48uep6bbphidcol2|ID
48uep6bbphidvals|3040
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Encounter with bile duct injury is a common occurrence despite its incidence being low (ranges from 0.1-0.2% after an open cholecystectomy and 0.2-0.6% following a laparoscopic cholecystectomy)1 in view of the sheer number of cholecystectomies done. Roux en Y hepaticojejunostomy (RYHJ) is the standard of care offered to these patients. In the long term follow up, anastomotic stenosis is a potential complication. Good long-term results have been reported following this procedure2, however there are studies quoting stenosis rate of RYHJ, ranging from 4 to 20%.2-5
Incidence of anastomotic stenosis following choledochal cyst excision and RYHJ is relatively low with described incidence of 0.6 to 3%.6,7 Also, the first attempt at repair is considered the best available chance with more the number of attempted repairs, the poorer the long-termoutcome.8 Most of the available literature on benign biliary stricture (BBS) repair has been on open technique with only a few case reports/ series describing the BBS repair being done laparoscopically with no literature available on laparoscopic Re-do RYHJ. Although technically challenging, laparoscopy has its own inherent advantages like magnification with better visualisation with less tissue trauma and early recovery9. Hence laparoscopy approach is a feasible option if all the requisites of bilio-enteric anastomosis like proper delineation of biliary anatomy, exposure of healthy proximal bile duct with adequate vascular supply, tension-free mucosa to mucosa anastomosis and adequate drainage of all the segments of liver can be achieved.
The present study is aimed at assessing the feasibility of laparoscopic Re-do RYHJ in patients developing HJ anastomotic stenosis in a tertiary Hepatobiliary surgery referral centre.
Methods
A retrospective analysis of prospectively maintained data base of patients operated for BBS at our institute from 2016 to 2018. A total of 144 patients were operated with RYHJ during this period. Of these, 74 patients were operated for BBS and 70 patients were operated with choledochal cyst (CDC) excision-RYHJ. A total of 9 patients presented with RYHJ stenosis managed medically/surgically in the year 2018. Of these, 6 patients were operated with laparoscopic Re-do RYHJ during this period. A detailed history and physical examination were done in all the patients. All available clinical and operative records were reviewed, and the details of the index surgery whenever possible. Common presenting symptoms were jaundice and repeated episodes of fever refractory to medical / radiological management.
All patients presenting with RYHJ stenosis were given a trial of medical management in consultation with a medical gastroenterologist and interventional radiologist and considered for surgery on a failed medical/radiological management. MRI abdomen with MRCP was the preferred imaging to assess the level of stenosis. Associated hepatic artery injury from previous surgery and the presence of atrophy-hypertrophy complex was assessed with CECT. Patients were also evaluated for secondary biliary cirrhosis in long standing symptomatic patients. Of these 6 patients who developed RYHJ stenosis, 4 patients had undergone BBS repair-RYHJ and 2 patients had undergone CDC excision- RYHJ. All the surgeries were performed by a single team of surgeons (AKA and AJ) well trained in advanced hepatobiliary surgery. The technique of laparoscopic Re-do RYHJ approach used is as follows:
Surgical technique (Fig.1-6)
The patient is placed in supine position with a leg split and head end elevated. Pneumoperitoneum is created by inserting a veress needle in the umbilical or the palmer’s point (safe point of entry as minimal adhesions expected at this point of entry). Five ports (a 10 mm, infraumbilical-camera port (10 mm, 300), 12 mm, left hypochondrium port, 2 cms anterior to the the mid clavicular line, 2 cms from the sub-costal margin, 5 mm port just above umblicus level in the mid clavicular line, 5 mm port on right side just above umblicus level in, mid clavicular line, 5 mm port in the epigastric region for liver retraction. are used as depicted in.
Initial adhesiolysis (Figure 1) by blunt and sharp dissection with the help of scissor, ultrasonic energy device and suction cannula is performed to reach the porta hepatis. Often, there are adhesions that fix the liver to the anterior abdominal wall thereby exposing and facilitating dissection in the hepatic hilum with no need for separate liver retraction. Roux jejunal limb is identified and anastomosis taken down to identify the strictured duct.
