48uep6bbphidcol2|ID
48uep6bbphidvals|2968
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Hydatid disease is a parasitic zoonosis caused by the larval stage of Echinococcus granulosus1. The disease is common in the Mediterranean region, Africa, Australia, South America, Middle East, and India2. Liver (50-77%) is the most commonly affected organ followed by lungs (15-47%) and spleen (0.5-8%)1. Pancreatic primary hydatid cysts are rare, with the reported incidence ranging from 0.14% to 2%3. The route of spread, natural history, diagnosis, management, and follow-up of isolated pancreatic hydatid cysts is unclear. There is considerable overlap in the imaging findings, making it difficult to differentiate from other more common cystic neoplasms of the pancreas or pseudocysts4. There are several treatment options, and laparoscopic management of pancreatic hydatid cysts is rarely reported.
Our department is a high volume center for management hepatobiliary diseases. We identified six patients with pancreatic hydatid cyst in our experience of treating 310 cases of hydatid disease and report our surgical experience.
Patients and Methods
We did a retrospective analysis of a prospectively maintained database of all patients with intra-abdominal hydatid disease managed in our department between January 2000 and December 2017.
We treated 310 patients with intra-abdominal hydatid disease during the study period, of which six patients had isolated pancreatic hydatid cyst. All patients were evaluated by detailed history and physical examination. Routine blood investigations included complete hemogram, liver function tests (LFT), serum electrolytes, renal function tests and hydatid serology by enzyme linked immunosorbent assay (ELISA). A chest x-ray and electrocardiogram (ECG) were done as a part of the pre-anesthetic checkup. Radiological evaluation was done by ultrasonography, contrast-enhanced computed tomography (CECT), magnetic resonance imaging (MRI), and magnetic resonance cholangiopancreatography (MRCP), and endoscopic ultrasound (EUS).
All patients underwent surgery and diagnosis was confirmed by histopathology.
Results
During the study period, we treated 310 patients with intra-abdominal hydatid cysts, of which pancreatic hydatid cyst was found in six patients (1.9%), each with a single cyst isolated to the pancreas. The mean age was 35 years (Range:14 to 48 years). Demographic data and pre-operative details are shown in table 1.
Pain was the predominant symptom in all, associated with an abdominal lump in four patients, nausea in 2 patients, and fever in 1 patient. One patient had intracystic bleeding manifested by hematemesis and malena during the hospital course, who underwent emergency surgery. None of the patients had jaundice, pancreatitis, anorexia, or weight loss.
Routine blood investigations including hemogram and LFT were essentially normal, except in the patient with intracystic bleeding who had a decline in hemoglobin level from 9 gm/dL to 6 gm/dL. Hydatid serology by ELISA was positive in three patients. Patients were initially evaluated by ultrasonography, which revealed a well-defined cystic lesion with heterogeneously hyperechoic contents and membrane-like structures within in three patients and a simple cystic lesion in three patients. CECT abdomen showed large well-defined peripherally enhancing thick-walled cystic space-occupying lesion with internal septations (Figure 1) in three patients, and thick-walled simple cyst in 3 patients. (Figure 2)
In the patient with intracystic bleeding, CECT also showed that the cyst’s superior wall was partially encasing the mid-segment of the splenic artery with three wide-necked small outpouchings in inferior wall suggestive of a pseudoaneurysm (Figure 3).
