|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Peptic ulcer, perforation, Boey score, prognosis |
|
|
Abhishek Agarwal, Sanchit Jain, LN Meena, Sumita A Jain, Lakshman Agarwal
Department of General Surgery,
SMS Medical College,
Jaipur, India
Corresponding Author:
Dr. Sanchit Jain
Email: drsanchit@rediffmail.com
DOI:
http://dx.doi.org/10.7869/tg.300
Abstract
BACKGROUND: The major complications of peptic ulcer are hemorrhage, perforation and gastric outlet obstruction with perforation occurring in about 2-10% of patients. Patients with perforated peptic ulcer still have a high rate of morbidity and mortality and to improve the outcomes it is important to stratify the patients into different categories.
AIMS: To evaluate the accuracy of Boey scoring system in predicting postoperative morbidity and mortality in patients operated for peptic perforation.
METHODS: It was a prospective observational single centre study conducted at SMS Medical College and Hospital, Jaipur, from October 2011 to October 2012 on 180 patients undergoing open surgery for peptic ulcer perforation. Postoperative outcomes in terms of recovery and complications were studied. For prediction of morbidity and mortality by Boey risk stratification, the odds ratio (OR) and 95% confidence interval (95% CI) of each risk score were compared with the outcomes of ''0'' risk score.
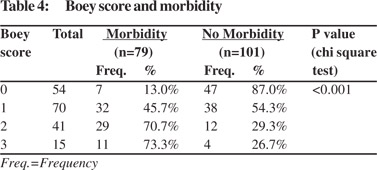
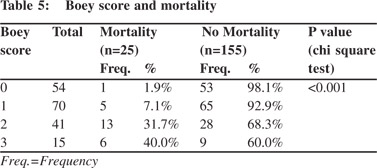
RESULTS: The mortality rate increased progressively with increasing numbers of the Boey score: 1.9%, 7.1%, 31.7% and 40% for 0, 1, 2, and 3 scores, respectively (p<0.001). The morbidity rates for 0, 1, 2, and 3 Boey scores were 13%, 45.7%, 70.7% and 73.3% respectively (p<0.001).
CONCLUSIONS: Boey score is a useful tool for assessing the prognosis of operated cases of peptic perforation and helps in the assessment of mortality and morbidity of these patients.
|
48uep6bbphidvals|1364 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext The estimated prevalence of peptic ulcer disease ranges from 5 to 15% in the western population.[1] The major complications of peptic ulcer are hemorrhage, perforation and gastric outlet obstruction. Perforation occurs in about 2–10% of peptic ulcers.[2] Although the origin of perforated peptic ulcer (PPU) is multifactorial it is most commonly associated with Helicobacter pylori (HP) infection and non steroidal anti-inflammatory drugs (NSAIDs).The incidence of elective surgery for peptic ulcer disease has decreased due to the availability of highly effective medical management, however, the incidence of surgery for perforated peptic ulcer has remained stable or increased over the past two decades.[4] However, patients with PPU still have a high rate of morbidity and mortality, and surgical outcomes vary between hospitals. Mortality rates range from 6 to 14% in recent studies.[5] To improve outcome it is important to stratify the patients into different categories based on the morbidity and mortality, and provide a suitable risk-group-based management. Three prognostic factors, namely preoperative shock, long-standing perforation, and associated medical diseases, were identified in patients with perforated peptic ulcer by Boey et al in 1982[6] and validated in 1987.[7] The Boey scoring system is amongst the most commonly used for risk stratification because of its simplicity and high predictive value for mortality and morbidity in cases of PPU.[8,9] The purpose of this study was to evaluate the surgical outcomes and accuracy of Boey scoring system in predicting postoperative morbidity and mortality in patients operated on for peptic perforation.
Methods
The study was a hospital based prospective observational study conducted at SMS hospital, Jaipur from October2011 to October 2012. The patients included in the study were all the patients operated for perforated peptic ulcer by open surgery irrespective of the age. The patients excluded were perforations associated with malignancy, patients who died before surgery and those in whom procedure other than primary repair with omentoplasty was done.
For diagnosis after a quick general and abdominal examination an X-ray abdomen upright was obtained for the presence of free gas under diaphragm. In the rest of the cases USG abdomen was done to confirm the diagnosis or the patient was posted for emergency laparotomy if there was a strong clinical suspicion.
