48uep6bbphidcol2|ID
48uep6bbphidvals|3015
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Choledochal cysts (CDC) are congenital dilatation of extra/intra hepatic biliary tree which usually present in paediatric population. Upto 20% of CDC can present in adults. Patients may present withassociated complicationslike cystolithiasis, cholangitis, pancreatitis or malignancy1,2. Adults are more likely to present with biliary or pancreatic symptoms and abdominal pain whereas children more likely present with an abdominal mass and jaundice. The classic triad of abdominal pain, right upper quadrant mass and obstructive jaundice is mainly seen in the paediatric population but uncommon in adults with incidence of less than 20%2.
Standard treatment for CDC is excision of entire cyst with bilioenteric reconstruction1-3. Most common methods of bilioenteric reconstruction following CDC excision are Roux-en-Y hepaticojejunostomy (RYHJ) and hepatico-duodenostomy (HD). With the acceptance of minimally invasive approach in hepato-pancreatico-biliary (HPB) surgery, CDC excision is being widely performed laparoscopically. In paediatric population, enough literature is available which support feasibility & long term safety of open HD4 and laparoscopic HD following CDC excision5,6. However, use of HD in adults is limited. Hepaticojejunostomy is the preferred mode of reconstruction in the adult series of laparoscopic CDC excision7,8. Laparoscopic HD has the advantages of technical simplicity and requiring single anastomosis. The aim of the present study is to analyse our experience of HD and to compare the short term and long term outcomes following HD and RYHJ following laparoscopic CDC excision.
Method
This is a retrospective analysis of prospectively maintained data of CDC patients (age >18 years) who underwent laparoscopic CDC excision and biliary-enteric reconstruction in a single surgical unit from January 2016 to March 2021 at GB Pant Institute of Post graduate Medical Education and Research, New Delhi. Choledochal cysts are classified based on Todani modification of the Alonso-Lej classification9. Data about gender, age at operation,type of choledochal cyst, surgical technique and reconstruction type were analysed. Patients were evaluated with history, clinical examination, liver function tests, ultrasound abdomen & MRCP
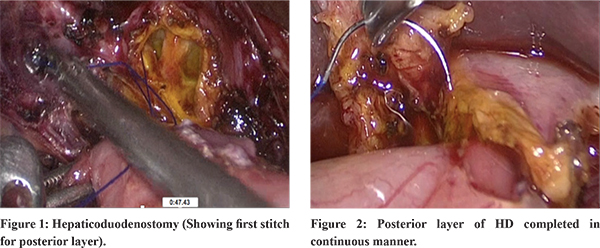
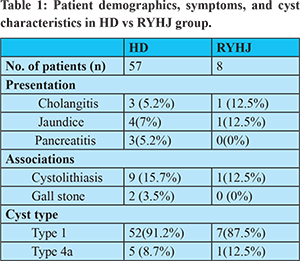
Laparoscopic CDC excision with bilioenteric reconstruction was done. HD was preferred method of reconstruction in our series. HD was performed using 4-0 or 5-0 Polydioxanone suture (posterior continuous and anterior continuous or interrupted) (Figure 1 and 2). In patients who had unfavourable conditions like restricted duodenal mobility or thin friable ducts, RYHJ was done. In patients with Gall bladder cancer (GBC) and CDC laparoscopic radical cholecystectomy (LRC) was done along with CDC excision. However theywere excluded from the study. Patients with CDC with portal hypertension were also excluded. In patients who presented with acute pancreatitis CDC excision was done after the index episode had settled down.
Short-term outcomes included operative time, blood loss and length of hospital stay and complications such as anastomotic leakage and post op bleeding. Long-term outcomes included anastomotic stricture formation and need of reoperation. During the follow up patients were examined clinically and in symptomatic patients LFT and ultrasonography (USG) were performed. MRCP was done in patients with altered LFT or USG showing intrahepatic biliary radical dilatation (IHBRD). McDonalds grading10 was used for grading of anastomotic stricture.
Statistical analysis:Values were reported as mean and standard deviation or median and range. Continuous variables were analysed using students t test, while discrete variables were compared using Pearson’s Chi-squared test. All descriptive analysis and summary statistics were analysed using SPSS Statistics Version 24. Statistical significance was defined by p < 0.05.
