|
Dibya Jyoti Sharma, Vishal Sharma, Sobur Uddin Ahmed, Ravi K Sharma, Rajesh Gupta, Surinder S Rana Department of Gastroenterology and Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Corresponding Author:
Dr Vishal Sharma Email: docvishalsharma@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.510
48uep6bbphidcol2|ID 48uep6bbphidvals|1894 48uep6bbph|2000F98CTab_Articles|Fulltext Dengue is a mosquito-borne viral infection which is endemic in tropical and subtropical countries.Reports of dengue fever (DF) and dengue hemorrhagic fever (DHF) presenting with atypical manifestations due to hepatic, renal, cardiac or nervous system involvement (expanded dengue syndrome) are available in literature.1,2 Acute pancreatitis is avery infrequently reported complication of DF and the published literature is in the form of case report or small case series.3-20 We report a case of acute pancreatitis complicating dengue fever and review the published literature on acute pancreatitis related to dengue and its course and outcomes.
Case Report
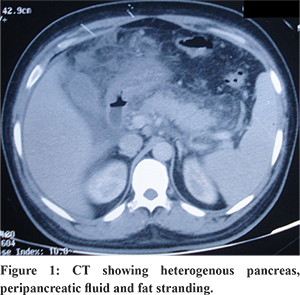
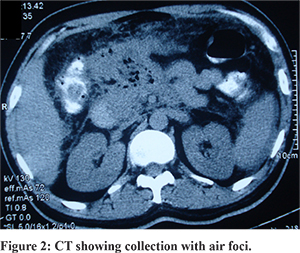
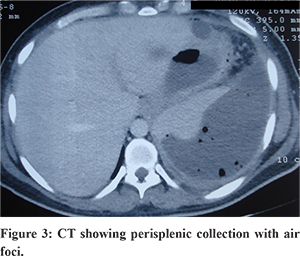
A 32 years old male patient presented with sudden onset severe epigastric pain with radiation to back lasting for six days. Pain abdomen was associated with 2-3 episodes of vomiting at the onset. Subsequently he developed abdominal distension and decreased bowel movements. Four days prior to the onset of pain abdomen patient had developed high grade fever with rigor which was associated with malaise, bodyache and headache. Patient denied any co-morbidities or any history of trauma. Patient was treated conservatively by a local physician with intravenous fluids, antipyretics (paracetamol) and fever subsided within 4 days. During the work up for fever dengue serology and serum NS1 antigen were found to be positive and work up for other causes of febrile illness including viral hepatitis (IgM Anti HAV, IgM Anti-HEV, HBsAg, IgMantiHbc, and Anti-HCV), malaria (peripheral smear and parasite lactate dehydrogenase antigen test), enteric fever (blood culture and Widal test), and scrub typhus (PCR for scrub typhus) were non-contributory. On physical examination at emergency patient had mild tenderness in epigastrium and left hypochondrium with abdominal distension. His bowel sounds were sluggish; sensorium and vitals were within normal limits and was afebrile. He had enlarged palpable liver on abdominal examination. In view of elevated serum amylase (1184 IU/L: Normal <100 U/L) along with abdominal pain a diagnosis of acute pancreatitis was made. On investigations patient was found to have thrombocytopenia (platelet-90000/mm3) whereas the rest of his hematological parameters were normal. Patient had normal renal function tests (urea 27 mg/dL, serum creatinine 0.8 mg/dL) whereas he had mild hypertransaminesemia (AST 61U/L, ALT 48U/L) and low albumin (2.8 gm/dL). Ultrasound (USG) abdomen revealed bulky pancreas with moderate ascites, normal gall bladder without calculi or sludge. Rest of the etiological work up including lipid profile, serum calcium, USG neck to rule out parathyroid adenoma, IgA anti tissue transglutaminaselevels were unremarkable. Patient’s ascitic fluid was tapped which was suggestive of low serum ascites albumin gradient (0.2 gm/dL) with elevated fluid amylase at 1139 IU/L. His initial contrast enhanced computed tomography (CECT) revealed heterogenously enhancing pancreas with peri-pancreatic fat stranding with a peripherally enhancing loculated collection in the lesser sac suggestive of acute pancreatitis (Figure 1). Patient was managed conservatively within intravenous fluids, analgesics and was allowed oral feeding after his pain subsided. As he had no organ failure and tolerated oral feed well, he was discharged after 7 days in stable condition. However, six weeks post discharge patient again developed repeated episodes of non projectile vomiting associated with increased abdominal pain followed by high grade fever and shortness of breath. A repeat CECT abdomen showed heterogenously enhancing pancreas with acollection in the lesser sac with air foci (Figure 2). In view of worsening sepsis he was started on broad spectrum antibiotics, oxygen inhalation and a 10F pigtail was inserted in the lesser sac collection which drained pus. Few days later he again started developing respiratory distress and sepsis and started to worsen for which CECT abdomen was done which showed presence of a large collection in splenic subcapsular region with air foci (Figure 3). Subsequently two additional 10 Fr pigtail catheters were inserted, one in left pleural effusion and another in the peri-splenic region, which drained purulent material. The patient symptomatically improved and the drain output in the pigtails reduced and eventually over two weeks these catheters were removed one by one. Patient improved to the above management and was discharged in a healthy state about two months after admission.
