48uep6bbphidcol2|ID
48uep6bbphidvals|3020
48uep6bbph|2000F98CTab_Articles|Fulltext
Fungal infections are commonly noted in immunocompromised patients. Recent rise of transplant procedures, increased usage of chemotherapy drugs has increased the incidence of these infections. Mucormycosis, caused by fungi of order Mucorales, presents as rapidly progressive, disseminated infections with poor prognosis in immunocompromised hosts. Mucormycosis usually affects rhinocerebral, pulmonary or cutaneous areas. Gastrointestinal involvement is rare. Unusual presentations as colonic-massor inflammatory lesions have also been reported1,2. Here we report a case of colonic-mucormycosis presenting as colonic mass successfully treated by surgery and anti-fungals.
Case Report
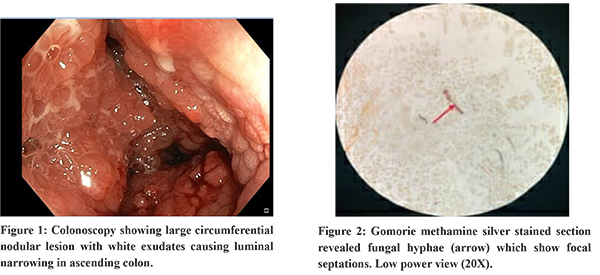
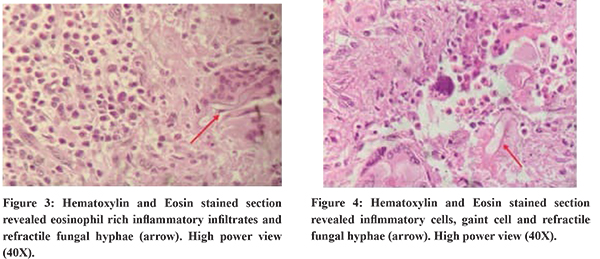
A 50-year-old male resident of Tripura, with uncontrolled diabetes presented with complaints of intermittent right lower-quadrant pain abdomen, occasional bleeding per-rectum, altered bowel habits and weight loss. CECT abdomen showed circumferential irregular wall thickening in terminal ileum, Ileo- caecal junction, caecum, proximal ascending-colon and enlarged lymph nodes in right iliac-fossa. Colonoscopy showed large circumferential nodular lesion with white exudates causing luminal narrowing in the region of ascending colon (Figure 1). Endoscopic biopsy showed extensive eosinophilia without any malignancy or granulomas. Right hemicolectomy of lesion was done due to impending obstruction and inconclusive biopsy. Histopathology of specimen showed dense infiltration with eosinophils and granulomas. Periodic acid–Schiff and Gomori’s Methenamine Silver Staining showed fragmented and broad fungal hyphae with rare septation and focal branching (Figure 2,3,4). There was no evidence of dysplasia, malignancy or angiovasion of fungal elements. Specimen for fungal culture were not sent to microbiology as it was thought to be malignant intra-operatively. Since histopathology showed fungal infection, he was started on itraconazole and which was continued for 3 months post-surgery. Mucormycosis was diagnosed by PCR analysis of formalin fixed paraffin embedded tissue sample. At present the patient is asymptomatic and doing well.
Discussion
Mucormycosis is caused by fungi belonging to class Zygomycetes and order Mucorales. They are ubiquitous, aseptate moulds and are mostly saprophytic organisms. Opportunistic infections in humans are through inhalation, ingestion, or inoculation of spores through skin and blood. Mode of infection determines the site of disease- rhinocerebral, pulmonary, cutaneous, and disseminated disease. Gastrointestinal mucormycosis is rare, accounting for 4-7% of all cases. Stomach is the most common site (57.5%), followed by colon (32.3%) and ileum (6.9%)3. Various risk factors associated were use of immunosuppressive agents, hematologic malignancy, AIDS, uncontrolled diabetes, iron overload states and post solid organ or bone marrow transplantation. Most of the cases were reported in immuno-compromised hosts but few cases were also reported in immunocompetent hosts4. Case reports have also been reported in patients with uncontrolled diabetes as noted in our case. In the current era of rampant morbid obesity with diabetes and India being the capital of diabetes, there could be increased incidence of colonic-mucormycosis.
