48uep6bbphidcol2|ID
48uep6bbphidvals|3002
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Extrahepatic biliary obstruction (EHBO) affects a significant proportion of the population worldwide. EHBO refers to obstruction of bile flow from the liver to the duodenum at the extrahepatic biliary system, which can originate within the duct or due to extrinsic compression from a broad spectrum of disorders.
Reports from the different parts of India have found choledocholithiasis, gallbladder carcinoma, carcinoma head of the pancreas and periampullary carcinoma to be the most frequent causes.1-5 There is a lack of data for young patients (= 40 years of age) presenting with the biliary tract obstruction.
Materials and Methods
We retrospectively analyzed the hospital records of all patients at or below 40 years of age, who had undergone ERCP in Gastroenterology Department, Banaras Hindu University, Varanasi, Uttar Pradesh, India from July 2018 till June 2019.
Etiological diagnosis was based on clinical features and examination, blood investigations which included complete blood count (CBC), liver function test (LFT), kidney function test (KFT), prothrombin time (PT/INR), along with imaging with ultrasonography (USG) or contrast-enhanced computerized tomography(CECT), magnetic resonance imaging (MRI) or Magnetic resonance cholangiopancreatography (MRCP). When possible, all diagnoses were confirmed by histopathologically (image-guided FNAC, Brush cytology, Post-surgical histopathology).
Patients underwent ERCP for at least one of the following indications: Choledocholithiasis on imaging, EHBO with cholangitis and intractable pruritis, referral from oncology team before surgery or chemotherapy, or for stent placement across strictures.
Diagnosis of benign biliary stricture6 was based on history, clinical finding, serum markers, imaging studies (MRCP)7,8 and brush cytology. Malignant strictures were identified when definitive evidence of malignancy by serological markers, imaging, or tissue diagnosis whenever available.
Statistical analysis: Data was represented as a percentage for nominal data and mean±SD or range for continuous data. Continuous data were compared using unpaired t-test and discrete variables by?2 test or Fischer-exact test. A p-value <0.05 was considered as statistically significant.
The data was analyzed by using SPSS version-24.0 statistical software (Trial Version). The institutional ethics committee approved the research protocol and all participants had given written informed consent.
Results
During the study period, a total of 1148 patients underwent ERCP, of whom 180 patients were = 40 years of age.
The mean age of patients was 33.38 ± 5.8 years, and most of them were females (67.78%). Choledocholithiasis (F=67.3%), benign biliary stricture (F=76.47%), and gall bladder carcinoma (GBC, F=72.73%) were seen predominantly in females. Periampullary carcinoma (M=60%) preferentially affected males. Pancreatic head carcinoma and cholangiocarcinoma was equally distributed between males and females. The youngest patient with GBC was 25 years of age.
Benign causes were seen in 67.2%, which included choledocholithiasis as the most prevalent cause (n=104, 57.8%) followed by benign biliary stricture in 17(9.4%). (Table 1) The latter was caused by prior cholecystectomy in 14 patients, portal biliopathy in 2 patients, and chronic pancreatitis in 1 patient. Malignant etiologies included GBC (n=44, 24.4%), cholangiocarcinoma (hilar cholangiocarcinoma in 6, and distal cholangiocarcinoma in 2 patients), periampullary carcinoma (5 patient) and pancreatic head carcinoma (2 patient).
The patients presented clinically with jaundice (66.1%), pain abdomen (59.44%), itching (26.11%), weight loss (19.44%, only in malignant EHBO), anorexia, and vomiting. (Table 2) Charcot’s cholangitis triad was present in only 68.18% of patients with cholangitis, fever being most consistent symptom present in all patients.
The mean hemoglobin concentration was higher in benign (12.0 ± 1.8 gm/dl) as compared to malignant causes (10.92 ± 1.67 gm/dl). In patients with cholangitis, total leukocyte count was elevated in 95.54%, and differential count in showed markedly elevated neutrophilic count in all these patients. Renal dysfunction was seen in 8(18.18%) patients with cholangitis. Mean bilirubin (16.9 mg/dl ± 6.8 versus 4.6 mg/dl ± 4.1) and alkaline phosphatase (1170.98 U/L ± 260.73 versus439.34 ± 362.73) were higher in malignant as compared to benign causes. (Table 3)
On imaging studies GBC patients had liver (segment IV, V) infiltration (36.36%), liver metastasis (18.18%), left adrenal metastasis (2.72%), loco-regional lymphadenopathy (40.91%), gastric outlet obstruction (4.55%) and ascites (9.09%). All GBC cases referred for endoscopic biliary drainage had advanced disease (stage 3 and 4) (figure 1).
