48uep6bbphidcol2|ID
48uep6bbphidvals|1776
48uep6bbph|2000F98CTab_Articles|Fulltext
Gastrointestinal tract involvement is uncommonin Sarcoidosis. Pancreatic involvement is even rarer and occurs in 1-3% of cases of systemic Sarcoidosis. There are few case reports of Sarcoidosis presenting as acute pancreatitis. In most of these cases, granulomatous infiltration of pancreas has been implicated as the etiology for pancreatitis. We report an atypical presentation of Sarcoidosiswith hypercalcemia induced pancreatitis presenting for the first time in the Emergency room (ER).
Case Report
A 55 years old male presented with pain abdomen associated with nausea and vomiting for 20 days duration. There was no history of abdominal distension, constipation, fever or jaundice. He was a non-diabetic and non-hypertensive with no history of alcohol or any other addictions. On examination, he was conscious and oriented with stable vital signs. The abdomen was soft with an ill-defined mass palpablein the epigastrium. The neurological, cardiovascular, and chest examination were unremarkable.
His investigations revealed leukocytosis (22,300 cells/mm3), hypercalcemia (corrected Calcium 15 mg/dL: normal 8.4-10.2 mg/dL), an elevated alkaline phosphatase (326 U/L; normal: 32-128 U/L) and increased serum creatinine levels (2.4 mg/dL). The blood sugars were elevated (fasting - 171 mg/dL, Post Prandial - 324 mg/dL) with HbA1c of 7.3%. Serum amylase and lipase were more than 4 times the upper limit of normal (Serum amylase - 264 U/L; lipase - 720 U/L). The coagulation and lipid profiles were normal. Contrast enhanced CT scan of abdomen and chest confirmed acute necrotizing pancreatitis with peripancreatic fluid collections and significant mediastinal lymphadenopathy. (Figure 1,2,3) Further investigations for hypercalcemia showed a normal parathyroid hormone, vitamin D and parathyroid hormone related peptide (PTHrp). Serum and urine electrophoresis alongwith Sestamibi scan was normal. In view of significant mediastinal lymphadenopathy patient underwent endoscopic transbronchial and endobronchial biopsy along with transbronchial needle aspiration (TBNA & TBLB), which showed a nodular erythematous airway mucosa. Biopsy from these lesions showed noncaseating granulomas (Figure 4,5). Staining of biopsy specimen for fungi and acid-fast bacilli was negative. His ACE levels were on the higher side (86 micrograms/L).

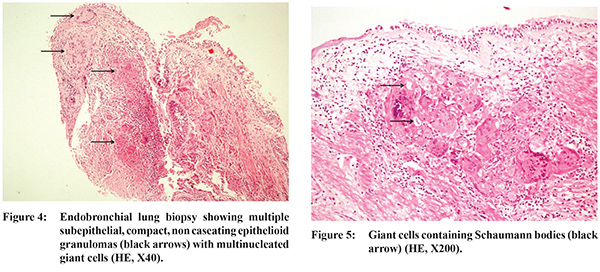
Hence on the basis of clinical presentation, two organs involvement of lymph nodes and lung, characteristic histopathologic findings, elevated ACE levels and exclusion of other granulomatous diseases, a diagnosis of sarcoidosis was made. The patient was managed with intravenous hydration, narcotic analgesics and started on tapering doses of prednisolone. Insulin was administered for recently diagnosed diabetes mellitus.
The patient showed resolution of symptoms with abdominal pain resolving in two weeks time and subsequently abdominal lump also got reduced. However, after three months patient again presented to ER with history of upper gastrointestinal bleed. CT angiography was done which revealed a pseudo aneurysm in the splenic artery (Figure 6). Coil embolization followed by cyanoacrylate glue injection of the pseudo aneurysm was done and hemostasis achieved. The patient has been asymptomatic since then and the steroids have been tapered to 5 mg/day for sarcoidosis.
Discussion
Pancreatic involvement in sarcoidosis, first described in 1937 by Nickerson may be symptomatic or asymptomatic.In the reported literature, the pancreatic involvement in sarcoidosis is seen in 1-3% of patients. Sarcoidosis may presents like a mass lesion localized to the head of pancreas or as a diffusely indurated pancreas. Sarcoidosis presenting as acute pancreatitis is a rare occurrence and its diagnosis is based on a compatible clinical presentation involving at least two organ systems, supportive histologic evidence of noncaseating granulomas, and an exclusion of other granulomatous diseases.
1, 2 Symptomatic pancreatic sarcoidosis most commonly presents as pancreatic mass or acute pancreatitis either due to organ infiltration and compression by enlarged lymph nodes. Cases of acute idiopathic pancreatitis in patients of sarcoidosis have also been described in literature. Hypercalcemia induced pancreatitis has been reported in sarcoidosis patients after sun exposure, but these patients also had other risk factors.
3 Our patient was extensively evaluated for the cause of pancreatitis. Other than hypercalcemia all other work up came out to be negative.
Acute pancreatitis caused by hypercalcemia was first described in 1957 by Cope et al.
4 Most of the cases were described in association with primary hyperparathyroidism. Pancreatitis in cases of hypercalcemia results from either pancreatic duct obstruction due to deposition of calcium in pancreatic duct or activation of trypsinogen within pancreatic parenchyma causing auto digestion of pancreas. Genetic factors e.g. SPINK 1 (serine protease InhibitorKazal type 1) and CFTR (cystic fibrosis transmembrane conductance regulator) gene mutations, have also been implicated.
5 There are no standard guidelines for the treatment of pancreatic sarcoidosis, corticosteroids being the mainstay of therapy. The prognosis of the disease is variable and the recurrence rate of pancreatic sarcoidosis in severe symptomatic cases is almost 100% after discontinuing corticosteroids.
References
- Eguro H, Yabuki M. Sarcoidosis of the skeletal muscle with tumor formation. A case report and review of the literature. Yokohama Med Bull. 1966;17:75-90.
- Johns CJ, Michele TM. The clinical management of sarcoidosis. A 50-year experience at the Johns Hopkins Hospital. Medicine (Baltimore). 1999;78:65-111.
- Cronin CC, Dineen SF, O’Mahoni MS, et al: Precipitation of hypercalcemia in sarcoidosis by foreign sun holidays: report of four cases. Postgrad Med J. 1990;66:307-309.
- Cope O, Culver PJ, Mixter CG, Jr, Nardi GL. Pancreatitis, a diagnostic clue to hyperparathyroidism. Ann Surg. 1957;145(6):857-863.
- Felderbauer P, Karakas E, Fendrich V, Bulut K, Horn T, Lebert R, Holland-Letz T, Schmitz F, Bartsch D, Schmidt WE. Pancreatitis risk in primary hyperparathyroidism: relation to mutations in the SPINK1 trypsin inhibitor (N34S) and the cystic fibrosis gene. Am J Gastroenterol. 2008;103:368-374.