|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Endoscopic Retrograde Cholangiopancreatography (ERCP), Post-ERCP Acute Pancreatitis, Pancreaticoduodenectomy. |
|
|
|
Solanki Rashesh1, Mehta Maulik2, Vaishnav Dhaivat3, Desai Gaurav4 1Department of Gastrointestinal Surgery, Narayana Multi-speciality Hospital and GCS Medical College and Research Centre, Ahmedabad, India; 2Department of General Surgery, Civil Hospital, Ahmedabad, India; 3Department of GI Oncology, Apollo Hospitals and Gastrointestinal surgery, GCS Medical college, Ahmedabad, India; 4Department of Community Medicine and Biostatistics, GMERS Medical college, Gandhinagar, India.
Corresponding Author:
Dr Rashesh Solanki Email: raseshsolanki@yahoo.co.in
DOI:
http://dx.doi.org/10.7869/tg.625
Abstract
Background: Pancreaticoduodenectomy (PD) in the setting of preoperative post-ERCP acute pancreatitis (PAP) might pose significant challenges and leads to higher morbidity as compared to those without acute pancreatitis. The aim of the study was to study patients undergoing PD and compare intraoperative variables and postoperative outcomes in patients with and without preoperative PAP. Methods: We retrospectively analysed 20 patients who underwent PD from January 2015 to July 2017. Out of these, 2 patients had preoperative PAP following endoscopic biliary drainage for cholangitis.This group was compared with the rest 18 patients (control group) in terms of patient characteristics, operative variables and postoperative outcomes. Postoperative outcomes and overall complication rate, specifically hemorrhage, delayed gastric emptying and pancreatic fistula were noted. The postoperative complications in stented (n=9) and non-stented (n=11) patients were studied. Risk factors for pancreatic fistula were analysed in entire study population. (n=20). Results: PAP was found in 2 out of 20 patients (10%). The number of complications were higher in the PAP group (8/2) compared to control group (20/18). The ICU stay, delayed gastric emptying (DGE)and postoperative stay was higher in PAP group. There was one perioperative mortality due to grade C pancreatic fistula in the control group. Overall as well as infectious complications, were not statistically different in stented versus non-stented group. Soft pancreas(p=0.001) and non-dialted pancreatic duct (p=0.004) were significantly associated with pancreatic fistula. Conclusion: PD in the setting of PAP is feasible, albeit associated with more frequent complications, prolonged ICU and hospital stay.
|
48uep6bbphidcol2|ID 48uep6bbphidvals|3013 48uep6bbph|2000F98CTab_Articles|Fulltext Introduction
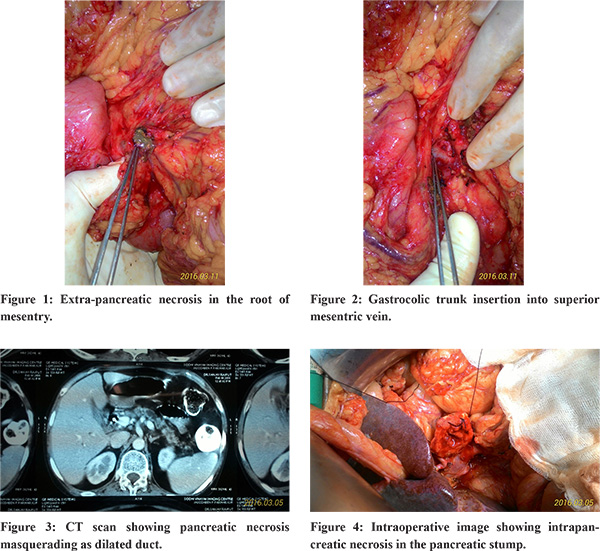
Endoscopic retrograde cholangiopancreatography (ERCP) is commonly performed to relieve biliary obstruction in patients with periampullary carcinoma or carcinoma head of pancreas undergoing pancreatico-duodenectomy (PD). Post-ERCP pancreatitis may pose significant challenges during PD due to obliteration of tissue planes and adhesions as well as necrosis in the root of the mesentery. The study aimed to compare postoperative outcomes in patients with and without preoperative post-ERCP acute pancreatitis. (PAP).
Methods
We retrospectively analysed 20 patients who underwent PD from January 2015 to July 2017. Among these patients, two had preoperative PAP following endoscopic biliary drainage for cholangitis. This group was compared with the remaining 18 patients in the control groupin terms of demographic profile, intraoperative variables such as operative time, blood loss, blood transfusions received, pancreatic texture(soft vs hard), pancreatic duct size, and postoperative outcomes such as ICU and hospital stay, pancreatic fistula, delayed gastric emptying and postoperative haemorrhage.Pancreatic fistula and delayed gastric emptying were defined and graded according to international consensus definitions1,2 and complications were graded according to the Clavien-Dindo classification3.
Results
The number of complications was higher in the PAP group (8/2) compared to the control group (20/18). The demographic profile and operative variables in the PAP group (n=2) and control group (n=18) are shown in Table 1.