In patients with choledocholithiasis, 75% also had cholelithiasis. Multiple common bile duct calculi (=2) were found in 37.5% of patients. (Table 4) Complete biliary clearance was achieved in 82 (78.85%) patients. Reasons for failure of biliary clearance with balloon sweeping were large stones >15 mm in size (n=17/104, 16.35%), associated biliary stricture (n=2/104, 1.92%), impacted stones in (n=2/104, 1.92%) and altered anatomy in (n=1/104, 0.96%) patients. (Table 4) Those with failure of biliary clearance were sent for surgicalintervention after biliary drainagewith stent in situ.
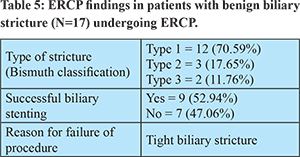
Bismuth type 1, type 2 and type 3 of benign biliary strictures were seen in 70.59%, 17.65%, and 11.76%, respectively. (Table 5) Successful biliary stenting was achieved in only 52.9% patients, and the reason for failure was tight stricture, not allowing guidewire passage across the stricture.
Cholangiography in GBC showed a perihilar stricture of predominantly Bismuth type 2 (n=12, 27.27%) and type 1 (20.45%). (Table 6) Thirteen patients had direct infiltration of CBD not extending up to hila, and three patients had lymph nodes compressing biliary radicles. Adequate endoscopic biliary drainage was achieved in 30/44(68.18%), while 31.82% required percutaneous transhepatic biliary drainage (PTBD) after the failed ERCP, which was successful in all patients. The failure of endoscopic biliary drainage was due to tight biliary stricture (12 patients) and gastric outlet obstruction (2 patients). (Table 6) Adequate endoscopic biliary drainage was achieved in 75%, 80%, and 50% cases of cholangiocarcinoma, periampullary carcinoma, and pancreatic head carcinoma, respectively. Types of hilar cholangiocarcinoma stricture seen were type 2, type 3a, type 4 in 3, 1, and 2 patients, respectively.
Discussion
This study in a young population (= 40 years of age) was done primarily to understand the spectrum, clinical features, and the usefulness of ERCP as a therapeutic or palliative modality in EHBO. In our study, choledocholithiasis and GBC were the most prevalent causes of EHBO. Despite having a younger study population, pancreaticobiliary malignancy was responsible for one-third cases of EHBO. Few studies available from India have investigated the spectrum of EHBO but did not analyze the younger population separately.
In a large prospective study from AIIMS, Delhi1, malignant causes were more common than benign (75.3% vs. 24.7%), and GBC (28.7%) and choledocholithiasis (12.4%) were the most common malignant and benign causes, respectively. Madhu et al.2 observed malignant and benign causes in 63.3% and 36.6%. Verma et al.3 from Meerut studied 110 patients, reporting malignancy in 62.7% and benign causes in 37.2%. In their population, carcinoma head of the pancreas (33.6%) was the most common malignancy. In another study from North India, GBC was the most frequent malignant cause of EHBO9. Selvasekaran et al.10 reported that malignant causes (70%) were more common than the benign cause (30%) with periampullary carcinoma (34%) being the commonest malignancy.
All the above-mentioned studies found malignancy to be the commonest cause of EHBO; however, benign causes were predominant in our study, possibly because we studied only younger individuals, and the incidence of malignancy increases with age. A recent survey by Upadhyay et al.5 in 287 patients reported similar findings to our study (choledocholithiasis (67.9%) followed by malignant stricture (18.12%)). GBC was the most frequent malignant cause of EHBO in most of these studies, like the present study.
Most cases of EHBO were females (67.8%) like those reported by Upadhyay et al.5 (57.7%) and Madhu et al.2 (65.6%). Choledocholithiasis (F=67.3%), GBC (F=72.73%) and benign biliary stricture (F=76.47%) was predominantly seen in females comparable to global trends5,11,12. Periampullary carcinoma (60%) had male preponderance like other studies3,13.
The most common presenting symptoms were jaundice and pain abdomen, which have been reported in 66-88% and 51 to 66% of cases from different parts of the country.3,5 All malignant cases had jaundice at presentation as they were referred primarily for ERCP for biliary drainage. A clinically palpable hard lump was present in 56.8% cases with GBC, and this should be examined routinely with the caveat in mind that its absence doesn’t rule out underlying malignancy.