The hilar plate is lowered to expose the left hepatic duct, which is confirmed by needle aspiration of bile. Multiple needle aspiration should be avoided as a blood clot may form in inside the bile duct from bleeding which then prevents subsequent bile aspiration. Strictured anastomotic end of the bile duct is opened and incision extended along the left hepatic duct. In the absence of a tactile feel, one should be careful not to injure the left hepatic artery while extending the incision on the left hepatic duct. The right hepatic artery, which has a course posterior to the choledochal is not generally encountered in the usual dissection. In case of Type 4 stricture, additional dissection is required to identify the right duct and a ductoplasty is performed and the hepaticojejunostomy is done using interrupted sutures. Magnified view helps in the precise placement of sutures in the anastomosis. The Re-do-RYHJ anastomosis was performed using the same Roux limb after re-fashioning the previous opening using a fine monofilament suture in a continuous or interrupted fashion. None of the anastomosis were stented. The jejuno-jejunostomy was re-checked for patency and any mesenteric defects were closed. A drain was placed close to the anastomosis and brought out through the right abdominal port. Patients were managed postoperatively in a high dependency unit. The drains were removed when the output was non-bilious and < 50 mL. Patients were followed up at 2 weeks, 3 months, 6 months and yearly thereafter and evaluated with ultra-sonogram abdomen, and liver function tests during these follow up.
Statistical analysis
Continuous data were expressed as median and range. Continuous variables were compared using Student’s t test and categorical variables using the chi-square test. P<0.05 was considered statistically significant. Statistical analysis was done using SPSS, version 23.
Results
During the study period, in the year 2018, 6 patients underwent laparoscopic Re-do RYHJ. 5 of these patients had their RYHJ surgery done at our institute while 1 patient referred from outside for symptomatic RYHJ stenosis.
Two patients had BBS type 2 and two patients had type 3 injury for which open RYHJ was done previously. Two patients had undergone lap converted to open cholecystectomy and two had undergone lap cholecystectomy as their index surgery. All four patients had developed controlled external biliary fistula and were operated with RYHJ after control of sepsis after a median duration of 3 months- post bile duct injury. None of these patients had an early repair. Two patients developed RYHJ stenosis post CDC type-1 excision-RYHJ. No patient had documented bile leak in the immediate post-operative period following RYHJ and were discharged after a median hospital stay of 8 days (6-10) and were kept at regular follow-up.
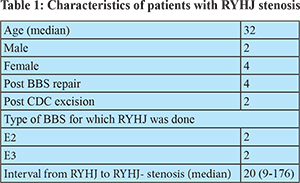
The median age of the patients was 32 with 4 females and 2 males in the group. Median time between RYHJ and Re-do RYHJ was 20 months. One of the patients presented to us 15 years after BBS repair with H-J stenosis and hepatolithiasis. Cases not amenable to radiological/ endoscopic intervention were taken up for surgery. (Table 1)
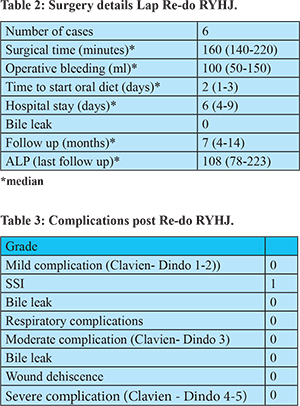
The median duration of Re-do RYHJ surgery was 160 minutes (140-210) with median intraoperative blood loss of 100 ml. Median time to start patients on oral diet was 2 days, initially started on liquid diet and gradually increased to normal diet. (Table 2) Duration of postoperative hospital stay was 6 days (4-9). All the patients had an uneventful post-operative recovery. One of the patients developed mild SSI (clavien- dindo grade 1) which did not prolong his stay in the hospital. Median follow up period is 7 months (4-14) (Table 3). One of the patients who underwent laparoscopic Re-do RYHJ post open BBS repair type 3 presented with complaints of episodes of fever, 4 months post-surgery with MRCP abdomen suggestive of mild intra hepatic biliary radicle dilatation. HIDA scan was done in the patient which showed normal hepatocyte function with no hold up of dye at the Re-do RYHJ site. She was started on medical management to which she responded well with patient being asymptomatic till now on the follow up.
Discussion
RYHJ is the routinely performed drainage procedure for BBS and post-CDC excision. RYHJ stenosis is a well-known complication in the long term follow up with reported rates of 4-20% for BBS and 0.6-3% for post CDC excision RYHJ, respectively.2,6,7
The important determinants of the result after RYHJ include level of the stricture, presence of concomitant vascular injury, portal hypertension, atrophy-hypertrophy complex of liver, number of previous attempts at repair, experience of the surgeon and anastomotic bile leak in the immediate post- operative period.4,10 Untreated RYHJ stenosis can result in patient having recurrent cholangitis, atrophy of liver, biliary cirrhosis and portal hypertension. There are case series describing requirement of hepatectomies and liver transplant in patients presenting late following BBS and stenosed RYHJ.11,12 Hence early intervention is the key for successful repair with good outcomes.