Results
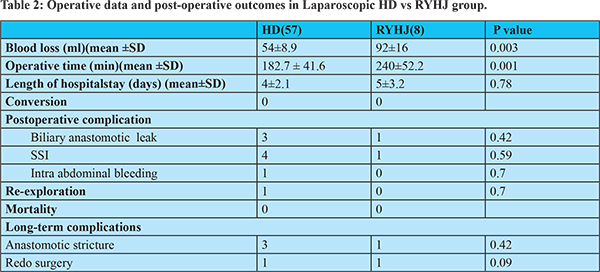
65 patients underwent laparoscopic CDC excision during the study period. Laparoscopic HD was feasible in 57 patients and 8 patients required RYHJ. Demographic characteristics,clinical presentation and cyst characteristics are shown in table 1. Females were more commonly affected than males (F:M=5.4:1). Mean diameter of cyst was 2.59 ± 0.78cm. Mean age of entire cohort was 31.6 ± 12.77 years. Four patients presented with cholangitis (6.1%) and 3 (4.6%) patients presented with acute pancreatitis,5 (7.65%) patients presented with jaundice (highest bilirubin 5mg/dl). Type 1 CDC was present in 59 (90.7%) patients and remaining 6 (9.2%)patients had type 4a CDC. Cystolithiasis were present in 10 (15.3%) patients out of which two patients had prior history of ERC stenting and were managed as CBD stone elsewhere. Two (3%) patients had associated gall stone and 4 (6.1%) patients had prior history of cholecystectomy (two lap cholecystectomy & two open cholecystectomy).Complete cyst excision was possible in all cases. None of the patients required conversion to open surgery. Short-term outcomes (Table 2) like mean operative time was significantly shorter in HD group (182 vs 240 min, p = 0.001). Operative blood loss in HD vs RYHJ group was 54 ml vs 92 ml (p = 0.003). There was no significant difference in length of hospital stay (median 4 vs 5 days, p = 0.78). There was no difference in anastomotic leak rate (3 vs 1,p=0.42 value), Surgical site infection (SSI) rate (4vs1, p=0.59)or postoperative bleeding rate (1vs 0,p=0.7). There was no perioperative mortality.None of the patients had symptoms attributable to bile reflux gastritis. Three patients in HD group developed Mc Donald’s grade 4 anastomotic stricture (2 of them could be managed endoscopically and 1 required redo surgery). One patient is HJ group developed grade 4 stricture who required a redo surgery.Median follow-up was 24 months (3-48 months).
Discussion
Laparoscopic CDC excision with bilioenteric anastomosis is gaining popularity in the management of CDC. Although excision of cyst remains the standard step, bilioenteric anastomosis is either done by HD or RYHJ. A meta-analysis which was published by Narayanan et al11 compared HJ versus HD as a reconstruction method following open CDC excision in children. It concluded that the post-operative outcomes like bile leak, cholangitis, anastomotic stricture, bleeding, operative time and reoperation rate did not differ between HD and HJ group. In children there are studies which compared the outcomes of HD versus HJ following laparoscopic CDC excision5. According to Yeung et al5 short term results were better in HD group and the long term complications were comparable. Their study concluded that HD is a safe and feasible method of reconstruction following laparoscopic CDC excision with better short-term outcomes and comparable long-term outcomes to RYHJ. HD can be used as a method of reconstruction with the advantages oftechnical simplicity,ease and requiring only one anastomosis.
Successful laparoscopic cyst excision with HD reconstruction was first described by Tan et al12 Subsequently, Liem et al13 reported their experience with 74 patients who underwent laparoscopic CDC excision and HD reconstruction, demonstrating that this method is feasible and safe. In his updated series14 laparoscopic HD was performed in 59.5% (238/400) patients. In our study, HD was feasible in 87.6% (57/65) of the patients. Total 8 patients required RYHJ because of restricted duodenal mobilityor thin friable ducts. According to Todani et al15 other factors in which HD may not be indicated are multiple duct opening, aberrant hilar duct anatomy, small duct size and tension at anastomotic site.
In the present study mean operative time was lesser in HD group which was statistically significant. Similar results were seen in the study by Yeung et al5.
As we know most common morbidity of biliary anastomosis is leak and stricture formation. Anastomotic leak rate was reported ranging from 1.7 to 5% in the HD group and 2.5 to 10% in HJ group in large studies14,16,17. In our study, there were 3 anastomotic leaks in HD group (5.5%) and 1 patient (12.5%) in RYHJ group. All were minor leaks which settled over a period of 5-7 days. Leak following HD can be managed with additional help of endoscopic stenting if conservative measures fail. However in our series the anastomotic leaks did not require any additional procedures. Similar leak rates (6.5%) were seen in a study by Zhang et al6 following laparoscopic CDC excision.
In our study 3 patients (5.5%) developed anastomotic stricture in HD group. Amongst which 2 of them could be managed endoscopically (stenting/dilatation) and 1 patient required redo surgery. Postoperative complication & long term complications in laparoscopic HD was comparable to RYHJ group. In a study by Senthilnathan et al8 55 adults were treated with Laparoscopic CDC excision and RYHJ, 2/55 (3.6%) of them developed anastomotic stricture.
Bile reflux gastritis is well known complication following HD. But its incidence is variable in literature ranging from 3.8-33.3%17. Initial study published by shimotokara et al17 and tadaka et al18 showed higher biliary gastritis following HD. But these incidence were endoscopic proven gastritis only. None had clinically significant gastritis. Large series published by Liem
et al.14 reported bile reflux gastritis in only 3.8% of the 238 patients who underwent HD. In our study none of the patients developed clinically significant gastritis. Patil et al20 published twenty five year follow up data of fifty four patients who underwent Open CDC excision with HD in which none of the patients developed clinically significant biliary gastritis.
The major limitations of our study are the retrospective nature and short follow up.
