|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Alcoholic liver diseases, Alcohol, India. |
|
|
|
Atul Gawande, Sudhir Maharshi, Shashank Wanjari, Gaurav Kumar Gupta, Sandeep Nijhawan, Shyam Sunder Sharma Department of Gastroenterology,SMS Medical College and Hospitals, Jaipur, India.
Corresponding Author:
Dr Sudhir Maharshi Email: sudhir.maharshi@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.629
Abstract
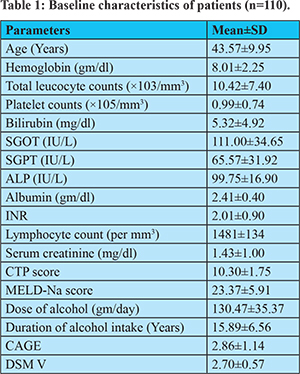
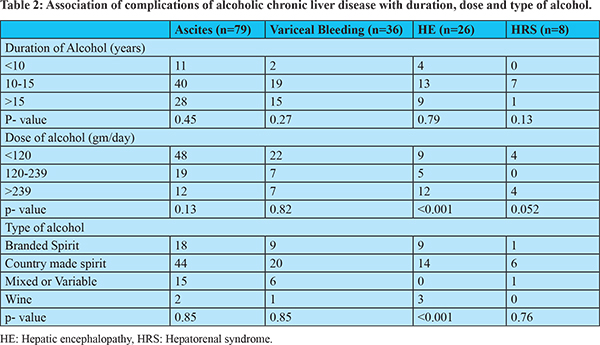
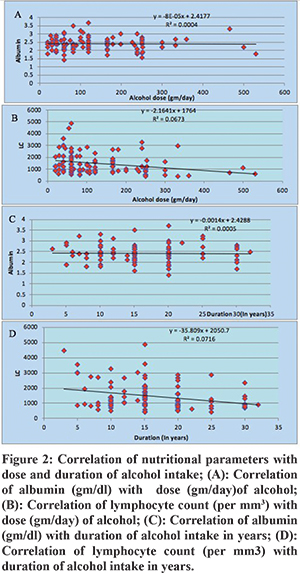
Background: Alcohol-related chronic liver disease (ALD) and its complications are major causes of morbidity and mortality. Predisposing factors for ALD include the amount, type, duration of alcohol consumption, patient’s genetic predisposition, race, sex, and other comorbid conditions. Aims: To study the dose, duration, and type of alcohol consumption in ALD and the effect of these parameters on severity and outcome Methods: This was a prospective study conducted at the Department of Gastroenterology, SMS hospital, Jaipur, between December 2017 to December 2018. All patients with alcoholic liver disease admitted in the department were consecutively enrolled. Data relating to dose, duration, type, alcohol intake pattern, biochemical, ultrasonographic, and clinical parameters were analysed. Results: One hundred ten patients (age 43.5±9.9, all-male) were studied. Mean alcohol consumption was 130.47±35.37gm/day. Sixty-three (57.3%) patients consumed <120gm, 25(22.7%) between 120-239gm, while 22(20%) patients consumed =240gm of alcohol per day. The mean duration of alcohol consumption was 15.89±6.57 years. Fifty-nine (53.63%) patients consumed country-made spirit, 25 (22.72%) branded spirit, 23 (20.91%) mixed or variable type, while three (2.73%) patients consumed only wine. The occurrence of hepatic encephalopathy (HE) was significantly associated with dose (p <0.001) and type (p <0.001) of alcohol consumption. MELD Na score significantly correlated (r=0.48, p <0.001) with dose of alcohol. Conclusion: Our study found a dose-dependent relationship of alcohol intake with hepatic encephalopathy and MELD-Na score. The incidence of ALD did not change with the type of alcohol consumed. Low lymphocyte counts were significantly associated with dose and duration of alcohol intake.
