48uep6bbphidcol2|ID
48uep6bbphidvals|3055
48uep6bbph|2000F98CTab_Articles|Fulltext
Hepatolithiasis is a rare disease in India. Here we report a patient with extensive hepatolithiasis with biliary obstruction. She presented with secondary biliary cirrhosis, developed rapidly progressive liver failure and died.
Case Report
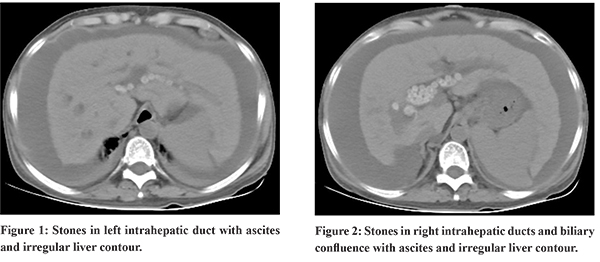
A 53-year-old lady presented with jaundice, ascites and hepatic encephalopathy. There was no history of fever or abdominal pain. Her ultrasound abdomen confirmed liver cirrhosis with dilation of intra-hepatic biliary radicles with filling defects. Hepatitis B surface antigen and anti HCV antibody was non-reactive. Her computed tomography of abdomen confirmed extensive hepatolithisis with ascites (Figure 1 and 2). A diagnosis of secondary biliary cirrhosis was made. Magnetic resonance cholangiopancreatography ruled out common bile duct stones. Arterial ammonia was 182 (normal range 11 to 51 micro mol per litre) she had high SAAG (2.15) ascites and no spontaneous bacterial peritoninits.
Serum bilirubin 17.97 mg per dl (reference 0-1), direct bilirubin 15.8 mg per dl (reference 0-0.3), alkaline phosphatase 143 units per liter (reference 35-105), aspartate aminotransferase 87 units per liter (reference 0-40), alanine aminotransferase 56 units per liter (reference 0-40 ), serum albumin 3.22 mg per dl (reference 3.5-5.2) to INR 1.25. There was no history of fever, abdominal pain in past. There was no prior history suggestive of liver disease.
Unfortunately, patient has a rapidly progressive course of illness and could not be referred for liver transplantation and died.
Discussion
Our patient had hepatic encephalopathy as substantiated by features of liver cirrhosis and ascites on computed tomography. She developed rapidly evolving liver failure. Although, she did not have symptoms of biliary obstruction or cholangitis in past. Hepatolithiasis involves presence of gallstones proximal to the confluence of left and right hepatic ducts, irrespective of presence or absence of common bile duct stones.1 Hepatolithiasis is frequently encountered in East Asian countries and is rare in other parts of the world.2 Cause of hepatolithiaisis is unknown, parasitic infestations, bacterial infections, dietry factors, environmental and genetic causes have been implicated.3 Hepatolithiaisis may cause in recurrent cholangitis, secondary biliary cirrhosis and cholangicarcinoma.1
Feng et al. proposed Dong’s classification for hepatolithiasis, in this classification diffusely distributed stones with bilary cirrhosis were classified as type IIc and liver transplant is recommended in such patients. On the other hand, patients with localized stones or diffuse stones without cirrhosis (Types 1 and IIa and IIb), are best managed with hepatectomy.4
References
- Sakpal SV, Babel N, Chamberlain RS. Surgicalmanagement of hepatolithiasis. HPB (Oxford). 2009;11:194-202.
- Tazuma S. Gallstone disease: Epidemiology, pathogenesis, andclassifcation of biliary stones (common bile duct and intrahepatic).Best Pract Res Clin Gastroenterol 2006; 20: 1075-1083
- Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: A review. World J Gastroenterol. 2015;21:13418–13431.
- Feng X, Zheng S, Xia F, Ma K, Wang S, Bie P, Dong J.Classification and management of hepatolithiasis: A highvolume, single-center’s experience. Intractable Rare Dis Res. 2012; 1:151-156