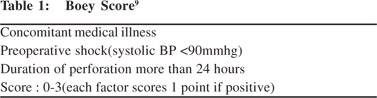
As soon as the diagnosis was made, after resuscitation the patient was posted for surgery. Patients with perforated peptic ulcer were divided into four groups based on the Boey scoring system (score 0–3) (Table 1). The score of each patient was the sum total of three independent risk factors (concomitant severe medical illness, preoperative shock, and duration of PPU longer than 24 hours; a value of 1 was assigned to each factor). Shock was defined as persistent hypotension [systolic blood pressure<90 mmHg]. Duration of the perforation was determined as the time interval between the onset of severe acute abdominal pain, and arrival time at the hospital.
In each and every case of PPU during laparotomy primary closure with omental grafting was performed. A feeding jejunostomy was added in cases of larger perforations based on the surgeon’s decision. Where procedures other than primary closure with omentoplasty were performed, patients were not included in the study. An intra-abdominal drain was usually placed and thorough peritoneal lavage was done using normal saline in all cases.
Postoperatively, intravenous antibiotics were given for 3–5 days. During postoperative period evaluation was done regarding morbidity and mortality. In case of uneventful recovery patients were discharged from the hospital when they had a good appetite and were ambulatory. If a patient had complications they were managed accordingly. All patients were called for follow up 15 days after surgery and after that as per requirement.
All the collected data was compiled and results obtained using SPSS-IBM software version 20. The comparison of normally distributed continuous variables between the groups was performed using the Student’s t test. Nominal categorical data between the groups were compared using the Chi-square test or Fisher’s exact test as appropriate. With regard to the prediction of morbidity and mortality by Boey risk stratification, the odds ratio (OR) and 95% confidence interval (95% CI) of each risk score were compared with the outcomes of ‘‘0’’ risk score, and were also adjusted with age, gender, size and location of PPU. For all statistical tests a p value of < 0.05 was considered statistically significant.
Logistic regression analysis and receiver-operating characteristic (ROC) curve analysis were used to estimate the predictive ability of the Boey score in assessing the postoperative morbidity and mortality. The area under the ROC curve (AUC) indicates the probability of concordance between the predicted probability of postoperative morbidity or mortality and the actual postoperative state. The area ranges from 0.50 for chance performance to 1.00 for perfect prediction.
Results
During the study period 186 patients underwent surgery for perforated peptic ulcer. Five patients were excluded as in them procedures other than primary closure with omentoplasty were performed. One patient was excluded as biopsy from the perforation indicated malignancy. So a total of 180 patients were included in the study.
The mean age was 48 years and maximum patients were seen in the age group 41- 50 yrs with more than half (55.6%) of the patients belonging to 40 – 60 yrs age group. Out of 180, 87.2% (157) were male and 12.8% (23) female. Approximately 30% of patients belonged to the elderly age group (age>60 years). Amongst the various risk factors, 15% patients used to take alcohol regularly, 30.6% were smokers and 19.4% used to take NSAID’s regularly.
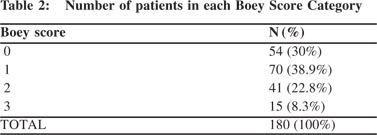
Pneumoperitoneum on plain X-ray was seen in up to 88% of cases. Preoperative shock was seen in 53(29.4%) patients and 118(65.6%) patients presented to the hospital after 24 hours of onset of acute abdominal pain. Associated chronic medical illness was seen in 27(15%) patients. Table 2 shows number of patients in each Boey score category. Maximum number of patients (38.9%) had Boey score 1 and only 8.3% patients had a Boey score of 3.
The most common site of perforation was D1 (first part of duodenum) followed by the prepyloric region and body of stomach. The mean size of perforation was 0.9cm (range 0.25 – 2.5cm) with maximum number of patients having perforation size between 0.5 and 1.5 cm.
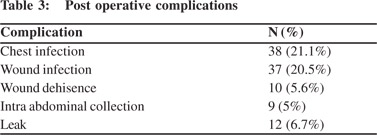
Postoperative complications (Table 3) were seen in 79(43.9%) patients. The most common complications were chest infection and wound infection. It was noted that occurrence of postoperative complications was significantly associated with age > 60 years, delayed presentation in the hospital, preoperative shock and presence of concomitant illness.