|
48uep6bbphidcol2|ID 48uep6bbphidvals|3017 48uep6bbph|2000F98CTab_Articles|Fulltext Introduction
Alcohol-related chronic liver disease (ALD) and its complications are prominent causes of death worldwide. However, all people who consume alcohol do not develop ALD. There are many reasons for the development of this disease in a subject. These reasons include the amount, type, and duration of alcohol consumption, a person’s genetic susceptibility, race, sex, and other associated conditions.1 The spectrum of ALD constitutes alcoholic fatty liver disease, alcoholic hepatitis, and cirrhosis.2-4 Daily alcohol consumption between 40-80 gm/day increases liver weight, fatty liver, and alcoholic hepatitis, whereas the development of both bridging fibrosis and cirrhosis increases significantly when daily consumption exceeds 80 gm.5 Females are at higher risk of developing ALD than males for any amount of alcohol consumption. South Asians and Indians are more prone to ALD due to their genetic polymorphism. In addition, there is a dose-dependent increase in the risk of alcohol-induced liver damage in both sexes.6-8 Subjects consuming illicitly brewed liquor compared to licit liquor are at a higher risk for ALD.9 Malnutrition may also affect outcomes in ALD.10 The increased access to alcohol with improving socio-economic conditions in India has resulted in a direct increase in ALD incidence. To date, literature is available from the West, but only a few studies are published from India on the pattern of alcohol consumption. This study was conducted to assess the pattern of type, dose, and duration of alcohol consumption in patients with ALD and their effects on the severity of liver disease and outcome.
Methods
This prospective observational study was conducted at the Department of Gastroenterology, SMS Hospital, Jaipur, India, from December 2017 to December 2018. Informed consent was obtained, and the institutional review committee approved the study protocol. All patients with age >18 years with ALD admitted to the gastroenterology department were included in this study. Patients with human immunodeficiency virus (HIV) infection, hepatitis B or C, diabetes mellitus, metabolic syndrome, antinuclear antibody-positive were excluded. Alcohol-related chronic liver disease was defined based on liver function test (LFT), ultrasonography, or liver biopsy with a history of significant alcohol intake (= 25gm/day) for at least five years, after ruling out other reasons for cirrhosis.11,12 CAGE questionnaires were administered to each patient, and patients were divided into mild, moderate, severe alcohol use disorder according to the Diagnostic and Statistical Manual of Mental Disorder V (DSM V criteria).13 All patients underwent LFT, kidney function test, complete blood count, and upper gastrointestinal endoscopy. A detailed history was obtained from each patient related to alcohol consumption in terms of type, dose/day, duration, and pattern of alcohol intake. The dose of alcohol was calculated in grams as 10 grams of alcohol is equivalent to 30 ml of branded spirits (like whisky, vodka, gin), 100 ml of wine, or 250 ml of beer.1 Alcohol concentration in country-made spirit is not fixed. It ranges from 25% to 50% alcohol by volume (ABV).1 In this study, we assumed the concentration of country-made spirit to be equivalent to branded spirits (40%). The alcohol concentration in wine and beer is 9-16% and 4-8% ABV, respectively. Hepato-renal syndrome (HRS) was diagnosed according to the International Club of Ascites 2015.14 Hepatic encephalopathy was diagnosed based on West Haven criteria.15 Anaemia was defined as haemoglobin < 13.0 gm/dl (men) or <12 gm/dl (women).16 Acute-on- chronic liver failure (ACLF) was diagnosed per Asian Pacific Association for the Study of the Liver (APASL) 2014 consensus recommendations.17 Patients prognostic markers like Model for End-Stage Liver Disease Sodium (MELD-Na) score and Child-Turcotte-Pugh (CTP) score were calculated. The patient’s nutritional parameters (serum albumin concentration and lymphocyte count) were also measured. The statistical analysis was performed using Statistical Package for Social Sciences (SPSS) trial version 23.0 for windows (SPSS, Chicago IL, USA). Categorical variables were expressed as an absolute number with percentage, while continuous data were presented as mean± standard deviation (SD). Ranges were calculated for continuous variables as appropriate. Analysis of variance (ANOVA) test for quantitative data and chi-square test for categorical data were used to assess association. Spearman’s non-parametric conduction test was used to assess the correlation of dose and duration of alcohol with nutritional parameters, CTP, and MELD-Na score. A p-value of <0.05 was considered to be significant.
