Mukesh Jain, Gyan Prakash Rai, Rupesh Kumar Pokharna, Subhash Nepalia, Prachis Ashdhir
Department of Gastroenterology,
Sawai Man Singh Medical college,
Jaipur - 302004,
Rajasthan, India
Corresponding Author:
Prof. Rupesh Kumar Pokharna,
Email: rkpokharna2@rediffmail.com
DOI:
http://dx.doi.org/10.7869/tg.312
48uep6bbphidvals|1376 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext The ampulla of Vater is located in the posteromedial wall of the second portion of the duodenum.
The common bile duct (CBD) normally goes through an oblique, 1-2 cm long intramural region beside the medial wall of the second portion of the duodenum and opens into the duodenum.[1-3]
At times, the Ampulla of Vater may be ectopic and located in uncommon sites such as the third and fourth portions of the duodenum, the duodenal bulb and the stomach. It has hardly ever been found at the pylorus and in the antrum.[3-5] This ectopic ampulla goes undetected unless it causes symptoms, usually related to biliary obstruction or cholangitis or when, for some reason, endoscopic retrograde cholangiopacreatography (ERCP) is attempted. Here we describe a case of colonic tuberculosis with incidentally detected ectopic Ampulla of Vater in the antrum.
Case report
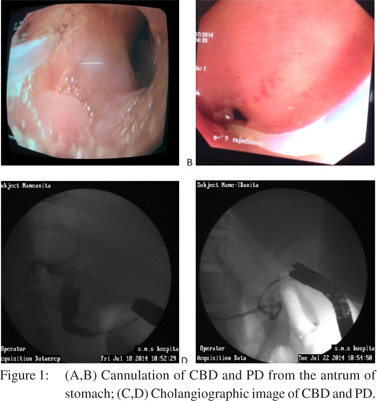
A 23-year-old female presented with complaints of periumbilical colicky pain abdomen with abdominal distension for 1 month prior to admission. The patient also had low grade fever and weight loss. Anemia was present and her physical examination and abdominal examination were normal. Her laboratory data were as follows: hemoglobin-10.8g%, leukocyte count-9.23/mm3, erythrocyte sedimentation rate-38mm/1st hour. Liver function test, renal function test, C-reactive protein, chestxray and ultrasound abdomen were normal. UGIE showed ulcerated area (1.5cm) in the antrum near the pylorus, from which bile seemed to be coming out. Biopsy of this ulcerated area revealed chronic inflammation, and no evidence of malignancy or tuberculosis. CT abdomen suggested bowel wall thickening (18mm) in ascending and transverse colon. Multiple enlarged mesenteric lymph nodes and pneumobilia were also seen. Colonoscopy revealed multiple irregular ulcerations with heaped-up margins and with nodularity at hepatic flexure and ascending colon. Biopsy was suggestive of tuberculosis. In view of pneumobilia and bile seeminglyarising from the ulcerated area in the antrum, possibilities of choledocho-antral fistula or ectopic opening of Ampulla of Vater were considered. Side view endoscopy (SVE) was performed, which did not reveal papilla in normal position or beyond in the duodenum. With SVE, cannulation of CBD and PD was done from two different openings in ulcerated area in the antrum (Figures 1A and B), which revealed contrast in CBD and PD (Figures 1C and D).Both ducts were normal. The patient discharged on antitubercular drugs and kept on follow up.
Discussion
Ectopic location of ampulla in the stomach or first, third, or fourth parts of the duodenum is a very rare congenital anomaly. The reported incidence of anomalous termination of bile duct is 5.6–23%.[2] However ectopic papillae are much less frequent in a proximal location, and a few cases have been located in the gastric, pylorus and duodenal bulb areas.[6] Filippini in 1931 described the first case of papilla located in the pylorus.[7] Thereafter few cases of ectopic Ampulla of Vater in the stomach were reported. The first major case series by Disibeyaz et al in 2007 reported 53 cases of anomalous opening of the CBD in to the duodenal bulb in 1215[8] patients who underwent ERCP procedures. In this study no case was reported with anomalous biliary opening in the stomach.[2] Another major case series by Saritas et al in 2010, reported the frequency of ectopic biliary drainage (EBD) of 2% (10 of 400 ERCP). The sites of EBD in this study were the stomach in 1 case, duodenum bulb in 7 cases and the postbulbar duodenum in 2 cases.[4] All patients were symptomatic due to ectopic biliary opening in these major series. In our case it was an incidental finding.
The exact etiology of this congenital anomaly remains unclear and is believed to be an abnormality during the embryonic developmental period. It has been proposed that an earlier subdivision of the hepatic diverticulum during embryogenesis mightcause the common bile duct to empty into ectopic locations.[3] Ectopic papillae located in the bulb may be secondary to an ulcerous duodenal pathology, which could cause, due to contiguity, anomalous drainage in the duodenum.[1] In our case the diagnosis was made as per criteria for an ectopic papilla as described by Lee et al,[6] - (1) an orifice was observed in the antrum by UGIE, and the bile duct and/or the pancreatic duct were directly visualized radiographically, when contrast was injected (2) direct drainage of the CBD into the antrum without any other drainage into the duodenum oncholangiography and (3) no evidence of a papilla-like structure in the second or third duodenal portions on SVE. In our patient EBD was not related to colonic pathology.
Based on few published reports, there appears to be an increased risk for choledocholithiasis due to anomalous bile drainage and lack of sphincter control mechanisms. Pancreatobiliary secretions can lead to mucosal damage with ulcer formation. The anomalous location in the pylorus can facilitate reflux of gastric contents into the biliary tree, predisposing to biliary tree injury and cholangitis.[2,3] Endoscopists who perform ERCP should be aware of this rare anomaly. In cases where the ampulla cannot be seen in the normal anatomical location, an ectopic ampulla should be suspected, and the endoscopist must carefully examine the stomach and the duodenum. Sphincterotomy should be avoided due to increased risk of perforation. Ampullary balloon dilation is recommended to extract large bile duct stones.[1,2,4]
References
- Sung HY, Kim JI, Park YB, Cheung DY, Cho SH, Park SH,et al. The papilla of Vater just below the pylorus presenting as recurrent duodenal ulcer bleeding. Intern Med. 2007;46:1853–6.
- Disibeyaz S, Parlak E, Cicek B, Cengiz C, Kuran SO, Oguz D,et al. Anomalous opening of the common bile duct into the duodenal bulb: endoscopic treatment. BMC Gastroenterol. 2007;7:26.
- Guerra I, Rábago LR, Bermejo F, Quintanilla E, García-Garzón S. Ectopic papilla of Vater in the pylorus. World J Gastroenterol. 2009;15:5221–3.
- Saritas U, Senol A, Ustundag Y. The clinical presentations of ectopic biliary drainage into duodenal bulbus and stomach with a thorough review of the current literature. BMC Gastroenterol. 2010;10:2.
- Bernard P, Le Borgne J, Dupas B, Kohnen-Shari N, Raoult S, Hamel A. Double common bile duct with ectopic drainage into the stomach. Case report and review of the literature. Surg Radiol Anat. 2001;23:269–72.
- Lee SS, Kim MH, Lee SK, Kim KP, Kim HJ, Bae JS, et al. Ectopic opening of the common bile duct in the duodenal bulb: clinical implications. Gastrointest Endosc. 2003;57:679–82.
|