|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Japan Narrow Band Imaging Expert Team, Magnifying Endoscopy, Narrow-band Imaging, Colonoscopy, Colorectal Neoplasms. |
|
|
|
Deepthi Mareedu, Sojan George Kunnathuparambil, Robert Panakkal Paul, Anoob John KA, Anoop Poulose Department of Gastroenterology, Amala Gastro Centre, Amala Institute of Medical Siences, Amalanagar, Thrissur-680555, India.
Corresponding Author:
Dr Sojan George Kunnathuparambil E-mail: sgkunnathil@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.664
Abstract
Background: Real time visual differentiation of colorectal polyps into benign and malignant helps to decide the appropriate treatment strategy and avoid the unnecessary risk associated with endoscopic therapies and need for repeat procedures. The Japan NBI Expert Team (JNET) classification developed in 2014 classifies colorectal polyps into types 1(Hyperplastic polyps including sessile serrated polyps), 2A (low grade dysplasia), 2B (high grade dysplasia/ superficial submucosal invasive carcinomas) and 3 (deep submucosal invasive carcinomas). We conducted this study to evaluate the diagnostic accuracy of the JNET classification for colorectal polyps. Methods: All patients undergoing colonoscopy in a tertiary care Centre in south India from February to July 2020, who had colorectal polyps were included in the study. A prospective image evaluation to identify the JNET class was done by 2 independent observers blinded to the histological diagnosis and the result was compared with the final histopathological diagnosis. Inflammatory polyps were excluded. The collected data was statistically analyzed to assess the diagnostic accuracy. Result: 139 polyps from 102 patients were included in the study. Most common locations were ascending colon (31%) or rectosigmoid (30.3%). 21 polyps were hyperplastic polyps, 78 polyps were LGD, 23 were HGD/SM-S and 17 were SM-D polyps. On NBI imaging, 23, 76, 30, and 10 polyps were classified as JNET types 1, 2a, 2b and 3 respectively. The diagnostic accuracy of JNET classification was 98.5%, 88.4%, 83% and 93.5% respectively. Conclusion: The JNET classification has a high diagnostic accuracy for predicting the histology of colorectal polyps and hence recommended.
|
48uep6bbphidcol2|ID 48uep6bbphidvals|3052 48uep6bbph|2000F98CTab_Articles|Fulltext Introduction
Colorectal cancers most often arise from adenomatous polyps through a series of genetic changes, also called as the adenoma-carcinoma sequence1,2. Accurate diagnosis of the type of colorectal polyps is essential to decide the appropriate treatment strategy. Inaccurate diagnosis can lead to unnecessary polypectomies and need for a second procedure in clinical practice, giving rise to potential negative consequences for patients and higher medical costs. Hence efforts are being made to improve the real-time precise endoscopic diagnosis of colorectal neoplasms. Narrow Band Imaging (NBI) is an advanced optical technology which uses interference filters to illuminate the target area with red, blue or green wavelengths. This helps in better visualization of vascular network and mucosal surface patterns of the lesionsand helps in improving the real-time diagnosis3. Several studies have indicated that NBI of colorectal polyps is very useful in predicting the histology4-7. The Japan NBI expert team proposed a universal NBI magnifying endoscopic classification for colorectal tumors (JNET classification) in 20148. Although JNET classification has been shown to be highly accurate and effective in studies from Japan9-12, it has not been used widely. We conducted this study to evaluate the usefulness and diagnostic accuracy of the JNET classification in real time diagnosis of colorectal neoplasms. Study Methods
After getting institutional ethical committee approval and informed consent from the patients, a prospective, observational analytical study was conducted among patients undergoing colonoscopy in a tertiary care hospital in central Kerala between February and July 2020. Colonoscopy was done after split dose preparation of colon preparation solution which contains sodium, potassium and magnesium sulphates. Polyps were evaluated using under water imaging or near focus to ensure better visualisation of mucosal and vascular patterns. The endoscopic images captured using the EvisExera III 190 series system were reviewed by an independent observer who was blinded to final histopathological diagnosis. Polypectomy was done using snare after lifting with saline. Inflammatory polyps, Polyps in which polypectomy was not done, or where there was disagreement between the observers, were excluded from the study. 158 polyps were diagnosed of which 19 were excluded. Polypectomy was not done in 9 polyps, 5 polyps were inflammatory polyps and in 5 polyps there was disagreement about the class among the observers and hence excluded. Polypectomy was not done in 6 polyps as they were referred for surgery as the polyps were not getting lifted up after submucosal saline injection, in 2 cases as they were on dual antiplatelets or anticoagulants and in one patient as the patient was not willing for polypectomy. 139 colorectal polyps from 102 patients were used for final analysis. The consensus NBI diagnosis was then compared with the final histopathological diagnosis. Statistical Analysis
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of the JNET classification was analysed for each classification category. The data obtained were recorded in MS excel worksheet and statistical analysis was done using IBM SPSS v23 program running on windows operating system. Categorical variables were presented in terms of percentages, frequency and proportions. The continuous variables were expressed as mean and for non-normal continuous variables, median was used for description. The strength of association between variables was assessed using Pearson’s correlation test. A p-value of <0.05 will be considered statistically significant.