Results
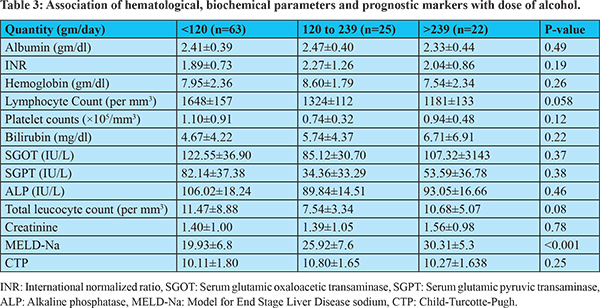
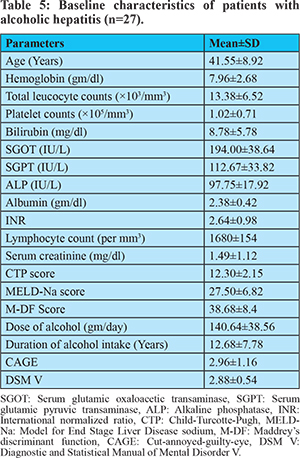
One hundred and ten patients with ALD were included in the study. All patients were male with age 43.57±9.95 years. Baseline demographic and laboratory parameters are shown in table 1. Fifty-nine (53.63%) patients consumed country-made spirit, 25 (22.72%) consumed branded spirits, 23 (20.91%) consumed mixed or variable types of spirit, while three (2.73%) patients consumed only wine. None of the patients predominantly consumed beer. Sixty-three (57.27%) patients consumed <120 gm of alcohol per day, 25 (22.72%) consumed 120-239 gm per day, and 22 (20%) consumed = 240 gm of alcohol per day. The mean intake of alcohol was 130.47±35.37gm/day. The mean duration of alcohol intake was 15.89±6.56 years. The mean duration of abstinence from alcohol before current admission was 23.4±8.5 days. Anemia was observed in 107 (97.27%) patients, jaundice in 29 (26.36%), splenomegaly in 75 (68%), and hepatomegaly in 10 (9%) patients. The mean MELD-Na score was 23.37±5.91, while the mean CTP score was 10.30±1.75. Seventy-one (64.5%) patients were in Child class C, 37 (33.63%) were in Child class B, while two (1.8%) patients were in Child class A. None of the patients underwent liver biopsy for diagnosis of ALD. Complications in patients with ALD were ascites, variceal bleeding, HE, and HRS. Ascites was present in 79 (71.8%), variceal bleeding in 36 (32.7%), HRS in eight (7.3%), and HE in 26 (23.6%) patients. Of the 26 patients of HE, five were in grade I, 15 in grade II, four in grade III, and two patients were in grade IV HE. None of these complications were associated with the duration of alcohol use. Only HE was significantly associated with the dose of alcohol (p <0.001) and type of alcohol (p <0.001). Hepatic encephalopathy was more common in patients who consumed wine (p< 0.001), as shown in table 2. None of the haematological, biochemical parameters and prognostic markers were associated with the dose and duration of alcohol except MELD Na with dose and total lymphocyte count with the duration of alcohol (table 3,4). Thirty-eight (34.54%) patients had a history of binge drinking, and 27 (24.54 %) patients were diagnosed with alcoholic hepatitis with mean Maddrey’s discriminant function (M-DF) 38.68±8.4. Baseline demographic and laboratory parameters of alcoholic hepatitis patients are shown in table 5. Twenty-five (22.72%) patients were diagnosed with ACLF. All ACLF patients had alcohol-related cirrhosis as a chronic component, while 20 (80%) patients had alcoholic hepatitis as an acute component of ACLF. There was a positive correlation between the dose of alcohol and MELD-Na, which was statistically significant r = 0.52, p <0.05 (figure 1). MELD-Na did not correlate with duration and type of alcohol. There was a small positive correlation between CTP score and dose of alcohol (r= 0.051, p>0.05). CTP score did not correlate with duration or type of alcohol of intake. Serum albumin level did not correlate either with dose or duration of ethanol. Lymphocyte count negatively correlated with the dose and duration of alcohol intake r = -0.25 and -0.26 respectively, p<0.05 (figure 2).


