48uep6bbphidcol2|ID
48uep6bbphidvals|1861
48uep6bbph|2000F98CTab_Articles|Fulltext
Amoebic liver abscess is a common cause of febrile illness intropical countries. It usually presents with fever and right upper quadrant abdominal pain. Although rupture of amoebic liver abscess is a common complication seen in about 22% of cases, rupture into stomach is very rare.1 Here, we report a case where a large left lobar liver abscess resolved almost completely due to formation of hepatogastric fistula.
Case Report
A 47 years old male presented with low grade, on and off fever and right upper quadrant abdominal pain for 20 days. On examination he had tender hepatomegaly. Biochemical investigation revealed Hb 10.6 g/dl, total leucocyte count 11000/cumm, alanine aminotransferase 72 IU/L, aspartate aminotransferase 96 IU/L and INR- 1.6. His blood cultures were negative. Serology for Entamoeba histolyticawas found to be positive.
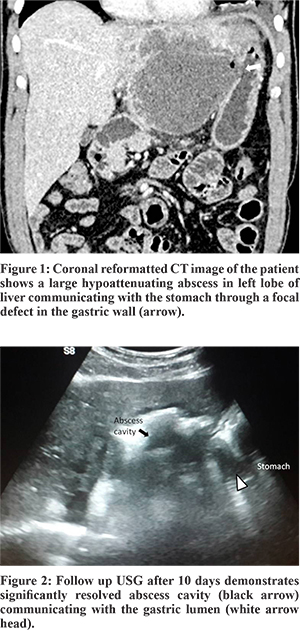
Abdominal USG showed a large, well defined, thick walled abscess of size 11 x 9.6 x 8 cm in the left lobe of liver. Athin rim of hepatic parenchyma was seen at the periphery on the medial aspect. There was no free fluid in the abdomen. USG guided percutaneous drainage of the abscess was plannedafter normalisation of INR. The same night he had an episode of severe epigastric pain. CECT of this patient was done showing an enlarged liver with a large well defined hypoattenuating lesion in the left lobe. There was a communication between the lesion and the adjacent gastric wall in the lesser curvature. Small air pockets were seen within the liver abscess,suggesting fistulous communication with stomach (Figure 1). No ascites was present. Based on imaging and biochemical findings, diagnosis of amoebic liver abscess with hepatogastric fistula was made. Patient was kept under close observation. He was managed conservatively within travenous metronidazole, ceftriaxone and pantoprazole. During this time,his pain improved thoughhe had increased frequency of dark brown coloured loose stool. There was no hematemesis or bilious vomiting. After 10 days, the patient showed clinically significant improvement repeat USG showed a collapsed abscess cavity with a defect communicating with the gastric lumen (Figure 2). The patient was subsequently found to be asymptomatic after 1 month follow up.
Discussion
Amoebic liver abscess is the most common extra-intestinal manifestationof invasive amoebiasis caused by the parasite Entamoebahistolytica with a prevalence of 3-9%. It is more commonly seen in alcoholic males of low socioeconomic status. Although more common in the right lobe, it is also seen in left lobe of liver. The most common complication of amoebic liver abscess is rupture into adjacent structures, associated with high mortality (20-75%).1 Rupture is more common in left lobe abscess.2 Components such as cystinease, amebapore andgalactose-/N-acetylgalactosamine binding lectin within the abscess cavity cause tissue invasionand lead to local complications. Common sites of rupture of the abscess are into the pleura and lungs (72%), subphrenic (4%) and peritoneal cavity (10%).1 Rupture into the stomach is very rare and has been reported in 0.3% in a series of 110 patients with perforated amoebic liver abscess. The site of perforation depends onthe location of the abscess in the liver; upper right lobe abscess usually perforates into the right pleural cavity and right lung; left lobe abscess to the left lung, pericardium, orstomach; whereas abscess in the lower portion of the livercan extend to the peritoneal cavity, gall bladder, colon.1
Involvement of the hepatic duct may result in internal biliary fistula and the patient may present with bilious vomiting. As bile flows through the path of least resistance, biliary system may preferentially drain through the hepatogastric fistula into the stomach instead of the common bile duct (CBD) and ampulla.This high output from the internal biliary fistula prevents its spontaneous closure. In such situations,endoscopic papillotomy and stenting of common bile duct may divert the bile flow and hasten healing of the fistulous tract. ERCP and stenting of the common bile duct has been reported in internal biliary fistula.5 Operative strategies are recommended in hepatogastricfistula with HCC, if fistula fails to heal by conservative management or if there are features of peritonitis.
Insummary, gastric perforation of liver abscess is a very rare complication of amebic liver abscess. Diagnosis is confirmed by CT scan and upper GI endoscopy. While, there are no definite management guidelines in place, the treatment must be individualized accordingto clinical presentation.
References
- Meng XY, Wu JX. Perforated amebic liver abscess: clinical analysis of 110 cases. South Med J. 1994;87:985-90.
- Sharma MP, Acharya SK, Verma N, Dasarathy S. Clinical profile of multipleamoebic liver abscesses. J Assoc Physicians India. 1990;38:837-9.
- Kumar R, Sundar S, Sharma P, Sarin SK. Conservative management of liverabscess complicated by hepatogastric fistula. Dig Liver Dis. 2011;43:752-3.
- Budhiraja S, Dhatt GS, Babra RS. Hepatogastric fistula in a pediatricpatient. Pediatr SurgInt. 2006;22:853-5.
- Sandeep SM, Banait VS, Thakur SK, Bapat MR, RathiPM, Abraham P. Endoscopic biliary drainage in patients with amebicliver abscess and biliary communication. Indian J Gastroenterol. 2006;25:125-127.