Result
Clinico-pathological Features
139 polyps from 102 patients were included in the study. 83 (81.4%) patients were males. The mean age of patients included in the study was 62.1 yrs. Polyps ranged from 5 mm to 40 mm in size, with a median of 7 mm (Table 1). The commonest location of polyps was in the ascending colon (49 polyps [31%]) and rectosigmoid region (48 polyps [30.3%]). 18 (11.3%) polyps were located in the caecum, 22 (13.9%) lesions were in the transverse colon and 21 (13.2%) polyps in descending colon (table 1). On histopathology, 21 (15.1%) polyps were hyperplastic polyps, 78(56.2%) polyps were LGD, 23(16.5%) were HGD/SM-S and 17 (12.2 %) were SM-D polyps (Table 1).
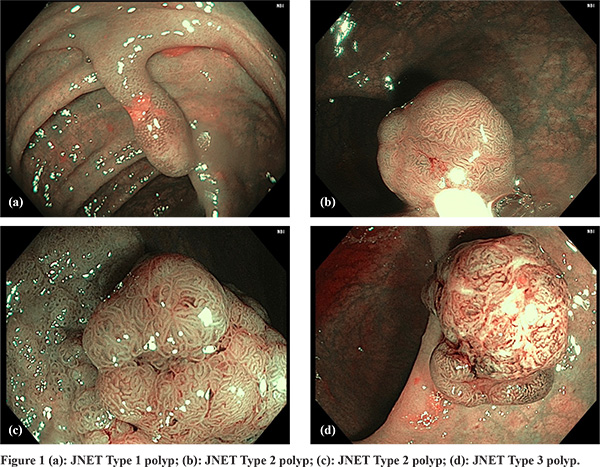
All 139 colorectal tumors enrolled in this study were classified as JNET Type 1, Type 2A, Type 2B and Type 3 as has been described (Figure 1 a-d). The NBI analysis of 139 lesions revealed 23 type I, 76 cases of type 2a, 30 cases of type 2b and 10 cases type 3 polyps as per JNET classification. On histopathological examination, 21 (91.3%) of type 1 polyps were hyperplastic/ SSA- P, while 2 polyps showed LGD. Among type 2a polyps 69 (90.7%) had LGD, 5 (6.5%) polyps had HGD and 2 (2.6%) had SM-S. among type 2b lesions, 5 (16.6%) polyps had HGD, 10 (33.3 %) had SM-S, 7 polyps (23.3%) had LGD and 8 (26.6 %) had SM-D. Among type 3 polyps 9 polyps (90 %) had SM-D, while 1 polyp had SM-S.
