48uep6bbphidcol2|ID
48uep6bbphidvals|2988
48uep6bbph|2000F98CTab_Articles|Fulltext
Squamous cell carcinoma (SqCC) and adenocarcinoma are the most common tumours of esophagus constituting 95 % of primary epithelial neoplasm. Other rare tumours of esophagus are lymphoma, sarcoma, melanoma and neuroendocrine tumours. Neuroendocrine carcinoma (NEC) of esophagus is very rare & constitutes 0.4%-2% of all esophageal carcinomas1,2,3. Esophageal NECs were represent only 0.04-1.4% of the gastrointestinal NECs reported4,5.
Combined tumour of esophagus are very rare neoplasm consisting of two morphologically and immunohistochemically different cell population developing in juxtaposition to each other. Combined tumours of esophagus includes composite tumour,collision tumour,craniosarcomaand amphicrine tumors. Only 24 cases of combined tumour of esophagushave been reported in English literature till 20126. Primary composite tumour of the esophagus is rare and only few cases have been reported in the literature7. Composite tumours have cellular intermingling and a common driver mutation that results in divergent histology from a common source (Pluripotent cell)8. It is difficult to diagnose these composite tumour preoperatively and managing them as both cellular component differ in terms of chemotherapy of choice, response to therapy, and prognosis. NEC is most common reported cellular component in composite tumour and also main important determinant of mortality7. Here we report a case of esophageal composite tumour of NEC and SqCC.
Case Report
49-year female presented to our department with complaints of painless gradually progressive dysphagia since 4 months associated with significant (13 kg) loss of weight and appetite. There were no symptom of gastroesophageal reflux disease. She was non-alcoholic, non-smoker and non-tobacco chewer. No comorbidity was present. Past history of carcinoma left lateral border of tongue was present, for which she underwent partial glossectomy with left supraomohyoid extended neck dissection in 2013. Postoperative biopsy showed moderately differentiated squamous cell carcinoma (PT 1 N0). No adjuvant radiotherapy was taken.
At the time of admission she was cachexic and was able to tolerate semisolid diet. Physical examination and laboratory examination was unremarkable. No evidence of recurrence of previous surgery was noted. She underwent UGIE, which showed ulceroproliferative growth at 30 cm, biopsy of which was suggestive of poorly differentiated squamous cell carcinoma. CECT was done which show concentric mural thickening from D7-D9 vertebra with luminal narrowing. Fat planes with adjacent structures were maintained. FDG PET scan done showed no uptake.
Preoperative diagnosis of squamous cell carcinoma (SCC) of lower esophagus was made and she underwent Hybrid Minimal invasive esophagectomy with feeding jejunostomy. Postoperatively the biopsy reportshowed composite tumour of neuroendocrine carcinoma with squamous cell carcinoma, reaching upto adventitia, resection margins free, no LVI/MVI. 17 lymph node positive out of total 22 lymph node. AJCC TNM Stage pT2N3.
Considering the aggressive neuroendocrine component she received adjuvant chemotherapy based on carboplatin and etoposide, 4 cycles. She developed left adrenal metastasis at 1-year follow up. DOTANOC Scan was done which showed uptake (Suv max 6.6) in left adrenal & Para aortic lymph node (Suv max 2.6). EUS FNAC from left adrenal mass was suggestive of neuroendocrine carcinoma. Serum chromogranin was normal (63 ng/cc).
Discussion
WHO definition of NEC includes positive endocrine markers such as CD56, chromogranin A and synaptophysin with Ki 67 or mitotic index 20% or more9. Small cell type (SCC) NEC are more common (90%) and aggressive than large cell type. It is frequently present at advanced stage with lymph node or distant metastasis10. Most common location of NEC of esophagus is lower one third. Composite tumour is diagnosed based on two morphologically and immunohistochemically different cell in juxtaposition in a same organ with actual cellular intermingling8. Collison tumour has no cellular intermingling. These cellular component might be SqCC, SCC, or adenocarcinoma. They might show two cell (bipartite) or three cell (tripartite) differentiation. New terminology, mixed adeno neuroendocrine carcinoma (MANEC) of Gastrointestinal tract described as tumour, which constitutes at least 30% of NEC and adenocarcinoma component, and its occurrence in the oesophagus, is extremely rare, making it a diagnostic challenge for clinician11.