The overall post operative mortality rate was 13.9%. Out of the 25 patients who died, 17 died due to septicaemia and subsequent multi-organ failure while 6 patients died following leak and its complications. One patient had acute myocardial infarction and another patient succumbed to respiratory complications in the postoperative period.
It was noted that delayed presentation in the hospital and preoperative shock were significantly associated with mortality in the postoperative period. In contrast to morbidity, mortality was higher in the <60 age year group. Presence of severe medical illness was associated with a higher mortality rate but the association was not statistically significant.
Although mortality and morbidity were higher in males, the relationship was not statistically significant. On evaluating the relationship between site of perforation and morbidity (p=0.36) and morbidity (0.29) the result was statistically insignificant. So site of perforation did not affect the surgical outcome.
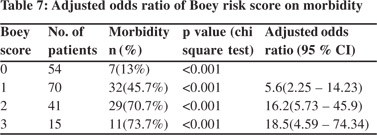
The morbidity rate increased progressively with increasing Boey score: 13%, 45.7%, 70.7% and 73.3% for 0, 1, 2 and 3 scores respectively and the relationship was statistically significant (p<0.001) (Table 4). The mortality rate also increased progressively with increasing numbers of Boey score: 1.9%, 7.1%, 31.7%, and 40% for 0, 1, 2, and 3 scores, respectively and this relationship was again statistically significant (p<0.001) (Table 5).
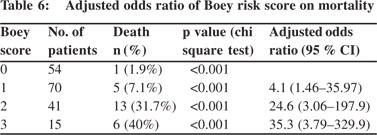
The odds ratio progressively increased with increasing Boey score showing that likelihood of postoperative death (Table 6) and postoperative complications (Table 7) increase with increasing Boey score in cases of perforated peptic ulcer. Receiver–operating characteristic (ROC) curve analysis demonstrated high predictive value of Boey score in predicting postoperative mortality (Figure 1) and morbidity (Figure 2) in our study. The area under the curve (AUC) in ROC curve analysis was 0.793 and 0.753 for mortality and morbidity, respectively. So although the Boey score was a good predictor of mortality and morbidity, its predictive ability was higher for mortality.


Discussion
Perforation occurs in 2-10% of patients with PUD and accounts for more than 70% of deaths associated with PUD. Often perforation is the first clinical presentation of PUD.[10] The incidence of duodenal perforation is 7-10 cases/ 100.000 adults per year. The perforation site usually involves the anterior wall of the duodenum (60%), although it may involve the antrum (20%) and lesser-curvature (20%).[11] In our study also the most common site of perforated peptic ulcer was the first part of the duodenum followed by prepyloric region and body of stomach. This observation was similar to that of other investigators.[12,13]
The peptic ulcer perforation was more common in males in our study. A similar finding has been noticed by other investigators.[5,7,12] A possible explanation for these findings may be that some behaviours such as smoking and drinking alcoholic beverages, are more frequent among men, thus increasing the risk of peptic ulcer diseases and perforation. In the present study, the morbidity rate was 43.9%. Overall, the postoperative complication rate in the literature ranges from 17% to 63%.[14,15] Pulmonary complications and wound infection were the leading postoperative complications as reported in other studies.These findings could be explained by the fact that emergency upper abdominal surgery carries a significant risk of pulmonary complications[16], and surgery for PPU is regarded as a contaminated or dirty operation, which has a wound infection rate of 15–40%.[17,18]
In all cases of wound dehiscence secondary suturing was done. Chest infection was seen in 38 patients and most of them were managed conservatively. Two of these patients developed bilateral pleural effusion which required USG guided aspiration in one case and tube drainage in the other. One patient died of respiratory complication. Intra-abdominal collection was seen on USG in nine patients. One of these patients had to be treated surgically whilst the others were managed conservatively. Leakage in the post-operative period was seen in 12 patients, seven of them were managed conservatively while 5 had to be operated on. Overall mortality was 13.9%, but it climbed fourfold to 38% in patients with all three Boey risk factors. Overall mortality after surgery for PPU in recent studies varies from 6% to 14% and remains at approximately 30–60% in patients with a Boey score of 2 or more.[5,8,12]
The initial study by Boey et al showed that patients with risk factors 0, 1, 2 and all 3 have mortality rates of 0%, 10%, 45.5% and 100%, respectively.[7] Progress and development in critical care over the years has helped to reduce mortality rates dramatically. Most of our patients were referred from peripheral hospitals at great distances which delayed the treatment thus increasing both morbidity and mortality.