The sensitivity of detection of type 1, 2a, 2b and 3 polyps was 100%, 88%, 65% and 52.9% respectively. The specificity of was type 1, 2a, 2b and 3 polyps was 98.3%, 88.5%, 87% and 99.1% respectively. The positive (PPV) and negative (NPV) predictive values were 91 and100, 90.7 and 85.7%, 50 and 92.6%, and 90 and 96 % for type 1, 2a, 2b and 3 polyps respectively. Overall diagnostic accuracy was 98.5%, 88.4%, 83% and 93.5% respectively for type 1, 2a, 2b and 3 polyps (Table 2).
Discussion
In our study, we analyzed the clinical utility of the JNET classification for the diagnosis of colorectal lesions by classifying 139 colorectal polyps through a review of NBI images and correlating with the histopathological findings. On analysis, JNET Type 1 and Type 2A strongly correlated with the HP-SSP and LGD types, respectively, suggesting that JNET classification alone may be needed for the diagnosis. Further, type 3 polyps had had high specificity, PPV and NPV but low sensitivity. However, the correlation was found to be poor for type 2b polyps, suggesting that additional tests or imaging techniques may be needed for accurate diagnosis. In the present study, the diagnostic accuracy was maximum for JNET type 1 (98.5%). These results are consistent with the previous studies which have shown an accuracy of > 98%. Thus, JNET classification seems to have high diagnostic performance in the diagnosis of type 1 lesions. In contrast, pathological examination revealed that JNET Type 2B included a wide range of colorectal tumors ranging from LGD to SM-D lesions. JNET type 2B had a low sensitivity of 65%. This result is consistent with the finding by Sano and colleagues of various histological features ranging from adenoma to deep SM cancer in type 2B lesions8. Although study by Komido et al10 showed relatively high sensitivity and specificity (90.5 %), other studies by Minoda et al9 and Sumimoto et al11 shows similar results. In a recent large study by Kobayashi et al12 analyzing 1402 polyps, the sensitivity was found to be the lowest for type 2B lesions. This finding is expected based on the original definition from JNET, in which pit pattern diagnosis using crystal violet is the gold standard for differentiating 2B lesions for final treatment decision. In a recent study by Hosotani et al13 it was shown the prevalence of deeply invasive cancer in type 2B lesions was 30.1%. However, the addition of magnifying chromoendoscopy for assessing the pit pattern could help in identifying deeply invasive malignancies and hence may be needed in lesions diagnosed as JNET type 2B. Conversely, JNET Type 3 strongly correlated with SM-D lesions and the specificity of JNET type 3 was 99.1%. However, in the study by Ahire et al from India, the diagnostic accuracy was found to be 96%, 82%, 90% and 97% for type 1, 2A, 2B and 3 lesions respectively. The interobserver agreement regarding classification was also significant with kappa values = 0.76 which suggests substantial agreement. The disagreement in classification among the 2 observers occurred in 5 out of 144 polyps (3.5%) in our study. This was mainly in type 2B polyps. This shows that the classification has reasonable interobserver agreement. A recent study by Kato et al validated the treatment algorithm based on JNET classification in polyps < 10 mm15. Cold polypectomy was done for type 2A lesions while endoscopic mucosal resection (EMR) was done for type 2 B lesions. It was found in the group where treatment algorithm was followed, there was higher rate of complete removal and lower post polypectomy bleeding. However, this study had some limitations as well. This was a single centre study and the reporting was done by an expert endoscopist. Hence it cannot be analysed whether expertise of the colonoscopist makes a difference. Our study included limited number of polyps and patients. A multicentre study including more polyps is needed to prove whether the results can be replicated. Only polyps > 5 mm in size was included in the study. This was done as to ensure that we had a good biopsy specimen to assess accurate diagnosis. Further as this requires a high definition endoscope, the results of the study may not be applicable to centres where this facility is not available. Conclusion
The JNET classification is a valid tool with reasonable interobserver agreement for predicting the histology of colorectal polyps and thereby deciding the treatment option. A JNET diagnosis of Type 1, 2A or 3 corresponds to a pathological diagnosis of an HP/SSP, LGD or SM-d lesion, respectively, without requiring magnifying chromoendoscopy. The diagnostic accuracy of type 2B polyps is low and hence, magnifying chromoendoscopy is strongly recommended for the accurate diagnosis. References - Carethers JM. The cellular and molecular pathogenesis of colorectal cancer. Gastroenterology Clinics. 1996 ;25(4):737-54.
