48uep6bbphidcol2|ID
48uep6bbphidvals|3014
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Acute watery diarrheal is defined as diarrhoea that begins acutely, lasts less than 14 days (most episodes last less than seven days), and involves the passage of frequent loose or watery stools without visible blood. In Indian health institutions, up to one-third of paediatric admission are reportedly due to diarrhoeal disease, and 17% of all deaths in indoor paediatric patients are due to diarrhoea.1 In diarrhea, significant morbidity and mortality occur due to loss of water and electrolytes from the body in liquid stools, causing dehydration, metabolic acidosis (due to the loss of bicarbonate), and dyselectrolytemia.
All previous studies of serum electrolyte profile in Indian children presenting with acute diarrhea have been conducted in children of low socioeconomic group.2,3,4,5,6 On the other hand, children from affluent societies are likely to have a different incidence of dyselectrolytemia because of the better educational status of parents, accessibility to readymade ORS, higher chances of seeking early and timely professional advice, and better adherence to standard diarrhoea treatment practices. Therefore, the incidence of dyselectrolytemia may be less in this population, and routine testing of serum electrolytes may not be essential in all children from this subset of the population. This study has been planned to fill this lacuna in the existing state of knowledge and data.
Materials and Methods
Study site: Tirath Ram Shah Hospital, Delhi (TRSCH)
Study population: All patients admitted to TRSCH with the diagnosis of acute diarrhoea, satisfying the inclusion criterion, in the age group from 6 months to 12 years.
Ethical clearance: The study was cleared by the institutional ethical committee
Study design: A Prospective Observational study
Sample size: A calculated sample size of 95 patients was planned.
Inclusion criteria: All consecutive admissions at the TRSCH with the diagnosis of acute diarrhoea, in the age group from 6 months to 12 years from August 2018 to July 2019.
Exclusion criteria: Children with persistent or chronic diarrhoea, severe acute malnutrition (SAM), acute dysentery, septicaemia, or any other coexisting systemic illness.
Methodology: Detailed history, physical examination, and investigations were recorded in specially designed proforma. Demographic profile of patients, details of diarrheal stools like duration, frequency, color, consistency and whether associated with blood or mucus, vomiting, fever, abdominal pain, clinical features suggestive of dehydration, and patient’s socioeconomic status were noted. The correctness of ORS preparation was assessed by measuring the volume of water taken in the utensils in preparation of ORS. Accordingly, the solution was classified as appropriate, concentrated, or diluted. Also, the total amount of water given either with or without ORS was roughly estimated based on the history given by the mother and then compared with the amount of loss of fluid in the form of loose stools and vomiting to determine whether they were given adequate intake of fluids or not. With respect to the frequency of loose stools or vomiting, the highest number was taken when more than one number was told. Modified Kuppuswamy scale was used to assess the socioeconomic status of the family. The child’s nutritional status was graded as per the IAP classification of malnutrition after comparing the weights of children recorded with ICMR standards.
A detailed examination was done to assess the degree of dehydration, presence or absence of features of dyselectrolytemia, and acidosis. At admission, 5 ml of blood was withdrawn to estimate the levels of serum sodium, potassium, chloride, blood urea, and creatinine, besides any other tests indicated clinically.
Before administering antibiotics (if indicated), stool samples were collected in a clean container and delivered to the laboratory immediately. Stool microscopy was done to look for ova, cyst, red blood cells, and pus cells.
Routine investigations like haemoglobin, total and differential leucocyte count, urine examination were done in all cases. In addition, relevant investigations like blood culture, ESR, Chest X-ray, CRP, venous or arterial blood gas analysis were performed wherever clinically indicated.
Statistical analysis: Data collected was subjected to bivariate and multivariate analysis to assess the association between study variables. All the results were calculated using SPSS software v 22.0 and Microsoft Excel. Independent t-tests, ANOVAs test, and chi-square tests were applied for analysis.
Results
A total of 107 children in the age group from 6 months to 12 years with acute diarrhoea were recruited in the study period of one year, out of which 69 were males, and 38 were females. Most patients (69/107) had no dehydration, whereas 34 had some dehydration, and only four had severe dehydration.
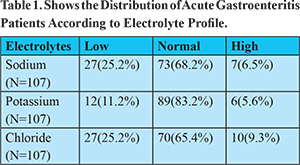
In our study, hyponatremia and hypochloraemia were the commonest electrolyte abnormality (25.2%), followed by hypokalaemia (11.2%), hyperchloremia (9.3%), and hypernatremia (6.5%). (Table 1) Hyponatremia (41%), hypokalaemia (26.5%), and hypochloraemia (35%) were observed more commonly in patients with some dehydration, while patients with severe dehydration had a higher proportion of hypernatremia (50%) and hyperkalaemia (25%). An abnormal serum creatinine level was reported in 10 (9.3%) cases, and high urea levels were seen in 25(23.4%) cases. Increased blood urea levels were seen in 52.9 % (18/34 children) in the some dehydration group compared with 100 % (4/4 children) in the severe dehydration group.
In our study, 52 children (48.6%) had 4-6 stools per day, followed by 36 children (33.6%) having 7-9 stools per day; more than 12 stools/day were reported in only five children (4.7%). Our population’s mean duration of illness was four days, with 58 children (54.2%) presenting with diarrhoea for 4-6 days. In our study, 65.4% of patients had normal nutrition status, 18.7% had grade I malnutrition, 11.2% had grade II malnutrition, and 4.7% had grade III malnutrition. One-third of our population (36, 33.6%) did not take ORS before hospitalization. Out of those taking ORS, 23 (32.4%) were using a diluted solution, 4 (5.6%) were using a concentrated solution, and the rest were using a solution of appropriate strength as per WHO standards. Diluted ORS consumption was significantly associated with hyponatremia (73.9%), hypokalaemia (34.8%), and hypochloraemia (56.5%).