Re-establishing the bile flow draining all segments of the liver is the objective of management. Repair performed on the bile ducts should be wide enough after proper delineation of biliary anatomy, exposure of healthy proximal bile duct with adequate vascular supply, tension-free mucosa to mucosa anastomosis and adequate drainage of all the segments of liver.
A patient with RYHJ stenosis may present with episodes of cholangitis, jaundice and intra-hepatic stone formation. Options available for treatment being radiological (percutaneous dilatation) endoscopic and surgical intervention. These procedures may be used in tandem or exclusively according to the patient presentation. Percutaneous approach is preferred in patients with poor general condition with active cholangitis, not responding to medical management, dilated intra-hepatic biliary radicles with a short segment stricture.13 Also this approach is preferred in patients with supra-hilar, high RYHJ stenosis wherein surgical/ endoscopic intervention results may be sub- optimal.
Anastomotic site access is relatively difficult for endoscopic procedures in RYHJ stenosis. Hence it is a common practice in our institute for complex cases to place an access loop of the roux limb in the subcutaneous plane while doing BBS repair for easy access of the RYHJ anastomosis. Also, patients with low BBS with favourable anatomy and post-CDC excision with mobile duodenum are operated with hepatico-duodenostomy (HD) for biliary drainage in our institute thus, added advantage being easy access of the anastomotic site for endoscopic dilatation, if required.
Initially conservative management was tried in all the patients before contemplating surgery in our study. All 6 patients had dilated intra hepatic biliary radicles, with a formed biliary confluence and three of these patients had hepatolithiasis with ducts packed with large stones making percutaneous approach difficult. Also, these patients were not suitable for endoscopic intervention. At the time of surgery, these patients were in a good general condition and did not have active cholangitis.
Re-do procedures involve dismantling of the anastomosis and re-fashioning of the strictured bile ducts for a healthy anastomosis. Hence more the number of surgeries, more difficult it is at the subsequent surgery.8 Due to previous complex surgery at the same area, local anatomy is normally distorted with fibrosis. With no tactile feedback, while doing laparoscopic dissection, anatomical landmarks should be set with umbilical fissure being the medial limit of dissection and gall bladder fossa forming the lateral limit.In the initial BBS repair, there is a probability of converting a low bile duct injury to a higher one. In our study two patients who had BBS type 2 injury and with RYHJ stenosis appeared to have type 3 BBS intra-operatively after anastomotic takedown and margin freshening and were accordingly dealt with lowering of hilar plate and extension of incision along the left hepatic duct for wider anastomosis. (Hepp-couinaud approach).14 One of the patients who had type 3 BBS (in index surgery) had disconnected ducts after RYHJ take down and accordingly ductoplasty was done before Redo RYHJ. Both the patients with stenosed RYHJ, post CDC excision had an intact primary confluence with anatomy similar to type 3 BBS and hence accordingly Hepp-couinaud approach was followed and Redo RYHJ done.
Re do RYHJ is the most commonly performed surgery for RYHJ stricture and has been traditionally done by an open approach. There is no literature describing laparoscopic approach in the management of RYHJ stricture. The main concern in here being advanced laparoscopic skills required for the dissection in the scarred area, vicinity of major vascular structures to the hilum, difficulty in suturing in atrophy-hypertrophy and varied angulation of the duct difficulty in achieving precisebilio-enteric anastomosis required especially in high strictures. Our initial endeavour in laparoscopic Redo RYHJ started with laparoscopic BBS repair and after completing 20 cases in BBS repair that we embarked on managing Re-do surgery laparoscopically.