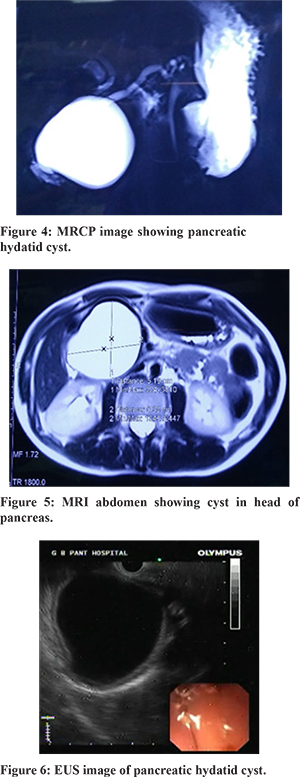
The cyst (maximum diameter) size ranged from 5 to 14 cm (mean diameter-8.8 cm). MRI with MRCP was done in 3 patients, which revealed thick-walled cyst hypointense on T1 and hyperintense on T2 weighted images (Figure 4) and with a hypointense rim and internal serpiginous hypointense structures in 2 patients. The main pancreatic duct (MPD) was prominent in two patients; however, no communication was seen between the MPD and cyst (Figure 5). Upper gastrointestinal (UGI) endoscopy revealed a normal study in two patients, including the one with intracystic bleeding. Endoscopic ultrasound (EUS) performed in two patients was suggestive of cystic lesion, one each in relation to the head and body of the pancreas (Figure 6).
Intraoperative details and follow-up are shown in table 2. After clinical evaluation and preoperative imaging, only three (3/6) patients had features suggestive of hydatid cyst, including the one with intracystic bleeding. After packing the operative field by sponges soaked scolicidal agent, needle aspiration of the cyst fluid was done in three patients, revealing clear fluid which demonstrated hydatid scolices and hooklets. (Figure 10)
Surgical interventions included cysto-pericystectomy, distal pancreatectomy, deroofing and distal pancreatectomy with splenectomy (Figure 7-9) in the open group. In the laparoscopic group, distal pancreatectomy was done in one patient and deroofing with Roux-en-Y cysto-jejunostomy in one patient (Figure 11).
There was no mortality, and one patient with open deroofing developed pancreatic fistula that was managed conservatively, while other patients had an uncomplicated post-operative course. Albendazole was started two weeks before surgery in three patients who had positive hydatid serology, and post-operative albendazole was given to all the patients. The diagnosis was confirmed by biopsy in all the patients, which showed a lamellated membrane (Figure 12) and scolex (Figure 13) typical of hydatid cyst. Mean follow-up duration is 41.5 months (ranging from 3 - 84 months) with all patients doing well without recurrence.
Discussion
The majority of cystic lesions in the pancreas are pseudocysts (80%) followed by cystic neoplasms (10%), and hydatid cysts are a rare cause of cystic lesion of pancreas.5 Pancreas is one of the most unusual sites of extrahepatic hydatid disease, with the reported incidence ranging from 0.14% to 2%3. The majority of the pancreatic hydatid cysts are solitary (92%) and isolated to the pancreas in 72% of patients. They are commonly seen in the head of the pancreas (50%-58%), followed by the body (24%-34%) and pancreatic tail (16%-19%)6. We report a similar prevalence (1.9%) and isolated single character of the cyst. However, in contrast to other studies, the cyst was more often situated in the body and tail of the pancreas.
There are many proposed mechanisms of pancreatic infestation of hydatid disease (Flow chart 1).
The most accepted mechanism is by hematogenous dissemination. Other proposed mechanisms include local spread by passage of cystic elements via bile duct to the pancreatic duct7, the direct passage of cystic components through the intestinal mucosa into peripancreatic lymphatic plexus, and retroperitoneal spread8. The parasitic embryos which penetrate the intestinal wall enter the portal circulation and are trapped in hepatic sinusoids leading to hepatic hydatidosis, the most common site (first Lemman’s filter). The larvae (=0.3 mm diameter)might escape the liver filter and reach the lung, where they are entrapped by lung capillary filter, the second most common site (second Lemman’s filter). Larvae that escape the lung may then pass to any part of the human body via arterial circulation leading to systemic hydatid disease.7
Javed et al.9 have suggested the possibility of an association between HIV and liver hydatid, especially in large or multifocal cysts. However, it is unclear whether extrahepatic hydatid cysts such as pancreatic cysts are associated with immunocompromised states. None of the patients had immunocompromised states in our study.