Discussion
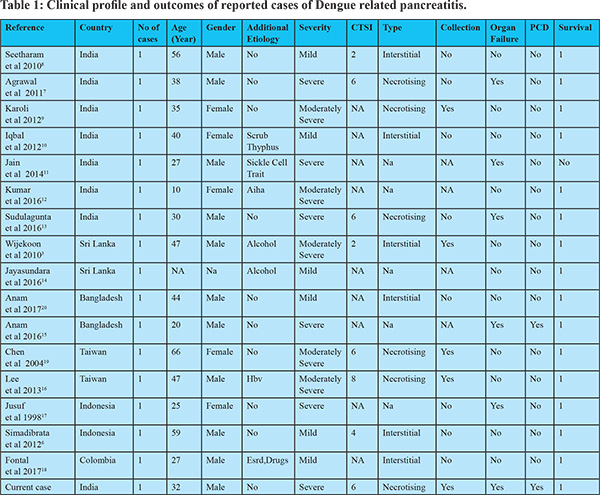
Although various gastroenterological symptoms are frequent in dengue, dengue is deemed to be an uncommon cause of acute pancreatitis.21-23 In a retrospective study of 8,559 patients with dengue fever, abdominal and gastrointestinal symptoms were present in 67% patients. Nausea (52%) was the most common symptom followed by abdominal pain (36%) and vomiting (29%).22 In dengue fever, abdominal pain can be caused by hepatitis, acalculouscholecystitis, pancreatitis or peptic ulcer disease.2,21-23 Khanna et al reported about 55 patients with dengue and abdominal pain from Delhi, India and found that common causes of pain were hepatitis in 20 (36.4%), cholecystitis in 9 (16.4%), pancreatitis in 8 (14.5%) and appendicitis in 3 (5.45%) while spontaneous bacterial peritonitis, enteritis, peptic ulcer and gastric erosions were other causes.21 We did a Pubmed search for “Dengue” AND “pancreatitis” in March 2017 and could retrieve 16 published cases of dengue related pancreatitis with full clinical details on course and outcomes. The clinical spectrum and outcomes in these 17 patients (including our case) are reported in Table 1. Majority of the reported cases were from Southeast Asian countries like India, Bangladesh, Taiwan and Indonesia as dengue is widely prevalent in these regions. Of these 17 cases, 11 were males (64.7%). The average age of the patients in these reports was 37.68 years (10-66 years). Among additional etiologies, alcohol intake was noted in two patients while other associated etiologies being end stage renal disease, drugs, hepatitis B and scrub typhus co-infection. When disease severity was analyzed (as per revised Atlanta definitions), six patients (35.3%) were noted to have mild disease, five (29.4%) had moderately severe and six (35.3%) had severe pancreatitis. Of the 12 patients in whom details were provided, six each had interstitial and necrotising disease. Of these patients five developed fluid collections related to pancreatitis and two needed interventions in the form of drainage. Organ failure developed in six patients with renal failure in two, respiratory in four and two had circulatory failure. None of the patients had undergone surgery while percutaneous drain (PCD) was inserted in two patients. One patient died due to circulatory and renal failure.
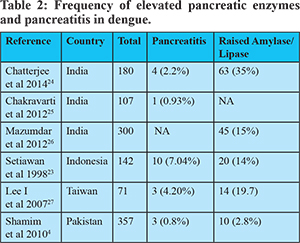
Further, some observational studies documented the occurrence of pancreatitis and lipase/amylase elevation in patients with underlying dengue fever (Table 2).4,23-27 The incidence of pancreatitis was reported from 0.8%-7.04% in various reports whereas the frequency of elevated pancreatic enzymes (amylase or lipases) was higher (2.8-35%). Most of these studies have not reported about the mortality and outcomes in these patients thereby making interpretation of the severity difficult. In one report the authors sought to look for enlargement of pancreas on ultrasound and found that this finding is fairly common. Of a total 142 cases, diffuse pancreatic enlargement was documented in 41 patients (28.8%) of whom 20 (14.1%) had elevated amylase levels.23
Acute pancreatitis may be under diagnosed as a manifestation of dengue due to lack of awareness and it is likely that mild forms without any local and systemic complications may be missed. Therefore, clinicians might not request serum amylase or lipase or suspect the diagnosis despite patient having abdominal pain or vomiting. In patients with dengue fever who develops abdominal pain, it is helpful to estimate and monitor serum lipase and amylase levels and to perform abdominal imagingto rule out acute pancreatitis. Similarly, if the etiology of pancreatitis is not found and in the setting of fever and thrombocytopenia, it may be worth while working up for dengue fever even when fever has subsided.
References - World Health Organization Regional Office for South-East Asia.Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever. Revised and expanded edition.World Health Organization: 2011. 196p.
- Samanta J, Sharma V. Dengue and its effects on liver. World J Clin Cases 201516;3:125-31.
- Wijekoon CN, Wijekoon PW. Dengue hemorrhagic fever presenting with acute pancreatitis. Southeast Asian J Trop Med Public Health 2010; 41:864-866.