Conclusion
In our study we found that Laparoscopic HD was feasible in 87% of the adult CDC patients. It can be preferred as a method of biliary reconstruction following laparoscopic CDC excision in adults as it is technically easier,requires single anastomosis and also accessible for future endoscopic intervention.
References
- Edil BH, Cameron JL, Reddy S et al Choledochal cyst disease in children and adults: a 30-year single-institution experience. J Am Coll Surg2008; 206(5):1000–1005.
- Lipsett PA, Pitt HA, Colombani PM et al. Choledochal cyst disease. A changing pattern of presentation. Ann Surg 1994; 220(5):644–652.
- She WH, Chung HY, Lan LC et al. Management of choledochal cyst: 30 years of experience and results in a single centre. J PaediatricSurg2009; 44(12):2307–2311.
- Ray BK, TripathyPK, MohantyPK, Jena PK, Mohanty HK. Roux-en-Y hepaticojejunostomy versus hepatico-duodenostomy after excision of choledochal cyst: A randomized clinical trial and experience in a tertiary care hospital. J PediatrRes.2017;4(07):438-445.
- Yeung F, Fung ACH, Chung PHY, Wong KKY. Short-term and long-term outcomes after Roux-en-Y hepaticojejunostomy versus hepatico-duodenostomy following laparoscopic excision of choledochal cyst in children. Surg Endosc. 2020;34(5):2172-2177.
- Zhang B, Wu D, Fang Y, Bai J, Huang W, Liu M, Chen J, Li L. Early complications after laparoscopic resection of choledochal cyst. Paediatric Surg Int. 2019;35(8):845-852.
- Gündogan E, Sümer F, Çolakoglu MK, Çiçek E, Gökler C, Aydin MC, Kayaalp C. Laparoscopic resection of choledochal cysts in adults: a series from Turkey. Turk J Surg. 2019 23;35(3):223-226.
- Senthilnathan P, Patel ND, Nair AS, Nalankilli VP, Vijay A, Palanivelu C. Laparoscopic Management of Choledochal Cyst-Technical Modifications and Outcome Analysis. World J Surg. 2015 ;39(10):2550-6.
- Todani T, Watanabe Y, Toki A, Morotomi Y. Classification of congenital biliary cystic disease: special reference to type Ic and IVA cysts with primary ductal stricture. J Hepatobiliary Pancreat Surg. 2003;10(5):340-4.
- McDonald ML, Farnell MB, Nagorney DM, Ilstrup DM, Kutch JM. Benign biliary strictures: repair and outcome with a contemporary approach. Surgery. 1995 ;118(4):582-90; discussion 590-1.
- Narayanan SK, Chen Y, Narasimhan KL, Cohen RC. Hepaticoduodenostomy versus hepaticojejunostomy after resection of choledochal cyst: a systematic review and meta-analysis. J Pediatr Surg. 2013 ;48(11):2336-42.
- Tan HL, Shankar KR, Ford WD. Laparoscopic resection of type I choledochal cyst. Surg Endosc 2003;17:1495.
- Liem NT, Dung le A, Son TN. Laparoscopic complete cyst excision and hepaticoduodenostomy for choledochal cyst: early results in 74 cases. J Laparoendosc Adv Surg Tech A. 2009 ;19 Suppl1:S87-90.
- Liem NT, Pham HD, Dung le A, Son TN, Vu HM. Early and intermediate outcomes of laparoscopic surgery for choledochal cysts with 400 patients. J Laparoendosc Adv Surg Tech A. 2012 ;22(6):599-603.
- Todani T, Watanabe Y, Mizuguchi T, Fujii T, Toki A. Hepaticoduodenostomy at the hepatic hilum after excision of choledochal cyst. Am J Surg1981; 142:584–587.
- Santore MT, Behar BJ, Blinman TA, Doolin EJ, Hedrick HL, Mattei P, et al. Hepaticoduodenostomy vs hepaticojejunostomy for reconstruction after resection of choledochal cyst. J Pediatr Surg. 2011;46(1):209-13.
- Mukhopadhyay B, Shukla RM, Mukhopadhyay M, Mandal KC, Mukherjee PP, Roy D, Biswas SK, et al. Choledochal cyst: A review of 79 cases and the role of hepaticodochoduodenostomy. J Indian Assoc Pediatr Surg. 2011 ;16(2):54-7.
- Shimotakahara A, Yamataka A, Yanai T et al. Roux-en-Y hepaticojejunostomy or hepatico-duodenostomy for biliary reconstruction during the surgical treatment of choledochal cyst: which is better? PediatrSurg Int 2005; 21(1):5–7.
- Takada K, Hamada Y, Watanabe K, Tanano A, Tokuhara K, Kamiyama Y. Duodenogastric reflux following biliary reconstruction after excision of choledochal cyst. PediatrSurg Int. 2005;21(1):1-4.
- Patil V, Kanetkar V, Talpallikar MC. Hepaticoduodenostomy for Biliary Reconstruction After Surgical Resection of Choledochal Cyst: a 25-Year Experience. Indian J Surg. 2015;77(Suppl 2):240-244.