Biju Pottakkat et al.15 evaluated 36 patients with failed primary BBS repair with 25 patients operated outside for BBS and 11 patients operated at their institute. In this cohort, 12 patients had an early repair for bile duct injury. Bilio- enteric anastomosis was performed in 22 patients and end to end bile duct repair in 14 patients as their index surgery. All patients with failed BBS repair were operated with open RYHJ. After a median follow up of 37 months, they concluded that long term outcome was the same for both primary repair and for failed BBS repair operated with RYHJ. Also their data analysis yielded that patients who had their primary repair of BBS at peripheral hospitals vis-a vis at a tertiary referral centre, presented early (median time 1.5 months) with symptoms of failed BBS repair. In our study, 5 patients were operated with RYHJ in our institute and they presented after a median duration of 20 months post RYHJ with symptoms of RYHJ stenosis and one patient who was operated in a peripheral hospital presented after 9 months. That BBS repair- RYHJ should be done preferably in tertiary care referral centres with good experience in hepato-biliary surgeries. We have earlier reported our results of laparoscopic hepaticojejunstomy.16
Amine Benkabbou et al.13 managed 44 patients of RYHJ failure. 41% of these patients had undergone surgery for type 2 BBS. Very early repair BBS repair (<48 hrs) was done in 20%, early repair (<45 days) in 50% and delayed repair in 30%. 72% of these patients had their BDI repair done in the authors hospital only. They followed a multidisciplinary approach using both radiological and surgical techniques in their management. 26 of their patients with good general condition without uncontrolled biliary sepsis were assigned for surgical management. 18 patients with marked worsening in their general condition or hepatic function, unfavourable local anatomy or severe sepsis underwent percutaneous technique for stenosed RYHJ management. 4 patients underwent partial hepatectomy for parenchymal atrophy and long segment intra hepatic stricture. None of the patients had refractory cholangitis. Also since all patients, post BBS repair and post CDC excison- RYHJ were at a regular follow up, anastomotic stenosis was detected relatively early in these patients and hence none had secondary biliary cirrhosis, atrophy of the involved segment of liver or portal hypertension.
Conclusion
RYHJ stenosis is a relatively uncommon occurrence. A multidisciplinary approach on a case to case basis and laparoscopic management of RYHJ stenosis in carefully selected cases in well trained tertiary centres yields good results and should be a considered option.
References
- Kaman L, Sanyal S, Behera A, Singh R, Katariya RN. “Comparison of major bile duct injuries following laparoscopic cholecystectomy and open cholecystectomy,” ANZ Journal of Surgery 2006:788–791.
- Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stricture — pattern of recurrence and outcome of surgical therapy. Am J Surg 1984;147:175–80.
- Murr MM, Gigot JF, Nagorney DM, Harmsen WS, Ilstrup DM, Farnell MB. Long-term results of biliary reconstruction after laparoscopic bile duct injuries. Arch Surg 1999;134: 604-9.
- Chaudhary A, Chandra A, Negi SS, Sachdev A. Reoperative surgery for post-cholecystectomy bile duct injuries. Dig Surg 2002;19:22–7.
- Mercado MA, Chan C, Tielve M, et al. Iatrogenic injury to the bile duct — experience with repair in 180 patients. Rev Gastro- enterol Mex 2002; 67: 245–49.
- Qiao G, Li L, Li S, Tang S, Wang B, et al. Laparoscopic cyst excision and Roux-Y hepaticojejunostomy for children with choledochal cysts in China: a multicenter study. SurgEndosc. 2015;29(1):140-4.
- Duan X, Mao X, Jiang B, Wu J. Totally laparoscopic cyst excision and Roux-en-Y hepaticojejunostomy for choledochal cyst in adults: a single-institute experience of 5 years. SurgLaparoscEndoscPercutan Tech. 2015;25:e65–68
- Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stricture — pattern of recurrence and outcome of surgical therapy. Am J Surg 1984;147:175–80.
- Agha, R, Muir, G. . Does laparoscopic surgery spell the end of the open surgeon? Journal of the Royal Society of Medicine 2003; 96: 544-6.
- He Z, Fu Z, Wu Y, Gong J, Zhang W. Surgical management of benign biliary strictures: a 20-year experience. International journal of clinical and experimental medicine. 2016;9(2):4630-4.
- Thomson BN, Parks RW, Madhavan KK, Garden OJ. Liver resection and transplantation in the management of iatro- genic biliary injury. World J Surg2007;31:2363-9
- Laurent A, Sauvanet A, Farges O, Watrin T, Rivkine E, Bel- ghiti J. Major hepatectomy for the treatment of complex bile duct injury. Ann Surg2008;248:77-83)
- Benkabbou, Amine et al. Treatment of failed Roux-en-Y hepaticojejunostomy after post-cholecystectomy bile ducts injuries. Surgery. Volume 153 , Issue 1 , 95 - 102
- Hepp j, couinaud c. L’abord et l’utilisation du canal hépatique gauche dans les réparations de la voiebiliaireprincipale. Presse Med. 1956;64(41):947–948
- Pottakkat, B., Sikora, S.S., Kumar, A., Saxena, R., and Kapoor, V.K. Recurrent bile duct stricture: causes and long-term results of surgical management. J Hepatobiliary Pancreat Surg. 2007; 14: 171–176
- Javed A, Shashikiran BD, Aravinda PS, Agarwal AK. Laparoscopic versus open surgery for the management of post-cholecystectomy benign biliary strictures [published online ahead of print, 2020 Mar 16]. SurgEndosc. 2020;10.1007/s00464-020-07496-6. doi:10.1007/s00464-020-07496-6.