication if recognised late. Early recognition, followed by appropriate management through multidisciplinary team can salvage these patients with favourable outcome.
References
- Kröner PT, Bilal M, Samuel R, Umar S, Abougergi MS, et al. Use of ERCP in the United States over the past decade. Endosc Int Open. 2020 Jun;8(6):E761-E769.
- Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020 ;52(2):127-149.
- Pivetta LGA, da Costa Ferreira CP, de Carvalho JPV, Konichi RYL, Kawamoto VKF, et al. . Hepatic subcapsular hematoma post-ERCP: Case report and literature review. Int J Surg Case Rep. 2020;72:219-228.
- Imperatore N, Micheletto G, Manes G, Redaelli DG, Reitano E, et al. . Systematic review: Features, diagnosis, management and prognosis of hepatic hematoma, a rare complication of ERCP. Dig Liver Dis. 2018 Oct; 50(10):997-1003.
- ASGE Standards of Practice Committee, Acosta RD, Abraham NS, Chandrasekhara V, Chathadi KV, Early DS, et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016; 83(1):3-16.