Each patient in the PAP group had moderately severe acute pancreatitis according to the revised Atlanta classification (2012)4. 18 patients underwent classical PD and 2 underwent pylorus-preserving pancreaticoduodenectomy (PPPD). The postoperative outcomes and complications with ClavienDindo grading are shown in Table 2.
The duration of ICU and post-operative stay and the incidence of delayed gastric emptying (DGE) were higher in the PAP group. There was one perioperative mortality due to grade C pancreatic fistula in the control group. 9/20 patients underwent endoscopic biliary stenting preoperatively. Complication rates in stented and non-stented patients are shown in Table 3.
The risk factors for pancreatic fistula were analysed. Follow up was available for 18 patients. The mean follow up duration was 15 months. Tumour recurrence-locoregional and distant each with pancreatic head adenocarcinoma occurred in 2 patients. Among these patients, one patient expired at 8 months and the other at 10 months following surgery.
Discussion
Although the role of diagnostic ERCP has diminished, it is still being performed for preoperative endoscopic biliary decompression in patients with obstructive jaundice when indicated. Whereas the overall incidence of post-ERCP pancreatitis ranges from 1% to 6%, the incidence of post-ERCP pancreatitis may exceed 30% in patients considered to be high risk5-7. Younger patients, difficult cannulation, a precut or dilated papilla, and injection of contrast into the pancreatic duct more than once are associated with post-ERCP pancreatitis8. The data on PD in the setting of preoperative post-ERCP acute pancreatitis is sparse. Studies have shown that this is feasible, albeit with higher morbidity9,10. The timing of surgery for PD after PAP is crucial. An interval of 4-6 weeks may be advisable to allow any local complication of acute pancreatitis like necrosis, pseudocyst or abscess to develop. This also permits sepsis control and optimization of general condition especially in patients with severe PAP. Preoperative contrast enhanced computed tomography (CECT) abdomen just before surgery must exclude these local complications and ensure viable (non-necrotic) pancreatic parenchyma as well to ensure a healthy pancreatic stump for anastomosis. In our study, one patient was operated at 33 days and the other one after 64 days of ERCP. Mean serum bilirubin was 7.5 mg/dL before endoscopic biliary stenting. The key intraoperative challenges encountered include inflammatory adhesions and necrosis in the peripancreatic region and the root of the mesentery leading to difficulty in retropancreatic tunnel formation and bleeding from the gastrocolic trunk or the SMV itself (Figure 2). Indeed,higher blood loss and operative time were reported in the study by Hirashita et.al10. Occasionally, a fused lesser sac precluding access may mandate abandoning the procedure itself. Operative tips to perform the procedure successfully in this setting include identifying the inferior border of the pancreas and dissecting close to the pancreatic head, to lead to the retropancreatic tunnel.
Each of the 2 patients in the PAP group had a higher rate of complications (Table 2), and longer hospital and ICU stay. One patient had pus in the peritoneal cavity which was not identified on preoperative imaging. As the patient was stable, surgery was completed. Postoperatively, the patient had hypotension requiring inotropic support and escalation of antibiotics. Similar findings have been reported previously9,10. In the study by Hirashita et.al, PD in the setting of PAP was associated with longer operative time, higher blood loss, elevated CRP and delayed gastric emptying10. In another study by Chen et.al, PAP was associated with a higher rate of severe complications (Clavien grade 3 or higher) and prolonged hospital stay. Moreover, PAP was an independent risk factor for postoperative pancreatic fistula9. As the numbers in our study are low, the impact of PAP on postoperative pancreatic fistula and other complications (Table 2) is difficult to assess.Nevertheless, delayed gastric emptying, prolonged hospital and ICU stay were associated with the PAP group. Delayed gastric emptying is one of the most common complications after PD11,12. The pathophysiology has been poorly understood. The association between delayed gastric emptying and postoperative complications, such as pancreatic fistula, postoperative pancreatitis, and overall complications has been reported previously13,14. In our study, both patients developed delayed gastric emptying with one of them having a severity of grade C requiring nasogastric tube for 22 days postoperatively. Residual local peripancreatic sepsis or collections may lead to delayed gastric emptying in this setting. Although preoperative endoscopic biliary stenting is not associated with major morbidity postoperatively in patients undergoing PD, infectious complications such as wound infection occur more frequently in stented patients, especially when bile is infected15-19. In our study, 9 out of 20 patients were stented. In contrast to the aforementioned studies, overall and wound infections were not statistically significant in either group. This observation could be due to small numbers in each group. The risk factors for pancreatic fistula can be classified into disease-related factors,such as a soft pancreas, non dilated ducts, ampullary, duodenal, cystic or islet-cell pathology; patient-related factors like age more than 70 years, comorbidities like coronary artery disease and duration of biliary obstruction; or operative risk factors like excessive blood loss20. In our study, pancreatic fistula occurred in 6/20 patients(30%), of which clinically relevant fistula formation (grade B or C) occurred in 4/20 (20%). We analysed the risk factors for pancreatic fistula (Table 4) and found that soft pancreas and non-dilated pancreatic duct are risk factors for pancreatic fistula. PAP was not statistically associated with pancreatic fistula in contrast to the study from Chen et.al9. To conclude, PD in the setting of PAP is feasible, albeit challenging and associated with more frequent complications, prolonged ICU and hospital stay.
References - Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: An international study group (ISGPF) definition. Vol. 138, Surgery. 2005. p. 8–13.
- Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: A suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761–8.
- Clavien P a, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
- Banks P a., Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2012;102–11.
- Jeurnink SM, Siersema PD, Steyerberg EW, Dees J, Poley JW, Haringsma J, et al. Predictors of complications after endoscopic retrograde cholangiopancreatography: a prognostic model for early discharge. Surg Endosc. 2011;25(9):2892–900.
- Freeman ML. Adverse outcomes of endoscopic retrograde cholangiopancreatography. Rev Gastroenterol Disord [Internet]. 2002;2(4):147–68. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12481167
- Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, et al. Complications of diagnostic and therapeutic ERCP: A prospective multicenter study. Am J Gastroenterol. 2001;96(2):417–23.
- Silviera ML, Seamon MJ, Porshinsky B, Prosciak MP, Doraiswamy VA, Wang CF, et al. Complications related to endoscopic retrograde cholangiopancreatography: A comprehensive clinical review. J Gastrointest Liver Dis [Internet]. 2009;18(1):73–82. Available from: http://www.embase.com/search/ results? subaction=view record &from=export&id=L355708105%5Cnhttp://www.jgld.ro/12009/12009_ 12.pdf%5Cnhttp://sfx.library.uu.nl/utrecht? sid=EMBASE&issn=18418724 & id= doi:&atitle=Complications + related + to + endoscopic + retrograde + cholang
- Chen YH, Xie SM, Zhang H, Tan CL, Ke NW, Mai G, et al. Clinical impact of preoperative acute pancreatitis in patients who undergo pancreaticoduodenectomy for periampullary tumours. World J Gastroenterol. 2015;21(22):6937–43.
- Hirashita T, Matsumoto T, Izumi K, Ikebe M. Effect of Post-ERCP Pancreatitis on Perioperative Factors of Pancreaticoduodenectomy. 2015;(February):35–41.
- B.W. M, M.G. S, J.A. VH, D.M. N, D.C. M, D. I. Complications following pancreaticoduodenectomy: Current management [Internet]. Vol. 127, Archives of Surgery. 1992. p. 945–50. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference & D=emed5 & NEWS=N & AN=22254969
- Hackert T, Hinz U, Hartwig W, Strobel O, Fritz S, Schneider L, et al. Pylorus resection in partial pancreaticoduodenectomy: Impact on delayed gastric emptying. Am J Surg. 2013;206(3):296–9.
- Murakami Y, Uemura K, Sudo T, Hayashida Y, Hashimoto Y, Nakagawa N, et al. An ante colic roux-en y type reconstruction decreased delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Gastrointest Surg. 2008;12(6):1081–6.
- Braasch JW, Deziel DJ, Rossi RL, Watkins E, Winter PF. Pyloric and gastric preserving pancreatic resection. Experience with 87 patients. Ann Surg [Internet]. 1986;204(4):411–8. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1251310 & tool=pmcentrez & render type=abstract
- Limongelli P, Pai M, Bansi D, Thiallinagram A, Tait P, Jackson J, et al. Correlation between preoperative biliary drainage, bile duct contamination, and postoperative outcomes for pancreatic surgery. Surgery. 2007;142(3):313–8.
- Hodul P, Creech S, Pickleman J, Aranha G V. The effect of preoperative biliary stenting on postoperative complications after pancreaticoduodenectomy. Am J Surg. 2003;186(5):420–5.
- Lermite E, Pessaux P, Teyssedou C, Etienne S, Brehant O, Arnaud JP. Effect of preoperative endoscopic biliary drainage on infectious morbidity after pancreatoduodenectomy: a case-control study. Am J Surg. 2008;195(4):442–6.
- Jagannath P, Dhir V, Shrikhande S, Shah RC, Mullerpatan P, Mohandas KM. Effect of preoperative biliary stenting on immediate outcome after pancreaticoduodenectomy. Br J Surg. 2005;92(3):356–61.
- Velanovich V, Kheibek T, Khan M. Relationship of postoperative complications from preoperative biliary stents after pancreaticoduodenectomy. A new cohort analysis and meta-analysis of modern studies. J Pancreas. 2009;10(1):24–9.
- Callery MP, Pratt WB, Vollmer CM. Prevention and management of pancreatic fistula. J Gastrointest Surg [Internet]. 2009;13(1):163–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18496727.
|
|
|
 |
|
|