- Shamim M. Frequency, pattern and management of acute abdomen in dengue fever in Karachi, Pakistan. Asian J Surg 2010; 33:107-113.
- Khor BS, Liu JW, Lee IK, Yang KD. Dengue hemorrhagic feverpatients with acute abdomen: clinical experience of 14 cases. Am J Trop Med Hyg 2006; 74:901-904.
- Simadibrata M. Acute pancreatitis in dengue hemorrhagic fever.Acta Med Indones 2012; 44:57-61.
- Agrawal A, JainNirdesh, Gutch Manish, Shankar Amit. Acute pancreatitis and acute respiratory distress syndrome complicating dengue haemorrhagic fever. BMJ Case Reports 2011;2011;bcr1020114891
- Seetharam P, Rodrigues G. Dengue Fever presenting as acute pancreatitis. Eurasian J Med. 2010;42:151-2.
- Karoli R, Fatima J, Singh G, Maini S. Acute pancreatitis: an unusualcomplication of dengue fever. J Assoc Physicians India 2012;60:64-5.
- Iqbal N, Viswanathan S, Remalayam B, Muthu V, George T. Pancreatitis and MODS Due to Scrub Typhus and Dengue Co-Infection. Trop Med Health. 2012;40:19-21.
- Jain V, Gupta OP, Rao T, and Rao S. Acute Pancreatitis Complicating Severe Dengue. J Glob Infect Dis 2014 ;6: 76–78.
- Kumar KJ, Chandrashekar A, Basavaraja CK, Kumar HC. Acute pancreatitiscomplicating dengue hemorrhagic fever. Rev Soc Bras Med Trop 2016 ;49:656-659.
- Sudulagunta SR, Sodalagunta MB, Sepehrar M, Bangalore Raja SK, NatarajuAS,Kumbhat M, Sathyanarayana D, Gummadi S, Burra HK. Dengue shock syndrome. Oxf Med Case Reports. 2016;2016:omw074.
- Jayasundara B, Perera L, de Silva A. Dengue fever may mislead the surgeonswhen it presents as an acute abdomen. Asian Pac J Trop Med 2017;10:15-19
- Anam AM, Rabbani R, Shumy F, Polash MM. Subsequent pancreatitis andhaemothorax in a patient of expanded dengue syndrome. Trop Doct. 2016;46:40-2.
- Lee CY, Tsai HC, Lee SS, Lin CK, Huang JS, Chen YS. Dengue hemorrhagic feverpresenting with hemorrhagic pancreatitis and an intramural hematoma of theduodenal wall: a case report and review of the literature. Southeast Asian J Trop Med Public Health 2013;44:400-8.
- Jusuf H, Sudjana P, Djumhana A, Abdurachman SA. DHF with complication of acutepancreatitis related hyperglycemia: a case report. Southeast Asian J Trop MedPublic Health. 1998 ;29:367-9.
- Fontal GR, Henao-Martinez AF. Dengue hemorrhagic fever complicated bypancreatitis. Braz J Infect Dis 2011;15:490-2.
- Chen TC, Perng DS, Tsai JJ, Lu PL, Chen TP. Dengue hemorrhagic fever complicated with acute pancreatitis and seizure. J Formos Med Assoc2004;103:865-8.
- Anam AM, Rabbani R, Shumy F. Expanded dengue syndrome: three concomitant uncommon presentations in the same patient. Trop Doct doi:10.1177/0049475517696638.
- Khanna S, Vij JC, Kumar A, Singal D, Tandon R. Etiology of abdominal pain in dengue fever. Dengue Bulletin 2005; 29:85-88.
- Ramos-De La Medina A, Remes-Troche JM, González-Medina MF, Anitúa-ValdovinosMdel M, Cerón T, Zamudio C, Díaz-Vega A. [Abdominal and gastrointestinal symptomsof Dengue fever. Analysis of a cohort of 8559 patients]. Gastroenterol Hepatol2011;34:243-7.
- Setiawan MW, Samsi TK, Wulur H, Sugianto D, Pool TN. Epigastric pain and sonographic assessment of the pancreas in dengue hemorrhagic fever. J Clin Ultrasound 1998; 26:257-259.
- Chatterjee N, Mukhopadhyay M, Ghosh S, Mondol M, Das C, Patar K. Anobservational study of dengue fever in a tertiary care hospital of eastern India.J Assoc Physicians India. 2014;62:224-7.
- Chakravarti A, Suresh K, Neha, Shweta, Malik S. Dengue outbreak in Delhi in2009: study of laboratory and clinical parameters. J Commun Dis. 2012;44:163-8.
- Majumdar R, Jana CK, Ghosh S, Biswas U. Clinical spectrum of dengue fever in atertiary care centre with particular reference to atypical presentation in the2012 outbreak in Kolkata. J Indian Med Assoc. 2012 Dec;110(12):904-6
- Lee IK, Khor BS, Kee KM, Yang KD, Liu JW. Hyperlipasemia/pancreatitis inadults with dengue hemorrhagic fever. Pancreas. 2007;35:381-2.
|