48uep6bbphidcol2|ID
48uep6bbphidvals|2976
48uep6bbph|2000F98CTab_Articles|Fulltext
Colorectal cancer is the third most common malignancy in the world. About 5 % of cases are attributed to hereditary causes with Lynch syndrome being among the commonest. Although the prevalence rate in the Indian subcontinent is comparatively low, the percentage of hereditary cases remains surprisingly the same as worldwide estimates. The lack of awareness and non-existent screening protocols often lead to preventable morbidity in these cases. Here we present a case of hereditary colorectal carcinoma with recurrent malignant lesions and a relatively rare intra-biliary metastasis from colorectal carcinoma.
Case Report
A 35-year-old male patient presented to our hospital with complaints of yellowish discolouration of the eyes and pruritis. He had undergone multiple medical and surgical interventions in the past.
At the age of 20 years, he was detected to have rectal carcinoma with liver metastasis. He underwent neoadjuvant chemotherapy with oxaliplatin and 5-fluoruracil (5FU) followed by low anterior resection and liver metastatectomy. Further, adjuvant therapy in the form of concurrent chemo-radiation was given. The patient, however, failed to follow up after completion of treatment.
He next presented in early 2018, with intestinal obstruction. He was evaluated and found to have an obstructive growth in the middle third of the descending colon with loco-regional and retroperitoneal nodes on CT. Biopsy showed moderately differentiated adenocarcinoma. He underwent limited colectomy with Hartmann’s procedure. Chemotherapy with FOLFOX regimen and cetuximab were started andhe was followed up with regular carcino-embryonic antigen (CEA) monitoring. After an initial decrease in CEA, the levels started to increase again. PET-CT showed FDG avid lymph nodes in and around the coeliac axis. Also, CT scanshowed locally advanced disease with a recurrence in the rectal stump involving the bladder and both pelvic walls.Pembrolizumab therapy was started in view of progressive disease.
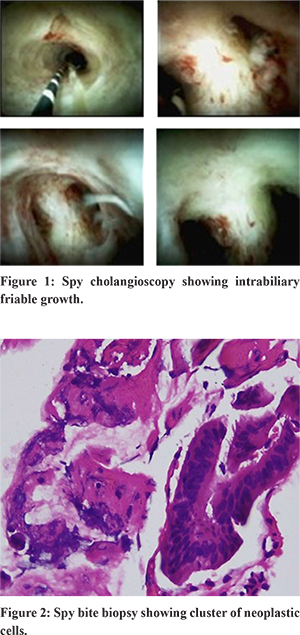
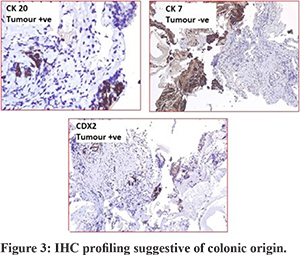
A week after therapy with pembrolizumab, the patient presented with jaundice ; serum bilirubin of 8.5 mg/dl and the direct component of 6.3 mg/dl.Magnetic resonance cholangiopancreatography (MRCP)showed mild intra-hepatic biliary radicle dilation (IHBRD) with ductal disconnection and narrowing of the common bile duct (CBD) and common hepatic duct (CHD) in the upper and middle third. Magnetic resonance imaging (MRI) also showed an ill-defined T2 hyperintense soft tissue lesion encasing the bile duct and portal vein. Spy cholangioscopy (Figure 1) showed erythema and friability in the hilum with prominent vessels. A spybite biopsy was taken. Histopathology of the biopsy specimen (Figure 2) showed fibrous tissue with clusters of neoplastic cells and strips of uniform epithelium. Immunohistochemistry (IHC) profiling (Figure 3) of the biopsy showed it to be CK20+ve, CDX2+ve and CK7-ve which was suggestive of colonic origin. Thus, the diagnosis was modified to intrabiliary metastasis of colonic carcinoma.