Over the years many prognostic systems have been introduced to predict outcomes in severely ill patients. This includes scoring indices such as the Acute Physiology and Chronic Health Evaluation (APACHE) score, the Simplified Acute Physiology Score (SAPS),the Jabalpur Index, the Multi Organ Failure (MOF) Score, and the Mannheim Peritonitis Index (MPI). Many have not proven useful on a large scale as either some of them are applicable only in certain conditions or some take into consideration so many factors that calculating scores becomes too complex. Our study has reaffirmed the accuracy of the Boey scoring system in predicting postoperative complications and death in peptic perforation patients. The odds ratio of developing mortality and morbidity increased progressively with increasing numbers of the Boey score. Early and accurate identification of patients with increased risk of adverse outcomes is needed to plan monitoring and treatment. Thus, a clinical scoring system should be able to predict adverse outcome with a high degree of precision and the score should be easy to calculate. Boey score as described is specific for PPU and being based on only three factors is easy to calculate.
In conclusion, while no scoring system is ideal and each has its limitations, Boey score is one of the scores that is easily applicable in clinical practice in patients of peptic perforation peritonitis.
References
- Aro P, Storskrubb T, Ronkainen J, Bolling-Sternevald E, Engstrand L, Vieth M, et al. Peptic ulcer disease in a general adult population: the Kalixanda study: a random population-based study. Am J Epidemiol. 2006;163:1025–34.
- Behrman SW. Management of complicated peptic ulcer disease. Arch Surg. 2005;140:201–8.
- Ng EK, Chung SC, Sung JJ, Lam YH, Lee DW, Lau JY, et al. High prevalence of Helicobacter pylori infection in duodenal ulcer perforations not caused by non-steroidal anti-inflammatory drugs. Br J Surg. 1996;83:1779–81.
- Rajesh V, Chandra SS, Smile SR. Risk factors predicting operative mortality in perforated peptic ulcer disease. Trop Gastroenterol. 2003;24:148–50.
- Kocer B, Surmeli S, Solak C, Unal B, Bozkurt B, Yildirim O, et al. Factors affecting mortality and morbidity in patients with peptic ulcer perforation. J Gastroenterol Hepatol. 2007;22:565–70.
- Boey J, Wong J, Ong GB. A prospective study of operative risk factors in perforated duodenal ulcers. Ann Surg. 1982;195:265–9.
- Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers: a prospective validation of predictive factors. Ann Surg. 1987;205:22–6.
- Arici C, Mesci A, Dincer D, Dinckan A, Colak T. Analysis of risk factors predicting (affecting) mortality and morbidity of peptic ulcer perforations. Int Surg. 2007;92:147–54.
- Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D. Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World J Surg. 2009;33:80–5.
- Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician. 2007;76:1005–12.
- Zittel TT, Jehle EC, Becker HD. Surgical management of peptic ulcer disease today indication, technique and outcome. Langenbecks Arch Surg. 2000;385:84–96.
- Lee FY, Leung KL, Lai BS, Ng SS, Dexter S, Lau WY. Predicting mortality and morbidity of patients operated on for perforated peptic ulcers. Arch Surg. 2001;136:90–4.
- Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK. Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg. 2004;91:481–4.
- So JBY, Yam A, Cheah WK, Kum CK, Goh PMY. Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg. 2000;87:1702–7.
- Lunevicius R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg. 2005;92:1195–207.
- Serejo LG, da Silva-Junior FP, Bastos JP, Bruin GS, Mota RM, Bruin PF. Risk factors for pulmonary complications after emergency abdominal surgery. Respir Med. 2007;101:808–13.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol.1999;20:250–78.
- Arias CA, Quintero G, Vanegas BE, Rico CL, Patino JF. Surveillance of surgical site infections: decade of experience at a Colombian tertiary care center. World J Surg. 2003;27:529–33.
|
|
|
 |
|
|