Discussion
Our study found no difference in ALD occurrence between different types of alcohol intake, including country-made spirit. There was no difference in complications of ALD except for HE. The prognostic factors (MELD-Na and CTP score) were also comparable for the type of alcohol. A study from Mumbai revealed that ALD was more common in patients who drank country-made liquor and that liver involvement occurred earlier at a lower dose of alcohol than the western population.9 Another study from north India found no difference between complications and prognostic scores in patients consuming branded or country-made spirits.1 A study from Jharkhand showed a higher prevalence of ALD at less alcohol with country-made spirit and Hadiya (rice beer).18 The percentage of alcohol in the country made spirit is not standardised, and this may have hepatotoxin, which depends upon manufacturers from different states. Therefore, it is difficult to say whether country-made spirit has a higher risk of ALD at a lower dose. In our study mean duration of alcohol consumption was 15.89±6.56 years. Fifty-nine (53.63%) patients consumed alcohol for 10 to 15 years, 38 (34.54%) consumed for more than 15 years, while 13 (11.81%) patients consumed alcohol for less than ten years. A study on the use of country-made spirit and its relation with ALD from Mumbai revealed that 86% of cirrhotic patients were taking alcohol for <15 years.9 Another study on 258 alcohol-abusing men free from cirrhosis showed 38 patients developed cirrhosis over the period of 10-13 years.19 In this study, the complications of ALD, MELD-Na, and CTP scores did not significantly correlate with the duration of alcohol consumption. Similar results were seen in another study. The authors did not find a significant correlation of MELD-Na score and discriminant (DF) function score with the duration of alcohol intake but found CTP score significantly correlated with the duration of alcohol consumption.1 The incidence of ALD increases exponentially with an increase in the amount of alcohol consumption.20 Different studies have given different thresholds for the amount of alcohol for the development of ALD.6,21,22 A study from eastern India noted the amount of alcohol to be 81-90 gm/day for nine-twelve years in patients with ALD.23 In our study, the mean amount of alcohol consumption was 130.47±3.37 gm/day. HE occurrence was significantly associated with the quantity of alcohol consumption; these results are compatible with another study from India.1 Patients who consumed more alcohol had a high MELD-Na score, but there was a weak correlation between the amount of alcohol and CTP score. However, there was a significant correlation of CTP with the duration of alcohol intake. Malnutrition is common in patients with ALD, and it depends on various factors.24-28 In our study, albumin concentration was not significantly associated with the dose or duration of alcohol. However, low lymphocyte counts significantly correlated with dose and duration of alcohol consumption. The degree of malnutrition has been shown to correlate with the serious complications of ALD and mortality.10 Our study has a few limitations: all the patients were male; long-term follow up data was not collected; only patients with chronic liver disease requiring admission were included, so other spectrums of alcoholic liver disease like fatty liver and mild alcoholic hepatitis could not be assessed.
Conclusion
Our study found a dose-dependent relationship of alcohol intake with hepatic encephalopathy and MELD-Na score. However, there was no correlation of type of alcohol consumed or duration of alcohol consumption with ALD severity in prognostic scores and complications of ALD. The incidence of ALD did not change with the type of alcohol consumed. Low lymphocyte counts were significantly associated with dose and duration of alcohol intake.
Abbreviation: ALD (Alcohol related chronic liver disease), HE (Hepatic encephalopathy), MELD Na (Model for end stage liver disease sodium), HIV (Human immunodeficiency virus), ANA (Antinuclear antibody) LFT (Liver function test), DSMV (Diagnostic and statistical manual of mental disorders V), ABV (Alcohol by volume), HRS (Hepatorenal syndrome), CTP (Child Turcotte Pugh), ANOVA (Analysis of variance), TNF (Tumor necrosis factor), M-DF (Maddrey’s discriminant function), ACLF (Acute-on-chronic liver failure)
References - Nand N, Malhotra P, Dhoot DK. Clinical Profile of Alcoholic Liver Disease in a Tertiary Care Centre and its Correlation with Type, Amount and Duration of Alcohol Consumption.J Assoc Physicians India 2015;63:14-20.
- Crabb DW. Pathogenesis of alcoholic liver disease: newer mechanisms of injury. Keio J Med.1999;48:184–188.
- Crawford JM. Histologic findings in alcoholic liver disease. Clin Liver Dis2012;16: 699–716.
- Theise ND. Histopathology of Alcoholic Liver Disease. Clin Liver Dis2013;2: 64-67.
- Savolainen VT, Liesto K, Mannikko A et al. Alcohol consumption and alcoholic liver disease: evidence of athreshold level of effects of ethanol. AlcoholClin Exp Res1993; 17:1112-1117.