Few patients may remain asymptomatic for years before attaining a sufficient size to cause symptoms and often are incidentally diagnosed. The rate of growth of pancreatic cysts is 0.3 to 2 cm per year10. In the present study, the average size of the cyst was 7.8 cm (ranging from 4 to 10cm). Clinical manifestations may vary depending on the location of the cyst within the pancreas. Those located in the head region may present with jaundice due to compression of the CBD11 and may mimic like a choledochal cyst12 on imaging similar to our patient (case 6). Cysts located in the body and tail of the pancreas may present with abdominal pain, lump, nausea, and vomiting due to compression of adjacent structures3. Other reported symptoms and complications are splenomegaly with portal hypertension, cholangitis, rupture into the biliary tree or peritoneal cavity, recurrent pancreatitis, pancreatic fistula, and abscess13. In our study, one patient had non-bilious vomiting and upper GI bleeding with splenic artery pseudoaneurysm and intracystic bleeding, which has not been reported in the literature.
Although ultrasonography is the most commonly used imaging technique for the diagnosis of liver hydatid cysts, CT, and MRI are widely used to evaluate cystic lesions of pancreas and extrahepatic hydatid cysts14. Multidetector computed tomography (MDCT) is the most common imaging technique for assessing pancreatic cysts15. Many imaging findings are classical of hydatid cysts, usually described in the context of the liver or lung. The typical characteristic features of liver hydatid are affected by the stage of the cyst. It can present as a simple cyst, double echogenic lines separated by a hypoechogenic layer, hydatid sand, echogenic foci lying in the dependent part of the cavity(snowstorm sign), detached endocyst from the pericyst partially (floating membranes) or completely (water lily sign), multivesicular cysts (honeycomb pattern), calcification of cyst wall, or a solid mass (when the matrix fills the cyst)16.
Characteristic imaging findings of hydatid cysts are often missing in pancreatic hydatid, with considerable imaging overlapping between other cystic lesions making pre-operative diagnoses difficult. Makni et al. concluded that pre-operative diagnosis of pancreatic hydatid cysts is challenging compared to different locations,17. In another study, only 40%-49% of patients with pancreatic hydatid were diagnosed preoperatively6. In our study also, we could diagnose the lesion accurately only in three patients (50%).
Hydatid serologic tests are based on Antibody detection by reaction and precipitation of the test antigen and the circulating antibodies in the host. Sensitivities for enzyme-linked immunosorbent assay (ELISA)vary from 85% to 98% for hepatic hydatid18, whereas sensitivity and specificity of pancreatic hydatid cysts are 54% and 62% respectively6. In our study, hydatid serology was positive in only three patients (50% sensitivity). Interestingly, only patients with positive hydatid serology had imaging features suggestive of hydatid cyst and could be diagnosed preoperatively.
Another diagnostic tool commonly used in the evaluation of cystic pancreatic lesions is EUS. Some authors recommend a fine-needle aspiration biopsy to differentiate a hydatid cyst from other common cystic lesions19. In contrast to FNAC and cyst fluid for analysis, it can also depict the relationship of the cyst with MPD and adjacent vessels. However, it is operator dependent and available only in high-volume centers. In the present study, EUS in two patients showed a cystic lesion, with one cyst in the head region mimicking a choledochal cyst, and EUS guided cyst fluid analysis was not done in any of our patients.
Treatment options for pancreatic hydatids include medical therapy, percutaneous technique (PAIR or direct percutaneous catheterization), surgery, or combination of these techniques. Modality selection depends on the location of the cyst, type of cyst, associated complications, and surgeon’s experience.20
PAIR (puncture, aspiration, injection, and re-aspiration) has been described as an alternative to surgical management of simple cysts21. In our previous study of hepatic hydatidosis22, we concluded that percutaneous drainage (with PAIR/PAIR-D) is preferred in type I and II cysts and surgery in others. However, the risk of peritoneal seeding (more than that of a solid organ like liver and spleen)23 or tumor cells remain, and it is ineffective for multiloculated cysts. PAIR is limited to a small number of patients with pancreatic hydatid as confirmation of the diagnosis and appropriateness of treatment are best achieved during surgery in the majority4,24.
