Anjan Kumar Dhua, Veereshwar Bhatnagar, Devasenathipathy Kandasamy1, Aparajita Mitra, Abhishek Ranjan, Abhimanyu Varshney
Department of Pediatric Surgery and Radiodiagnosis1,
All India Institute of Medical sciences,
New Delhi, India
Corresponding Author:
Dr. Anjan Kumar Dhua
Email: dhuaanjan@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.311
48uep6bbphidvals|1375 48uep6bbphidcol2|ID 48uep6bbph|2000F98CTab_Articles|Fulltext Dilatation of the biliary tree to variable extent and severity is called choledochal cyst (CDC). The prevalence is higher in Asian countries, especially Japan, and females are more affected than males in a ratio of 4:1[1,2]. Eighty percent of CDC patients manifest clinically in childhood and are either detected on an antenatal scan or present later with jaundice and/or abdominal pain. The triad of pain, lump and jaundice is rare in children. Giant choledochal cysts (GCDC), defined as >10 cm in diameter, are uncommonly encountered in practice. The reports of GCDC that are described in the literature pertain to older children and adults. This report highlights that a GCDC can present even in infancy and without features of cholestasis.
Case report
A 5-month-old boy presented with failure to thrive and progressive abdominal distension since one month of age. There was no associated history of jaundice, fever or bowel complaints. The child looked emaciated and weighed 5.5 kg (< 10th percentile for age). He was anicteric and mild pallor was noted. Abdominal examination revealed fullness on the right side. A soft, large, non-tender lump was palpable in the the right hypochondrium, extending to the right iliac fossa and umbilical region. The lump had a smooth surface and was continuous with liver dullness. Laboratory values were: Hb- 10.9 g/dL, total bilirubin-0.7 mg/dL, SGPT-38 IU/L, SGOT-39 IU/L and serum alkaline phospatase-1038 IU/L.
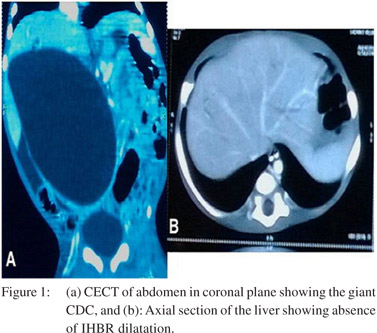
Ultrasound scan of the abdomen and contrast enhanced computed tomography scan revealed a 13 cm ×8.8 cm welldefined round to oval cystic structure occupying almost the entire abdominal cavity with thin peripheral enhancement and continuous with the right and left hepatic ducts. There was no appreciable intra hepatic biliary radical (IHBR) dilatation (Figures 1a & b).
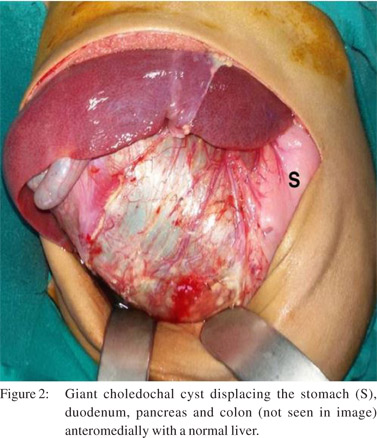
The child underwent laparotomy and a GCDC was seen occupying the entire right side of the abdomen, reaching up to the pelvis with the ascending colon, duodenum and pancreas lifted antero-medially. The liver was grossly normal (Figure 2). After decompressing the contents (650 mL of greenish biletinged fluid) the cyst was completely excised. The common hepatic duct, proximal to the GCDC, was approximately 15 mm in diameter and the lower end of the cyst tapered before joining the pancreatic duct. After flushing the proximal ducts a standard Roux-en-Y hepatico-jejunostomy was performed. The postoperative recovery was uneventful. On follow-up the child is well and thriving.
Discussion
Very few reports of GCDC in infancy were found in the literature with the majority pertaining to adults.[3] Tang et al in a series of 62 children with CDC described a child with jaundice and a cyst measuring 158 mm in the largest dimension, the age of the child was not mentioned though. A massive CDC presenting as an acute abdomen in a 5-month female infant was reported by Okoromah et al.[4] It was initially mistaken as a pseudocyst of pancreas but later confirmed to be CDC by histopathological examination. A recent report by Yurttutan et al[5] describes a 4-month old female infant with abdominal distension and cholestatic jaundice caused by a GCDC. The GCDC had a maximum diameter of 160 mm. The author believes that this is the largest GCDC reported so far in the literature. These scattered reports endorse the fact that this is a rare entity in children, more so in infancy.
The case reported here is unique since the child had neither jaundice nor any other features of cholestasis. This finding is consistent with the observation that a large choledochal cyst has low intra-cystic pressure and produces less cholestatic effects on the liver.[6] This is probably also the reason for a grossly preserved liver with no IHBR dilatation in our case.
References
- Miyano T, Yamataka A, Li L. Congenital biliary dilatation. Semin Pediatr Surg. 2000;9:187–95.
- Komi N, Tamura T, Miyoshi Y, Kunitomo K, Udaka H, Takehara H. Nationwide survey of cases of choledochal cyst. Analysis of coexistent anomalies, complications and surgical treatment in 645 cases. Surg Gastroenterol. 1984;3:69–73.
- Anand U, Priyadarshi RN, Kumar B, Khandelwal C. Diagnosis and management of giant choledochal cysts: complexities compared to smaller cysts. Indian J Gastroenterol. 2013;32:262–7.
- Okoromah CN, Odelola MA, Etukudo FS.Complicated massive choledochal cyst: A case report. Nigerian Journal of Clinical Practice. 2002:5;150–2.
- Yurttutan N, Karakus SC, Koku N, Demirci M, Ucak R. A giantcholedochalcyst in infancy; a casereport. Korean J Pediatr; 2014 August 15.
- Sharma N, Bhatnagar V, Srinivas M, Agarwala S, Singh MK, Sharma R. Correlation of intracystic pressure with cyst volume, length of common channel, biochemical changes in bile and histopathological changes in liver in choledochal cyst. J Indian Assoc Pediatr Surg. 2014;19:10–6.
|