- Becker U, Deis A, Sorensen TI et al. Prediction of Risk of Liver Disease by Alcohol intake,Sex, and Age: A prospective population study. Hepatology1996; 23:1025-1029.
- Shuppan D, Afdhal NH. Liver Cirrhosis. Lancet2008;371:838–851.
- Douds AC, Cox MA, Iqbal TH et al. Ethnic differences in cirrhosis of the liver in a british city: alcoholic cirrhosis in south asian men. Alcohol and Alcoholism2003;38:148–150.
- Narawane NM, Bhatia S, Abraham P et al. Consumption of‘country liquor’ and its relation to alcoholic liver disease in Mumbai. J Assoc Phys Ind1998; 46:510-513.
- Mendenhall C, Roselle GA, Gartside P et al. Relationship of protein calorie malnutrition to alcoholic liver disease: are examination of data from two Veterans Administration Cooperative Studies. Alcohol Clin Exp Res1995;19:635-641.
- Corrao G, Bagnardi V, Zambon A et al. Meta-analysis of alcohol intake in relation to risk of liver cirrhosis. Alcohol Alcohol 1998;33:381-392.
- Hanck C,Manigold T, Bocker U et al. Gene expression of interleukin18 in unstimulated peripheral blood mononuclear cells of patients with alcoholic cirrhosis. Gut2001;49:106-111.
- Alcohol Use Disorder: A Comparison Between DSM-IV and DSM-5. National Institute on Alcohol Abuse and Alcoholism, 2013. NIH Publication No. 13:7999.
- Angeli P, Gines P, Wong F et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites.J Hepatol2015; 62:968-974.
- Conn HO. Quantifying the severity of hepatic encephalopathy. In: Conn HO, Bircher J, eds. Hepatic Encephalopathy: Syndromes and Therapies. Bloomington, IL: Medi-Ed Press; 1994:20-1099-1100.
- SJ Suh, HA Lee, TH kim et al. Anemia in chronic liver disease. J Hepatol2018;68:182-183.
- Sarin SK, Kedarisetty CK, Abbas Z et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver(APASL) 2014. Hepatol Int2014;8:453-471.
- Jeewan KM, Praneet AM, Bindey K et al. Profile of Alcoholic Liver Disease in Population of Jharkhand: An Insight into the Realm of Alcoholism from Profligacy to Burden. International Journal of Contemporary Medical Research2017;4:770-773.
- Sorensen TI, Orholm M, Bentsen KD et al. Prospective evaluation of alcohol abuse and alcoholic liver injury in men as predictors of development of cirrhosis. Lancet 1984;2:241-244.
- Hozo I, Miric D, Ljutic D et al. Relation between the quantity, type and duration of alcohol drinking and the development of alcoholic liver cirrhosis. Med Arh1995;49:5-8.
- Savolainen VT, Liesto K, Männikkö A et al.Alcohol consumption and alcoholic liver disease: evidence of a threshold level of effects of ethanol.Alcohol Clin Exp Res1993;17(5):1112-1117.
- Lieber CS. Alcohol and liver: 1994 Update. Gastroenterology1994;106:1085-1105.
- Ray S, Khanra D, Sonthalia N et al. Clinico-Biochemical Correlation to Histological Findings in Alcoholic Liver Disease: A Single Centre Study from Eastern India. Journal of Clinical and Diagnostic Research2014;8:1-5.
- StickelF,HoehnB,SchuppanD et al.Reviewarticle: nutritional therapy in alcoholic liver disease. Aliment PharmacolTher2003;18:357–373.
- Khoruts A, Stahnke L, McClain CJ et al. Circulating tumor necrosis factor, interleukin-1 and interleukin-6 concentrations in chronic alcoholic patients. Hepatology 1991;13:267-276.
- McCullough AJ, Buglianese E, Marchesini G et al. Gender dependent alterations in serum leptin in alcoholic cirrhosis. Gastroenterology1998;115:947–953.
- Kiefer F, Jahn H, Schick M et al.Alcohol intake, tumour necrosis factor-a, leptin and craving: factors of a possibly vicious circle? Alcohol and Alcoholism2002;37:401–404.
- Muller MJ, Lautz HU, Plogmann B et al. Energy expenditure and substrate oxidation in patients with cirrhosis: the impact of cause, clinical staging and nutritional state. Hepatology1992;15:782–794.
|
|
|
 |
|
|