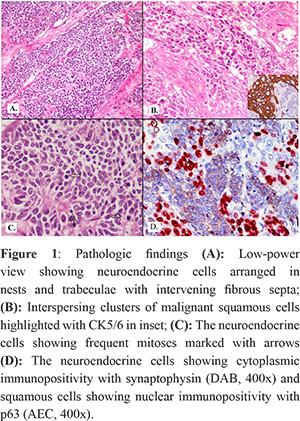
The most widely accepted histogenetic hypothesis for composite tumours of the esophagus is neoplastic transformation of a totipotent primitive cell in the basal region of the squamous mucosa, leading to heterogeneous differentiation within a single tumour12,13. In the present case the close merges between the squamous and small cell carcinoma elements histologically lend support to this hypothesis (Figure 1).
These composite tumour displays highly aggressive behaviour, early disease metastasis, and poor prognosis.It may be difficult to diagnose such composite tumours before esophagectomy because their gross appearance is similar to that of ordinary esophageal cancer and biopsy may not disclose both components because of spatial location. In our case preoperatively it was diagnosed as SqCC. It is well known that aggressive biological behaviour is a characteristic of small cell carcinoma, which typically shows early dissemination and a rapidly fatal course. Although the composite tumours in the present study were composed of squamous cell carcinoma and small cell carcinoma, the clinical behaviour of these tumours is attributed predominantly to the small cell carcinoma components. Patient developed left adrenal metastasis from small cell carcinoma component. Therefore, it is recommended that composite tumours containing small cell carcinoma, even if the volume of this component is small in the primary tumour, should be treated as small cell carcinoma. NEC esophagus has poor prognosis and standard treatment is not well defined due to rarity of tumour.
References
- Huang Q, Wu H, Nie L, et al. Primary high-grade neuroendocrine carcinoma of the esophagus: a clinicopathologic and immunohistochemical study of 42 resection cases. Am J SurgPathol. 2013;37:467–83.
- Kukar M, Groman A, Malhotra U, et al. Small cell carcinoma of the esophagus: a SEER database analysis. Ann Surg Oncol. 2013;20:4239–44.
- Yun JP, Zhang MF, Hou JH, et al. Primary small cell carcinoma of the esophagus: clinicopathological and immunohistochemical features of 21 cases. BMC Cancer. 2007;7:38.
- Estrozi B, Bacchi CE. Neuroendocrine tumors involving the gastroenteropancreatic tract: a clinicopathological evaluation of 773 cases. Clinics (Sao Paulo) 2011;66:1671-5.
- Gastrointestinal Pathology Study Group of Korean Society of Pathologists, Cho MY, Kim JM, et al. Current Trends of the Incidence and Pathological Diagnosis of Gastroenteropancreatic Neuroendocrine Tumors (GEPNETs) in Korea 2000-2009: Multicenter Study. Cancer Res Treat 2012;44:157-65.
- Esophageal combined carcinoma : Immunohistochemical and moleculer genetic studies
- Squamous cell and neuroendocrine carcinoma of esophagus: Collison versus composite tumour: A case report and review of literature
- Collision and composite tumors; radiologic and pathologic correlation Sung CT, Shetty A, Menias CO, Houshyar R, Chatterjee S, Lee TK, Tung P, Helmy M, Lall C.AbdomRadiol (NY). 2017 Dec;42(12):2909-2926. doi: 10.1007/s00261-017-1200-x.
- Rindi G, Arnold R, Bosman FT, Capella C, Kilmstra DS, Klöppel G, Komminoth P, Solcia E. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: IARC Press; 2010. p. 13–4.
- Brenner B, Tang LH, Klimstra DS, Kelsen DP. Small-cell carcinomas of the gastrointestinal tract: a review. J Clin Oncol. 2004;22:2730–9.
- S. La Rosa, A. Marando, F. Sessa, and C. Capella, “Mixed adenoneuroendocrine carcinomas (MANECs) of the gastroin- testinal tract: an update,” Cancers, vol. 4, no. 1, pp. 11–30, 2012. ?
- Ho K-J, Herrera GA, Jones JM, Alexander CB. Small cell carci- noma of the esophagus: evidence for a unified histogenesis. Hum Pathol 1984;15:460–8.
- Ugras S, Akpolat N, Er M, Yalcynkaya I, Karaayvaz M. Primary composite tumor with bipartite differentiation of the esophagus. Acta ChirBelg 2000;100:39–43.