48uep6bbphidcol2|ID
48uep6bbphidvals|3018
48uep6bbph|2000F98CTab_Articles|Fulltext
Primary intestinal lymphangiectasia (PIL) PIL usually presents in first three years of life. It very rarely presents in adulthood for the first time and if it so, it is usually associated with malabsorption. Being identified as ‘idiopathic hypercatabolic hypoproteinemia’ by Waldmann, this clinical entity is also known as Waldmann’s disease.1,2 This case highlights the peculiar finding of Primary intestinal lymphangiectasia on endoscopy and histopathology.
Case Report
A 27-year-old male, presented with history of ascites and pedal edema for last 2 years. He was managed intermittently with diuretics and paracentesis. He had a BMI of 16 kg/m2, muscle wasting, pedal edema, and tense ascites. Investigations revealed low hemoglobin (10gm/dl), normal total leukocyte count (8000 cells/mm3) with lymphopenia (1150 cells/mm3), normal platelet count (3.5x105/mm3), low protein levels (4.5 gm/dl), low albumin levels (1.8 gm/dl) and low globulin levels (2.7 gm/dl). HIV was non-reactive and TSH levels were normal. Serum ANA and Circulating filarial antigen (CFA) detection tests were negative. Urine examination was normal. Ascitic fluid was chylous with low serum albumin ascitic fluid gradient (SAAG), high triglyceride levels (350 mg/dl), normal Adenosine Deaminase (ADA) and negative TB PCR. Cytology was negative for malignant cells.
Ultrasound abdomen with doppler showed massive ascites with normal liver, hepatic veins, and portal vein. X-ray chest showed mild right-sided pleural effusion. The echo showed mild pericardial effusion. CT abdomen showed massive ascites with thickening of the small bowel. Upper Gastrointestinal endoscopy showed multiple whitish specs over the duodenal folds giving a snowflake appearance (Figure 1). Multiple Duodenal biopsies were taken.
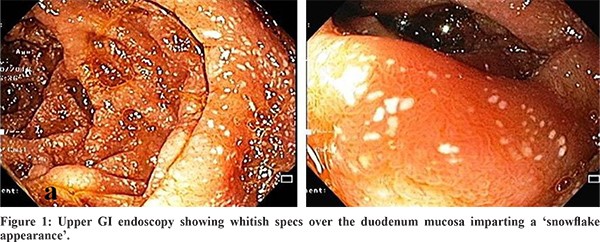
A presumptive diagnosis of lymphangiectasia was made on endoscopic examination. Histopathological examination showed mild broadening of villi and presence of multiple dilated lymphatic lacteal vessels in few villi. Pink coloured homogenous glassy lymph was seen filling the lacteals (Figure 2a & 2b). There were dilated lacteals seen in the lower part of mucosa as well (Figure 3). There was no significant increase in the inflammatory cell population in the mucosa or submucosa. Submucosa was unremarkable. Diagnosis of Primary Intestinal lymphangiectasia was made and patient was treated with high protein, low-fat diet supplemented with medium-chain triglycerides, and supportive treatment.
Discussion
The plan of treatment includes protein rich diet with low content of fat, supplemented with medium chain triglyceride. Medium chain triglyceride provide energy by bypassing the lymphatic system of intestine and get directly absorbed in portal venous circulation. Also, there is no loss of lymph and lacteal engorgement.
Rupture of lacteals leading to lymph leakage which can be prevented by low fat diet which in turn reduces the pressure in the lymphatic system thus prohibiting its dilatation. Thus, the measure found to be more effective in children than adults is a permanent dietary treatment along with total parenteral nutrition needed in some patients. Paracentesis and albumin infusion provide a concomitant supportive therapy.
In non-responders, therapies including tranexamic acid, vitamin D octreotide, antiplasmin, supplementation and surgical resection of segmental or localised intestinal lymphangiectasia.3,4
References
- Waldmann TA, Steinfeld JL, Dutcher TF, Davidson JD, Gordon RS. The role of the gastrointestinal system in “idiopathic hypoproteinemia”. Gastroenterology 1961; 41:197-207. PMID: 13782654
- Bavanandam S, Dheivamani N, Raju B.Primary intestinal Lymphangieactasia in a child. J Gastrointest Dig Syst 2016;6: 446. DOI: 10.4172/2161-069X.1000446
- Jeffries GH, Chapman A, Sleisenger MH. Low-fat diet in intestinal lymphangiectasia. Its effect on albumin metabolism. N Engl J Med. 1964 Apr 9;270:761-6. doi: 10.1056/NEJM196404092701503. PMID: 14107315.
- Aoyagi K, Iida M, Matsumoto T, Sakisaka S. Enteral nutrition as a primary therapy for intestinal lymphangiectasia: value of elemental diet and polymeric diet compared with total parenteral nutrition. Dig Dis Sci. 2005;50:1467–1470. https://doi.org/10.1007/s10620-005-2863-7.