Most cases of colonic-mucormycosis present with pain abdomen, altered bowel habits, weight loss, fever or symptoms related to other organ involvement, usually with dissemination. Case reports of unusual presentation with hematochezia, perforation and obstruction have also been reported. In our case the fungal infection presented as colonic mass. Similar presentation of colonic-mucormycotic mass masquerading as cancer has also been reported earlier1.
Endoscopic samples were sufficient to make the diagnosis in few cases, but failure has been reported in most cases. It is probable that the fungi reside deep in the mucosa, rendering its retrieval difficult. Further evaluation in these group of patients with image guided biopsy may prevent the patient from the morbidity of surgery. Histopathological examination of biopsy specimens is currently the major diagnostic modality. Features of eosinophilic infiltration with granulomas in immunocompromised patients without features of dysplasia or malignancy may suggest fungal or helminthic infections. Other ancillary tests including fungal cultures, serological tests, and molecular techniques may establish the diagnosis with certainty. In practice, finding of hyphae with characteristic morphological features, tissue invasion and vascular thrombosis may be the only available means, as the diagnosis is rarely suspected for tissue cultures to be performed, before immersing the biopsy material in formalin, which destroys all fungal forms. Usually, these characteristic features are noted in 90% of samples, leading to diagnostic difficulty in rest of them. Molecular tests like fungal PCR, as performed in our case can clinch the diagnosis in difficult cases.
Principles of treatment of mucormycosis are rapid diagnosis, reversal of the underlying predisposing factors, appropriate surgical debridement of infected tissue, and appropriate antifungal therapy. Surgery is mandatory for treatment of patients with obstruction, perforation or fatal invasive-mucormycosis. Medical management with anti-fungals can be considered in selected group of patients. Liposomal amphotericin B is the drug of choice. The usual starting dose is 5 mg/kg daily, which can be increased to 10 mg/kg daily in non-responders. For patients who have responded to amphotericin B, posaconazole or isavuconazole can be used for oral step-down therapy. As Mucormycosis showsin-vitro resistance to echinocandins, caution should be executed while using these as single agents. Although there are no recommendations for duration of anti-fungals, they should continue until there is clinical resolution of infection, as well as resolution of radiographic signs. Therapy should also continue until reversal of underlying immunosuppression has been achieved, when feasible. Itraconazole is the only marketed azole drug that has in vitro activity against Mucorales. There are case reports of successful therapy with itraconazole alone5. In our case only itraconazole was used after surgical resection and the patient does not have any recurrence to date.
Conclusion
Colonic-Mucormycosis can have varied presentations and high index of suspicion is needed for early diagnosis and appropriate management. Endoscopic samples alone might suffice for detection of fungal hyphae in few cases but culture is needed for definitive diagnosis and appropriate anti-fungal therapy. Surgery is needed for diagnosis when endoscopic reports are inconclusive and in complicated infections. Anti-fungals alone can be considered in select group of patients. Surgery is needed for most patients for removal of diseased segment. Untreated cases are fatal, but early diagnosis and initiation of treatment can prevent significant morbidity and mortality.
References
- Kumar Debata, Prasanna et al. ““An unusual presentation of colonic mucormycosis mimicking carcinoma colon- a surgeon’s perspective”.” International journal of surgery case reports vol. 10 (2015): 248-51.
- Shankaralingappa S. Unsuspected invasive gastrointestinal mucormycosis masquerading as inflammatory bowel disease: A pathologist’s perspective. Indian J Pathol Microbiol 2019;62:332-4.
- F. Lanternier, E. Dannaoui, G. Morizot, C. Elie, D. Garcia-Hermoso, M. Huerre, et al., A global analysis of mucormycosis in France: theRetroZygo study (2005–2007), Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 54 (S1) (2012) S35–43.
- Wotiye, A.B., KS, P. &Ayele, B.A. Invasive intestinal mucormycosis in a 40-year old immunocompetent patient - a rarely reported clinical phenomenon: a case report. BMC Gastroenterol 20, 61 (2020).
- Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18(3):556-569.