Various surgical procedures have been described, mainly as open procedures, including distal pancreatectomy for distal body and tail lesions, drainage, and cysto-jejunostomy25, central pancreatectomy, cysto-pericystectomy for proximal body and neck lesions. Those in the head region have been treated by marsupialization and external drainage, partial cystectomy, cyst-enteric anastomosis, and pancreaticoduodenectomy when there was a diagnostic uncertainty24. Javed et al. performed cysto-jejunostomy to avoid post-operative pancreatic fistula after drainage of pancreatic hydatid cyst in the region of the neck and proximal body of pancreas, with excellent post-operative outcome. We believe that Roux en Y cysto-jejunostomy should be done in all patients undergoing surgical drainage, as it can avoid any post-operative pancreatic fistula without increasing morbidity. Besides, timely intervention is necessary to prevent life-threatening complications. In our patient with intracystic bleeding, emergent timely laparotomy with distal pancreatectomy and splenectomy was curative and avoided a major catastrophe of pseudoaneurysm rupture.
Although there are numerous articles about laparoscopic management of hydatid cysts in other organs22, there are only a few case reports on the use of the laparoscopic approach for pancreatic hydatid. In one report, the content of a cyst located in the pancreatic head was emptied by directly inserting a 10 mm trocar into the cyst, followed by omentoplasty26. Two patients in our study were managed laparoscopically by distal pancreatectomy in one patient and deroofing followed by Roux En Y cysto-jejunostomy in one patient with uneventful post-operative recovery. To the best of our knowledge, both distal pancreatico-splenectomy for intracystic bleeding and laparoscopic management of pancreatic hydatid cyst by Roux En Y cysto-jejunostomy has not been reported in the literature. Our center being a tertiary care referral center for hepato-pancreato-biliary disease with vast experience of managing these patients by laparoscopic surgery22,27, we believe that laparoscopic surgery is feasible and safe in patients with pancreatic hydatid cyst.
Pancreatic hydatid cysts in the perioperative period, atleast four days before surgery, should be started on anti-helminthic drugs (albendazole, mebendazole, or praziquantel) to reduce anaphylaxis and post-operative recurrence risks28. Also, these patients should be followed up at regular intervals to detect any recurrence.
Conclusion
Isolated pancreatic hydatid cyst is rare, and its preoperative diagnosis is challenging. However, it should be kept in the differential diagnosis of cystic lesion of the pancreas, especially in patients from endemic areas. Timely intervention may avoid fatal complications. Laparoscopic surgery is feasible and safe, and cysto-enteric drainage may prevent the formation of pancreatic fistula.
References
- S. Akbulut, et al., Hydatid cyst of the pancreas: report of an undiagnosed caseof pancreatic hydatid cyst and brief literature review. World J. Gastrointest.Surg. 6 (10) (2014) 190–200.
- S. Sharma, et al., Endoscopic ultrasound-guided FNA: emerging technique todiagnose hydatid cyst of pancreas. J. Cytol. 32 (3) (2015) 211–212.
- O.J. Shah, et al., Hydatid cyst of the pancreas. An experience with six cases.JOP 11 (6) (2010) 575–581.
- Shah OJ, Robbani I, Zargar SA, Yattoo GN, Shah P, Ali S, et al. Hydatid cyst of the pancreas. An experience with six cases. Jop J Pancreas. 2010;11(6):575–81.
- Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C, Warshaw AL. Cystic Neoplasms of the Pancreas. N Engl J Med. 2004;351(12):1218–26.
- Sami Akbulut et al. Hydatid Cyst of the Pancreas: Report of an Undiagnosed Case of Pancreatic Hydatid Cyst and Brief Literature Review World J Gastrointest Surg 2014 October 27; 6(10): 190-200
- Wani RA, Wani I, Malik AA, Parray FQ, Wani AA, Dar AM. Hydatid disease at unusual sites. Int J Case Reposts Images 2012; 3: 1-6.