The mean bilirubin and ALP levels were higher in malignant EHBO cases than benign cases, and the mean bilirubin level in choledocholithiasis (3.83 mg/dL) was like previous studies14. Thus, higher bilirubin levels could be an indicator of malignant pathology in patients with obstructive jaundice. Complete Charcot’s triad may not be present in all patients with cholangitis, and fever or new-onset organ dysfunction in an appropriate clinical setting demands further evaluation. Elevated TLC with a neutrophilic predominance and renal dysfunction could help in identifying patients with cholangitis. GBC patients presented in an advanced stage of the disease, as is common throughout the country, and is associated with poor prognosis.9
Among patients with choledocholithiasis, single calculus was present in 62%, and ERCP achieved biliary clearance in 78.85%, comparable to a previous report by Upadhyay et al.5 Reasons for balloon method failure were large stones (=15 mm), presence of biliary stricture, impacted calculi, and modified anatomy. Biliary stenting for benign biliary stricture was successful in 52.94% cases, and failure was due to tight biliary stricture. Adequate endoscopic biliary drainage was achieved in 68.2% case of GBC, while the rest required percutaneous transhepatic biliary drainage (PTBD). Causes of failure in malignant cases were tight biliary stricture and gastro-duodenal infiltration.
Conclusion
The present study highlights that benign causes, especially CBD stones, predominate in case of extra-hepatic biliary obstruction in younger patients under 40 years of age, and endoscopic therapy is rewarding. Also, malignancy (especially gallbladder carcinoma) contributes to a significant proportion of these cases, even among younger patients. Malignant EHBO cases present with advanced disease and endoscopic palliation is required for mitigating symptoms. Endoscopic palliative therapy has excellent results in most of these patients, and PTBD remains a reasonable alternative.
References
- Sharma MP, Ahuja V. Aetiological spectrum of obstructive jaundice and diagnostic ability of Ultrasonography clinician’s perspective. Trop Gastroenterol. 1999; 20:67–9.
- Madhu MP, Agarwal V, Soni A, Pokharna RK, Nijhawan S, Sharma G et al. Etiological spectrum of extra hepatic biliary obstructive (EHBO) at a tertiary care centre in Northern India. Trop Gastroenterol. 2015;36(2):142–143.
- Verma S, Sahai S, Gupta P, Munshi A, Verma S, Goyal P. Obstructive jaundice-aetiological spectrum, clinical, biochemical and radiological evaluation at a tertiary care teaching hospital. Internet J Trop Med. 2010; Volume 7 Number 2.
- Singh A, Mann HS, Thukral CL, Singh NR. Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. J Clin Diag Res. 2014;8:103–07.
- Upadhyay S, Bhargava R, Rajender A, Singh G, Nepalia S. Clinical Profile of Extrahepatic Biliary Obstruction Cases Undergoing ERCP at an Indian Tertiary Care Centre. J Med Sci Clin Res. 2019;7(5):872-77.
- Bing Hu,Bo Sun, Cai Q, Lau JYW,Ma S, ItoiT et al.Asia-pacific consensus guidelines for endoscopic management of benign biliary stricture. GastrointestEndosc. 2017;86(1).
- Saini S. Imaging of the hepatobiliary tract. N Engl J Med. 1997;336:1889–94.
- Suthar M, Purohit S, Bhargav V, Goyal P. Role of MRCP in differentiation of benign and malignant causes of biliary obstruction. J Clin Diag Res. 2015;9:8-12.
- Vijay S, Gourdas C, Richa S, Vivek AS. Profile of Malignant Extrahepatic Biliary Obstruction at an Indian Tertiary Care Centre: A Dismal Picture. Adv Res Gastroentero Hepatol. 2017;2(4):555-591.
- Selvasekaran R, Nagalakshmi G, Anandan H. Clinical Spectrum of Presentation of Obstructive Jaundice in Inflammation, Stone Disease and Malignancy. Int J Sci Stud 2017;5(4):10-14.
- Randi G, Franceschi S, La Vecchia C: Gallbladder cancer worldwide: Geographical distribution and risk factors. Int J cancer. 2006;118(7):1591-602.
- Sangwan MK, Sangwan V, Garg MK, Singla D, Thami G, Malik P. Gallstone disease menacing rural population in north India: a retrospective study of 576 cases in a rural hospital. Int Surg J. 2015;2(4):487-91.
- Fischer H, Zhou H: Pathogenesis of carcinoma of the papilla of vater. J Hepatobiliary Pancreat Surg. 2004;11:301-309.
- Canto MI, Chak A, Stellato T, Sivak MV Jr. Endoscopic Ultrasonography versus cholangiography for the diagnosis of choledocholithiasis. GastrointestEndosc. 1998;47(6):439-48.