48uep6bbphidcol2|ID
48uep6bbphidvals|1908
48uep6bbph|2000F98CTab_Articles|Fulltext
The surgical treatment for disconnected pancreatic duct is difficult, even in the elective setting. Here we describe a case of DPDS wherein emergency surgery was required. This report aims to highlight the clinical and technical nuances of this tricky situation.
Case Report
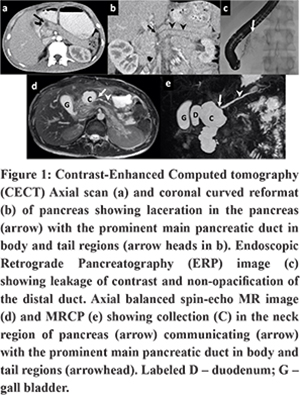
An 18 year-old male was referred to our hospital after having undergone an emergency laparotomy for blunt abdominal trauma two months prior, at another hospital, with the details of the procedure and operative findings being unavailable. He was emaciated (Weight:35 Kg, BMI:14.4kg/m2) and had a high output fistula (600 ml/day) from the midline wound. The patient was evaluated under the department of gastroenterology, where he was found to be having disconnected pancreatic duct syndrome (DPDS). An Endoscopic Retrograde Pancreatography (ERP) with trans-papillary pancreatic duct stenting was performed. ERP showed leakage of contrast at the level of the neck of pancreas, and the distal duct was not opacified (Figure 1). The fistula output remained high even after transpapillary stenting. As the patient was malnourished and was in poor general condition, he was started on nasojejunal feeds and was given injection octreotide for 10 days. Following this, the fistula output decreased to less than 200 ml/day, and the patient was discharged on oral feeds. The fistula output further decreased to around 10 ml/day over the next 2 weeks. Around 4 weeks later, the patient presented with a gradually increasing lump in the upper abdomen. On further evaluation with Magnetic resonance imaging (MRI), the lump was found to be a pancreatic pseudocyst (Figure 1) for which an endoscopic ultrasound (EUS) guided transmural drainage was done (at 4 months after the injury and 2 months after the trans-papillary stenting). However, soon after the procedure, the patient worsened with severe pain, tachycardia, and hypotension. On abdominal examination, the epigastric lump had disappeared, and there was diffuse tenderness. He was diagnosed with ruptured pseudocyst with peritonitis and taken for emergency surgery after resuscitation.
At laparotomy, there was around 300 ml of serosanguinous fluid in the peritoneal cavity with moderate adhesions. Anterior wall of the pseudocyst, between the stomach and the colon, was thin and flimsy and had a defect through which the cyst contents had escaped into the peritoneal cavity. The stent was seen entering into the cyst through the posterior wall of the stomach. (Figure 2a). After opening the lesser sac, the pancreas was found to be entirely transected with a gap of 2 cm between the proximal and the distal parts. The thin anterior wall of the pseudocyst was excised, and the cyst wall dissected off from the posterior wall of the stomach superiorly and the transverse mesocolon inferiorly. The stent protruding through the posterior wall of the stomach was removed and the gastric opening repaired in two layers. The ductal opening in the distal pancreas was not visible and could be identified only after excavating the parenchyma, analogous to the technique1 used to locate the duct during surgery for chronic pancreatitis in patients with small ducts. The duct was then opened longitudinally for 3 cm and a Roux-en Y cysto-pancreatico-jejunostomy performed incorporating the remaining cyst cavity into the anastomosis as shown in Figures 2b & 2c. As the transected end of the pancreas was unhealthy, longitudinally opening the duct allowed us to anastomose to the healthy distal part of the pancreas.Ductal opening in the proximal pancreas was not sought as the normal passage was intact and papillotomy and stenting had already been done. A single drain was placed near the anastomosis.
Post-operative recovery was uneventful. The nasogastric tube was removed on post-operative day (POD) 3, and oral feeding resumed on POD 4. Drain output was only 50 ml/day but the drain fluid amylase was high (1477 IU/ml). The patient was discharged on POD7 with drain in-situ that was subsequently removed 4 weeks after the surgery since the output was nil for 3 consecutive days. The patient was doing well (weight: 40 Kg, BMI: 16.4) and had no exocrine or endocrine insufficiency at 6 months after surgery.
Discussion
DPDS typically occurs as a result of severe acute necrotizing pancreatitis or abdominal trauma.2 Most cases (around 75%) are managed with endoscopic therapy, but surgical intervention may be required.3,4 Surgical options include resection of the distal pancreatic segment or internal drainage.2 Resection may be the best option for transection at the level of the distal body that results in a small unhealthy distal segment, which may be sacrificed without consequences. Internal drainage is an attractive option in patients with a sizeable distal segment and has been shown to be associated with lesser operative time, blood loss, transfusion requirement, and hospital stay compared with resection.5
A few small series have reported a success rate of up to 90%.2
It needs to be emphasized that most of the patients in the series mentioned above were operated in the elective setting. Our patient had to be operated in an emergency setting for peritonitis. There was uncontrolled rupture of the cyst into the peritoneal cavity, and the posterior gastric wall had been breached. Resection was avoided as the transection at the neck of pancreas resulted in a sizeable distal segment. Internal drainage is a risky option in the emergency and should be considered only after careful clinical assessment of the intra-abdominal milieu. Creating a pancreatico-enteric anastomosis in the setting of inflammation and friable tissues can be disastrous as the leakage of enteric contents may result in severe septic complications. In such situations, external drainage may be the best option to tide over the initial crisis, and pancreatic leakage may be dealt with at a later date electively when the local inflammation has settled. We chose to do internal drainage as our patient was stable, and the surgery was performed within 6 hours of cyst rupture due to which there was minimal contamination, and the tissues were not inflamed or friable.
References
- Izbicki JR, Bloechle C, Broering DC, Kuechler T, Broelsch CE. Longitudinal V-shaped excision of the ventral pancreas for small duct disease in severe chronic pancreatitis: prospective evaluation of a new surgical procedure. Ann Surg. 1998; 227: 213–219.
- Nadkarni NA, Kotwal V, Sarr MG, Swaroop Vege S. Disconnected Pancreatic Duct Syndrome: Endoscopic Stent or Surgeon’s Knife? Pancreas. 2015; 44: 16–22.
- Devière J, Bueso H, Baize M, Azar C, Love J, Moreno E, et al. Complete disruption of the main pancreatic duct: endoscopic management. GastrointestEndosc. 1995; 42: 445–451.
- Varadarajulu S, Wilcox CM. Endoscopic placement of permanent indwelling transmural stents in disconnected pancreatic duct syndrome: does benefit outweigh the risks? GastrointestEndosc. 2011; 74:1408–1412.
- Howard TJ, Rhodes GJ, Selzer DJ, Sherman S, Fogel E, Lehman GA. Roux-en-Y internal drainage is the best surgical option to treat patients with disconnected duct syndrome after severe acute pancreatitis. Surgery. 2001; 130: 714-719-721.