- Leslie A, Carey FA, Pratt NR, Steele RJ. The colorectal adenoma–carcinoma sequence. British Journal of Surgery. 2002 ;89(7):845-60.
- Song LM, Adler DG, Conway JD, Diehl DL, Farraye FA, Kantsevoy SV, et al. Narrow band imaging and multiband imaging. Gastrointestinal endoscopy. 2008 ;67(4):581-9.
- Tischendorf JJ, Wasmuth HE, Koch A, Hecker H, Trautwein C, Winograd R. Value of magnifying chromoendoscopy and narrow band imaging (NBI) in classifying colorectal polyps: a prospective controlled study. Endoscopy. 2007;39(12):1092-6.
- McGill SK, Evangelou E, Ioannidis JP, Soetikno RM, Kaltenbach T. Narrow band imaging to differentiate neoplastic and non-neoplastic colorectal polyps in real time: a meta-analysis of diagnostic operating characteristics. Gut. 2013 ;62(12):1704-13.
- Hewett DG, Kaltenbach T, Sano Y, Tanaka S, Saunders BP, Ponchon T, et al. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology. 2012 ;143(3):599-607.
- Sano Y, Ikematsu H, Fu KI, Emura F, Katagiri A, Horimatsu T, et al. Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Gastrointestinal endoscopy. 2009;69(2):278-83.
- Sano Y, Tanaka S, Kudo SE, Saito S, Matsuda T, Wada Y, et al. Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumours proposed by the Japan NBI Expert Team. Digestive Endoscopy. 2016 ;28(5):526-33.
- Minoda Y, Ogino H, Chinen T, Ihara E, Haraguchi K, Akiho H, et al. Objective validity of the Japan Narrow-Band Imaging Expert Team classification system for the differential diagnosis of colorectal polyps. Digestive Endoscopy. 2019 ;31(5):544-51.
- Komeda Y, Kashida H, Sakurai T, Asakuma Y, Tribonias G, Nagai T, et al. Magnifying narrow band imaging (NBI) for the diagnosis of localized colorectal lesions using the Japan NBI Expert Team (JNET) classification. Oncology. 2017;93(Suppl. 1):49-54.
- Sumimoto K, Tanaka S, Shigita K, Hirano D, Tamaru Y, Ninomiya Y, et al. Clinical impact and characteristics of the narrow-band imaging magnifying endoscopic classification of colorectal tumoursproposed by the Japan NBI Expert Team. Gastrointestinal endoscopy. 2017 ;85(4):816-21.
- Kobayashi S, Yamada M, Takamaru H, Sakamoto T, Matsuda T, Sekine S, et al. Diagnostic yield of the Japan NBI Expert Team (JNET) classification for endoscopic diagnosis of superficial colorectal neoplasms in a large-scale clinical practice database. United European gastroenterology journal. 2019;7(7):914-23.
- Hosotani K, Imai K, Hotta K, Ito S, Kishida Y, Yabuuchi Y, et al. Diagnostic performance for T1 cancer in colorectal lesions= 10 mm by optical characterization using magnifying narrow-band imaging combined with magnifying chromoendoscopy; implications for optimized stratification by JNET classification. Digestive Endoscopy. 2020 Jun 12.
- Ahire DS, Rathi PM, Banka NH, Shah PK. Utility of Japan Narrow Band Imaging Expert Team Classification Using Narrow Band Imaging for Evaluation of Colonic Polyps. Journal of Digestive Endoscopy. 2020 ;11(02):138-45.
- Kato M, Abe K, Kubosawa Y, Sunata Y, Hirai Y, Hirata T, et al. Validation of treatment algorithm based on the Japan narrow-band imaging expert team classification for sub-centimetre colorectal polyps. Endoscopy international open. 2018;6(8):E934.
|
|
|
 |
|
|