- Mandelia A, Wahal A, Solanki S, Srinivas M, Bhatnagar V. Pancreatic hydatid cyst masquerading as a choledochal cyst. J Pediatr Surg 2012; 47: e41-e44
- Javed A, Kalayrasan R, Agarwal AK. Liver Hydatid with HIV Infection: an Association? J Gastrointest Surg (2012); 16:1275–1277
- Eris C, Akbulut S, Yildiz MK, Abuoglu H, Odabasi M, Ozkan E, Atalay S, Gunay E. Surgical approach to splenic hydatid cyst: single center experience. Int Surg 2013; 98: 346-353
- Z. Turkyilmaz, et al., Obstructive jaundice resulted from hydatid cyst ofpancreatic head. Hippokratia 17 (4) (2013) 378–379.
- A. Mandelia, et al., Pancreatic hydatid cyst masquerading as a choledochalcyst. J. Pediatr. Surg. 47 (11) (2012) e41–e44
- P. Szanto, et al., Hydatid cyst of the pancreas causing portal hypertension.Maedica (Buchar) 5 (2) (2010) 139–141.
- Safioleas M, Misiakos E, Manti C (1997) Surgical treatment for splenic hydatidosis. World J Surg 21:374–378
- Allen PJ, et al: A selective approach to the resection of cystic lesions of the pancreas: results from 539 consecutive patients. Ann Surg 244:572–582, 2006.
- Davolio SA, Canossi GC, Nicoli FA, et al. Hydatid disease: MR imaging study. Radiology 1990;175:701–706
- Makni A, Jouini M, Kacem M, Ben Safta Z. Extra-hepatic intra-abdominal hydatid cyst: which characteristic, compared to the hepatic location? Updates Surg 2013 65:25–33
- Brunetti E, et al: Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114:1–16,2010
- Ugras S, Sakarya ME, Arslan H, Bozkurt M, Akdeniz H. The diagnosis by fine needle aspiration biopsy of hydatid cyst of the pancreas. Acta Chir Belg. 1997 Oct;97(5):244–6.
- Trigui A, Rejab H, Guirat A, Mizouni A, Amar MB, Mzali R, Beyrouti MI. Hydatid cyst of the pancreas About 12 cases. Ann Ital Chir 2013;84(2):165-70.
- Yattoo GN, Khuroo MS, Zargar SA, Bhat FA, Sofi BA. Case report: Percutaneous drainage of the pancreatic head hydatid cyst with obstructive jaundice. J Gastroenterol Hepatol. 1999 Sep;14(9):931–4.
- Gupta N, Javed A, Puri S, Jain S, Singh S, Agarwal AK. J Gastrointest Surg 2011; 15:1829–1836
- Derbel F, Zidi MK, Mtimet A. Hydatid cyst of the pancreas:A report on seven cases. AJG 2010; 11: 219-222
- Bansal VK, Misra MC, Krishna A, Kumar S, Garg P, Khan RN et al. Pancreatic hydatid cyst masquerading as cystic neoplasm of pancreas. Trop Gastroenterol. 2011 Feb 14;31(4):335–7.
- Javed A, Pal S, Chaubal GN, Dash NR, Garg PK, Sahni P, et al. Unusual cystic lesion of the pancreas. JOP 2010 Jul 5;11(4):401-2.
- Suryawanshi P, Khan AQ, Jatal S. Primary hydatid cyst of pancreas with acute pancreatitis. Int J Surg Case Rep 2011; 2:122-124
- Agarwal AK, Javed A, Kalayarasan R, Sakhuja P. Minimally invasive versus the conventional open surgical approach of a radical cholecystectomy for gallbladder cancer: a retrospective comparative study. HPB. 2015 ;17(6):536-41.
- Szanto P, Goian I, Al Hajjar N, Badea R, Seicean A, Manciula D, Serban A. Hydatid cyst of the pancreas causing portal hypertension. Maedica (Buchar) 2010; 5: 139-141.