48uep6bbphidcol2|ID
48uep6bbphidvals|1795
48uep6bbph|2000F98CTab_Articles|Fulltext
We report a case of isolated pancreatic tuberculosis in an immunocompetent female simulating solid pseudo-papillary epithelial neoplasm (SPEN).
Case Report
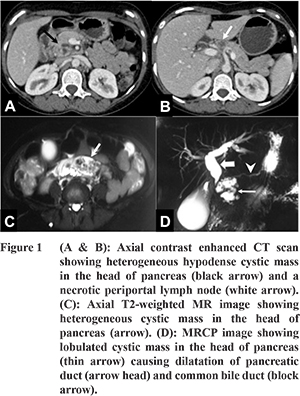
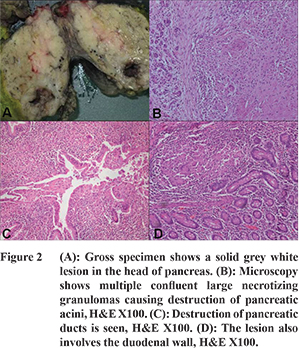
A 23 years old female presented with history of jaundice, high coloured urine, clay coloured stools and severe diffuse pain in the abdomen for few days. She did not give any history of weight/appetite loss or fever. Biochemical investigations were as follows: SGOT-118 IU, SGPT-109 IU, GGT-232 IU, ALP-666 IU, serum bilirubin-7.8, BU-10, serum creatinine-0.6, serum protein-7.8, albumin-4.3, globulin-3.5 and CA19-9-37.3 U/ml. Ultrasound abdomen showed a 2.2x2.2x2.8 cm solid mass in head of pancreas. Contrast enhanced computed tomography (CT) scan showed a heterogeneous cystic lesion in the head of pancreas causing dilatation of common bile duct (CBD) and pancreatic duct (PD) (Figure 1). Few enlarged necrotic periportal and aortocaval nodes were also seen. Magnetic resonance imaging (MRI) with MR cholangiopancreatography (MRCP) done subsequently showed a complex cystic mass with solid component in the head of pancreas, a prominence of main PD, dilatation of CBD and intra-hepatic biliary radicles. Endoscopic ultrasound (EUS) showed a large, solid cystic lesion measuring 5.6x3.4 cm in the head of pancreas. A provisional diagnosis of SPEN was suggested and patient was operated. On intraoperative examination, 2x2 cm mass was seen in the head of pancreas along with multiple lymph nodes in aortocaval and retropancreatic region. Lymph node submitted for frozen section showed caseation necrosis. Since, tuberculosis is prevalent in this part of world and is a common co-existent finding, Whipple’s was performed with a provisional diagnosis of pancreatic SPEN. Gross examination of the specimen showed a solid lesion in the head of pancreas measuring 3x2.5x2 cm along with few enlarged lymph nodes (Figure 2). Sections examined showed large confluent necrotizing granulomas in the pancreas and adjacent duodenal wall. The granulomatous inflammation was seen to affect both the pancreatic acini and ducts. Some of the dissected lymph nodes also showed necrotizing granulomatous inflammation. Special stains performed for acid fast bacilli (Ziehl Neelson and Auramine Rhodamine) did not reveal any bacilli. Based upon the histomorphology, a final diagnosis of tuberculous inflammation was given. Postoperative course of the patient was uneventful. She was started on anti-tubercular therapy.
Discussion
Primary abdominal tuberculosis is not uncommon. Tuberculosis easily disseminates to gastrointestinaltract, liver, spleen and mesenteric lymph nodes; however the involvement of pancreas by tuberculosis is rare, with a worldwide incidence reported to beless than 4.7 percent.
1 Signs and symptoms are variable and include abdominal pain, weight loss, anorexia, fever, vomiting, jaundice and pancreatic mass. Patients may also present with obstructive jaundice and a pancreatic mass lesion that is clinically indistinguishable from a pancreatic neoplasm or pancreatic cyst or an abscess which can be mistaken fora cystic neoplasm or an infected pseudocyst as in our case.
2 Feng Xia et al described several clinical characteristics of pancreatic TB as follows: (1) pancreatic TB is mostly seen in young people, especially female, while pancreatic tumor is more common in old persons; (2) some patients have a history of TB in past, and most often come from areas having high incidence of active tuberculosis; (3) the patients often present with epigastric pain, fever and weight loss; (4) ultrasound and CT scan show pancreatic mass and peripancreatic nodules, some with focal calcification.
1 To conclude, isolated pancreatic tuberculosis presenting as cystic mass is rare and patients generally complain of non-specific symptoms. In areas with high incidence of active infection and clinical or radiological evidence of lymphadenopathy, a high index of suspicion must be kept. Furthermore, preoperative EUS guided FNA/biopsy may be performed both from the main lesion and adjacent lymph nodes to avoid extensive surgery. If still, a pre or intra-operative diagnosis cannot be made, surgical excision may be required. However, this is usually associated with low morbidity and mortality and good longterm outcome after adequate ATT.
References
- Rong YF, Lou WH,Jin DY. Pancreatic tuberculosis with splenic tuberculosis mimicking advanced pancreatic cancer with splenic metastasizes: a case report. Cases Journal. 2008;1:84 doi:10.1186/1757-1626-1-84.
- Chatterjee S, Schmid ML, Anderson K, Oppong KW. Tuberculosis and the Pancreas: A Diagnostic Challenge Solvedby Endoscopic Ultrasound. A Case Series. J Gastrointestin Liver Dis. 2012;21(1):105-7.