48uep6bbphidcol2|ID
48uep6bbphidvals|2949
48uep6bbph|2000F98CTab_Articles|Fulltext
Benign recurrent intrahepatic cholestasis (BRIC) and acute viral hepatitis (AVH) are two examples of conditions that can result in intrahepatic cholestasis. Antihistaminics and cholestyramine are generally used for managing pruritus. Some cases have severe pruritus refractory to all medical therapies. Pruritus may be associated with severely impaired quality of life and inability to sleep. We present two cases of BRIC and one case of AVH in which the patients had pruritus refractory to medical therapy.
Case Series
Case 1: A 40-year-old male presented with yellow discoloration of eyes and high colored urine associated with severe pruritus for 2 weeks. A liver biopsy was done after negative viral and autoimmune markers. The liver biopsy showed bland cholestasis consistent with BRIC. As the patient had severe pruritus refractory to medical therapy with impaired quality of life, the option of NBD was discussed, and NBD placement was done.NBD was removed subsequently after 3 weeks at a Bilirubin level of 5.5 mg/dl. No complication was noted.
Case 2: A 32-year-old male with history of cholestatic jaundice twice in past, presented with 2 weeks history of jaundice and severe pruritus with consequent insomnia and impaired quality of life. Liver biopsy showed bland cholestasis consistent with BRIC. The option of NBD was discussed in view of severe pruritus refractory to medical therapy. NBD was removed subsequently after 16 days at a Bilirubin level of 20.6 mg/dl. No complication was noted.
Case 3: A 27-year-old male diagnosed with acute hepatitis A infection had prolonged cholestasis for 8 weeks and presented with severe pruritus refractory to medical management. NBD placement was done at bilirubin level of 42.3 mg/dl. The patient had fever after NBD placement, which improved on antibiotics. NBD was removed subsequently after 1 month at a bilirubin level of 18.5 mg/dl.
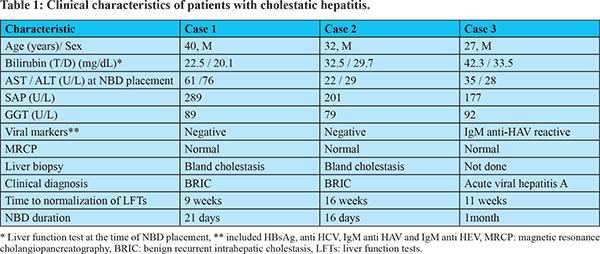
These patients received ursodeoxycholic acid, hydroxyzine and cholestyramine. One patient also received naltrexone and steroids. These patients presented four to 8 weeks after the onset of jaundice with increasing bilirubin levels and pruritus refractory to medical therapy. All patients were seen at several sites before coming to our center; however, none of them had previously been offered the option of naso-biliary drainage. In our centre, the potential complications of ERCP were explained and the alternative of NBD was given to the patient. A 7 Fr NBD was placed after selective cannulation of the common bile duct. Endoscopic papillotomy was not done since it would have increased the procedure-related risk of pancreatitis. Table 1 shows the clinical and biochemical parameters of 3 patients. All the three patients had negative work up for underlying auto-immune disease (anti-nuclear antibody, anti-mitochondrial antibody, anti-smooth muscle antibody, and anti-liver kidney microsomal antibody). MRCP showed normal appearance of the biliary tree in allpatients. All the patients had remarkable improvement of pruritus after 48 to 72 hours of NBD insertion.
Discussion
Bile salts are the main agents thought to cause pruritus associated with jaundice. Biliary drainage is the most effective treatment for pruritus and itching subsides very soon following NBD placement. The relief in pruritus occurs prior to a significant decrease in serum bilirubin concentration. Several pharmacological agents have been tried; however, occasionally, pruritus remains refractory to these medications.1,2 NBD interrupts the entero-hepatic circulation of bile salts and leads to improvement of pruritus. Stapelbroek et al used NBD in 3 patients with BRIC associated pruritus and demonstrated improvement within 24 hours.3
Singh et al used NBD in six patients with cholestatic acute viral hepatitis and intractable pruritus prospectively. The authors noted that naso-biliary drainage hastened the recovery in these patients.4 Hedage et al analyzedretrospective data from five European centres. Pruritus was quantified using a visual analogue scale (VAS). 27 patients (59% females) underwent 29 nasobiliary drainage procedures. The median duration of NBD was 7 days. NBD decreased pruritus in 89.6% of cases (VAS from 10.0 to 0.3, p< 0.0001). The median percentage decline in pruritus was 94% and 33% of patients were free of pruritus within 24 hours. The duration of treatment response was independent of duration of drainage and bile output. The authors also noted significant improvements of serum alkaline phosphatase and serum bilirubin.5 Yakar et al used NBD in 16 patients (25 NBD procedures) with BRIC and refractory pruritus while 17 patients were managed by medications. The authors noted longer clinical remissions in the NBD group.6 It is important to note that ERCP can lead to pancreatitis. Mild post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis occurred in 31% of cases in series by Hedage et al.5 Yakar et al also noted pancreatitis in one out of 16 patients.6 A small size NBD catheter and avoidance of papillotomycan decrease risk of ERCP associated pancreatitis.7
Conclusion
We have presented above a series of 3 cases with refractory pruritus secondary to intrahepatic cholestasis, all of whom had remarkable improvement after NBD placement. NBD can be a very useful modality in such cases but it is rarely used due to lack of awareness.
Acknowledgements: Mr Yogesh Saini (research coordinator)
Funding: none.
Conflict of interest: none
References
- Bassari R andKoea JB. Jaundice associated pruritis: A review of pathophysiology and treatment. World J Gastroenterol. 2015; 21: 1404–1413.
- Levy C. Management of Pruritus in Patients with Cholestatic Liver Disease. Gastroenterol Hepatol (N Y). 2011;7:615–617
- Stapelbroek JM, van Erpecum KJ, Klomp LW et al. Nasobiliary drainage induces long-lasting remission in benign recurrent intrahepatic cholestasis. Hepatology. 2006;43:51-3
- Singh V, Bhalla A, Sharma N, Dheerendra PC, Agarwal R, Mahi SK. Nasobiliary drainage in acute cholestatic hepatitis with pruritus. Dig Liver Dis. 2009;41:442-5
- Hegade VS, Krawczyk M, Kremer AE et al. The safety and efficacy of nasobiliary drainage in the treatment of refractory cholestatic pruritus: a multicentre European study. Aliment PharmacolTher. 2016;43:294-302
- Yakar T, Demir M, Gokturk HS et al.Nasobiliary Drainage for Benign Recurrent Intrahepatic Cholestasis in Patients Refractory to Standard Therapy. Clin Invest Med. 2016;39:27522.
- Ishigaki T, Sasaki T, Serikawa M, et al. Comparative study of 4 Fr versus 6 Fr nasobiliary drainage catheters: a randomized, controlled trial. J Gastroenterol Hepatol 2014; 29: 653–9.