The young age and history of multiple carcinomas led to suspicion for an inherited cancer syndrome. Micro-satellite instability (MSI) immunohistochemistry was performed on the blocks available from the previous surgery. It showed loss of MSH-2 and MSH-6. Confirmation genetic testing was done with ClinVarwhich showed mutation in the MSH-2 gene. A detailed family history revealed history of carcinoma stomach in the grandfather and carcinoma colon in the father. A diagnosis of Lynch syndrome was made by the Amsterdam II criteria.
Discussion
Hereditary colorectal cancer (CRC) accounts for around 2 to 5% of all cancer cases in the Western world. Although the incidence of colorectal cancer is relatively low in the Indian subcontinent, the proportion of cases attributed to hereditary causes have been found to be around 10%. Amongst these cases, Lynch syndrome is the leading cause1. Lack of awareness about such conditions often leads to avoidable morbidity and mortality in this population. The age of onset of malignancy is earlier and the lesions are more proximally located in cases of Lynch syndrome. Amongst the extra-colonic malignancies, endometrial cancer is the most common. Other associated cancers are gastric, ovarian, biliary, urinary tract, small bowel, brain and pancreatic.
Amsterdam II criteria and revised Bethesda criteria are used to identify individuals at risk. Diagnosis is confirmed by gene testing. National Cancer Care Network (NCCN) guidelines recommend colonoscopy at age 20 to 25 years or 2 to 5 years prior to the earliest colon cancer if diagnosed before 25 years of age with repeat colonoscopy every 1-2 years. For adenomas detected during surveillance, complete endoscopic polypectomy with follow-up colonoscopy is recommended every 1-2 years. Segmental/ extended colectomy depending on the clinical scenario is to be considered for adenomas not amenable to endoscopy, lesions with high grade dysplasia and adenocarcinomas.
The following six points should be kept in mind to suspect a case of hereditary CRC2.
- Colon cancer diagnosed at < 50 years of age
- Multiple colonic malignancies present, wither synchronous or metachronous
- Multiple primary cancers diagnosed either colonic or extracolonic
- Over a lifetime> 10 adenomas present or > 2 histologically characterised hamartomatous polyps
- Colon cancer in > 1 generation of the individual’s family
- Clustering of extracolonic cancers in family members.
The interesting detail in the above case was the presence of intrabiliary metastasis from the primary cancer. The incidence of colorectal metastasis presenting as intrabiliary growth range from 3.6% to 10.6%3. A review of literature shows multiple case reports of intrabiliary metastasis from colorectal cancer but none in Lynch Syndrome4. The longest duration between initial resection and metastasis as per literature, is 12 years5. In our case, the time duration between initial resection and presentation of the intrabiliary growth was 15 years.
Conclusion
Though the Indian subcontinent has a low incidence of colorectal cancer, the percentage of hereditary cancers are the same as in western population. Early identification, genetic testing and management as per guidelines can help in preventing mortality and morbidity in this group of patients. Our case is one such case in which an initial diagnosis of Lynch syndrome was missed. The diagnosis could only be made after a second tumour was detected. Also, our case showed a gap of 15 years between initial tumourpresentation and intra-biliary metastasis which is the longest reported in literature till date.
References
- Maharaj R, Shukla P, Sakpal S, Naraynsingh V, Dan D, Hariharan S. The impact of hereditary colorectal cancer on the Indian population. Indian Journal of Cancer. 2014;51:538-41.
- Ballester V, Cruz-Correa M. How and When to Consider Genetic Testing for Colon Cancer? Gastroenterology. 2018;155:955-9.
- Estrella JS, Othman ML, Taggart MW, Hamilton SR, Curley SA, Rashid A, et al. Intrabiliary growth of liver metastases: clinicopathologic features, prevalence, and outcome. Am J Surg Pathol. 2013;37:1571-9.
- Coppola S, Zucchini N, Romano F, Bovo G, Gilardoni E, Nespoli L, et al. Colorectal liver metastasis with intrabiliary growth: case report and review of the literature. Int J Surg Pathol. 2014;22:272-9.
- Sasaki S, Nomura Y, Fukutomi S, Shirahama N, Kusano H, Akiba J, et al. Intrabiliary growth type of metastasis from colon cancer, 12 years after curative colectomy: a case report. BMC Surg. 2019;19:8.