Discussion
Acute diarrheal diseases are amongst the most common diseases in developing countries with significant morbidity and mortality. In children of developing countries, both diarrhoea and malnutrition are common, with a complementary relationship. The pattern of diarrheal illness and attendant dyselectrolytemia have been elucidated previously in studies on children from lower socioeconomic status2,3,4,5,6 but the same may not be true for children from higher socioeconomic backgrounds. The present work was undertaken to study the incidence of common electrolyte abnormalities in children of higher socioeconomic strata (Grade I/II/III according to modified Kuppuswamy scale), admitted with diarrhoea, and the risk factors associated with dyselectrolytemia.
The most common age group in the present study was six months to 1 year (36.4%), followed by 2-5 years (27.1%). Thus, 91.6% of children were below five years of age. In a study by Shah GS et al.7 to evaluate the frequency of electrolyte imbalance, the majority (70%) of patients were below two years of age.
In our study, male patients (64.5%) outnumbered female patients (35.5%), in a ratio of 1.8:1. There were 37 (65%) males and 20(35%) females in the study conducted by Shah GS et al.7 while there were 54.40% males and 45.60% females in the study of Dagar et al.2
In a study conducted by Zulqarnain et al.8 on 90 malnourished children, the average duration of diarrhoea was 4.67±0.821 days, while in our study, the average duration was 4.10 days.
In our study 48.6% of patients had vomiting for 1-3 days, followed by 46.7% who had no vomiting.35.5% of patients had a frequency of 4-6 times per day. In our study, 64.9% of patients had no dehydration, 31.78% had some dehydration, and 3.74% had severe dehydration.
In our study, 65.4% of patients had normal nutrition status, 18.7% had grade I malnutrition, 11.2% had grade II malnutrition, while only 4.7% had grade III malnutrition as a patient enrolled in this study were mostly from affluent socioeconomic strata (Kuppuswamy scale – upper and middle class). No significant correlation was found between socioeconomic status and serum electrolyte levels at admission (p value>0.05). In the study by Dagar et al., 31% of children were severely malnourished. Malnourished children were shown to have a higher electrolyte imbalance study conducted by Bilal et al.9 This could be due to poor sanitation, unhygienic practices, illiteracy, unsafe drinking water, and food unavailability. No significant correlation was found between malnutrition and serum electrolyte levels (p value>0.05) in our study. It might have been because of educational status, early help-seeking behavior in our study population, appropriate use of ORS, and small sample size, which may not represent the general population.
In our study, 36 (33.6%) patients were not taking ORS before hospitalization. Of these, 23 (32.4%) were using a diluted solution, while 4 (5.6%) were using a concentrated solution. Diluted ORS consumption was significantly associated with hyponatremia, hypokalaemia, and hypochloraemia (p value<0.05). Similar results were observed in Ghosh et al.,4 who reported that the consumption of diluted ORS caused hyponatremia in 83.3% of individuals, and all patients who consumed concentrated ORS developed hypernatremia.
Conclusion
The prevalence of diarrhea in children in our study was maximum in age group 6 months to 1 year and decreased with increasing age. The severity of dehydration and dilute ORS administration were important risk factors for dyselectrolytemia. Nutritional status, lower socioeconomic status and type of feeding were not associated with increase in prevalence of dyselectrolytemia in our study. It is important to note that the morbidity and possible mortality due to dyselectrolytemia is preventable by creating awareness about the correct method to prepare the ORS.
References
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva, 1992.P 1-267.
- Dagar J, Shah P, Koppad AM, Singh S. To study serum electrolyte profile in 1 month-5 years children with dehydration admitted to Kimsdu hospital, Karad. J Evol Med Dent Sci. 2016;12(5):7263-6.
- Shah BH, Gosai DK, Chaudhari MR et al. Study of clinical profile in acute gastroenteritis patients with special reference to dyselectrolytemia. IJAR 2016;2(8): 255-7.
- Dastidar RG, Konar N. A Study of Electrolyte Disturbances in a child presenting with acute gastroenteritis, with special emphasis on hyponatremic dehydration-A hospital based cross-Sectional Study:2017: Pediatr Ther 7: 322. doi:10.4172/2161-0665.1000322.
- Pratima P, Geethanjali MP. Study of electrolyte imbalance in children suffering from acute gastroenteritis of under 5 age group: J Evid Med Health.2018;5(46):3210-13.
- Gangaraj S, Das G, Madhulata S. Electrolytes and blood sugar changes in severely acute malnourished children and its association with diarrhoea and vomiting. Int J Pharm Sci Invent.2013;2(5):33-6.
- Shah GS, Das BK, Kumar S, Singh MK, Bhandari GP. Acid base and electrolyte disturbance in diarrhoea. KUMJ.2007;5(1): 60-2.
- Zulqarnain A, Jaffar Z, Iqbal I. Malnourished children with diarrhea. Professional Med J 2015; 22(5):610-4.
- Bilal A, Sadiq MA, Haider N. Frequency of hyponatraemia and hypokalaemia in malnourished children with acute diarrhoea. J Pak Med Assoc.2016;66(9):1077-80.