|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Prasenjit Das1, Maneesh K Vijay1, Rajni Yadav1, Sunil Kumar2, Jyoti Sharma2, Siddhartha Datta Gupta1
Department of Pathology1
and Surgical Oncology2,
All India Institute of Medical Sciences,
New Delhi, India
Corresponding Author:
Dr Prasenjit Das
Email: prasenaiims@gmail.com
dr_prasenpgi@yahoo.co.in
DOI:
http://dx.doi.org/10.7869/tg.273
48uep6bbphidvals|733 48uep6bbph|2000F98CTab_Articles|Fulltext Giant villous adenoma (GVA) is a rare mass forming lesion of the gastrointestinal tract, which is often difficult to differentiate from an infiltrating adenocarcinoma based on clinical presentation and radiological investigations. These lesions however can be suspected in an elderly patient if a gastroenterologist is aware of its typical location and presentation, with knowledge that conventional radiological investigations may not give sufficient information regarding its benign nature. If diagnosed peroperatively endoscopic or laparoscopic limited excision procedures can reduce morbidity of extensive surgical resection. Herein, we report a case of a GVA with literature review, citing examples, where they were mistaken for an invasive carcinoma.
Case report
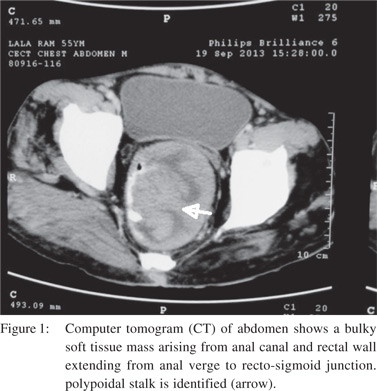
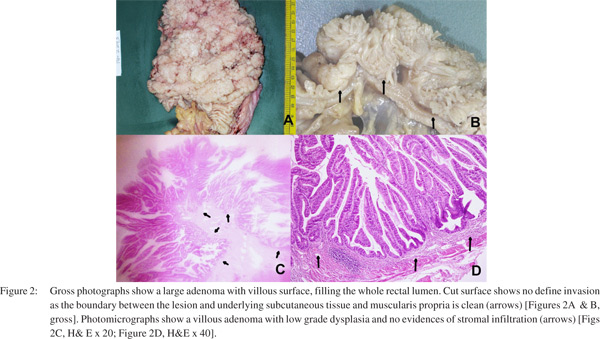
This 55 year old male, presented with history of passing blood and mucus in stool along with weakness since last one year. There was no history of pain during defecation or alteration of bowel habits. No significant family or past history of such illness was there. On clinical examination his performance status was ECOG 2 with pallor and anasarca. Digital rectal examination revealed an ulcero-proliferative growth starting at 1 cm from the anal verge on left lateral wall of rectum and becoming circumferential at 4 cm, with no palpability proximal to it. Growth was mobile and gloved finger was stained with blood. Rest of the systemic examination was unremarkable. Laboratory investigations showed significant anaemia (Hemoglobin 5.2 gm/dL) and hypo-albuminaemia (Albumin 1.2 gm/dL) with rest of the parameters within normal limits, including electrolyte levels. Colonoscopy revealed a circumferential polypoidal growth starting at 1 cm from anal verge and extending up to 10 cm proximally. Computed tomography scan (CT) of abdomen showed a bulky soft tissue mass with ulceration, arising from anal canal and rectal wall extending from anal verge to rectosigmoid junction [Figure 1] with normal liver and no ascites.The lesion was biopsied twice and in both occasions superficial fragments from a villous adenoma (VA) with low grade dysplasia were reported. However as clinical and radiological suspicion of an adenocarcinoma was strong an abdominoperineal resection (APR) was performed. Grossly a 14 centimetres (cm) long APR specimen was received and there was a large villiform lesion measuring 8.5x6x4 cms, lying 5cm away from the proximal resection margin [Figure 2A & B]. The cut surface showed a polypoidal lesion comprising predominantly of villous structures. Grossly infiltration into underlying layers was not identified. Multiple sections examined from all over the lesion showed a villous adenoma with low grade dysplasia. No infiltration into muscularis mucosae or stalk was noted. No displaced glands were identified. No lymph node was found in the APR specimen [Figure 2]. Based on overall features diagnosis of a giant villous adenoma with low
grade dysplasia was suggested. The patient is under regular follow up and is now asymptomatic.
Discussion
Though, it has been stressed in the published literature that, while the proximal colonic adenomas are polypoidal, and the distal ones are sessile, this is not always true. While most of the right colonic lesions present with features of anaemia, the left colonic lesions show altered bowel habit, blood in stool and intestinal obstruction. Amongst the adenomas, VA is least common (5-10%) than the tubular (70%) and tubulo-villous adenomas (10%). Though the VAs are Commonly 2-4 cms in size, rarely they can be more than 5 cm in size and even can be upto 18 cms in size [GVA].[1-3] Giant polyposis causing intestinal symptoms have also been described in inflammatory bowel diseases (IBD), especially in ulcerative colitis.[4] The GVAs are usually seen in the fifth decade and present with features of secretory diarrhoea and electrolyte loss.[1,2] Rarely rectal bleeding can be seen when it is large and ulcerated.[2] Rare reports of GVA presenting as McKittrick–Wheelock syndrome are there, characterized by large volume diarrhoea, sever electrolyte dysfunction and pre-renal acute renal failure.[3] Occasionally irreducible rectal prolapse can be a complication of GVA. The index case presented with diarrhoea admixed with mucus and blood and there was radiological suspicion of an infiltrating carcinoma. No clinical, colonoscopic and radiological feature of IBD was there. Radiological investigations often cannot differentiate a GVA from carcinoma and conventional computer tomography (CT) is non-specific in this regard. Attenuation of conventional CT is equal to the adjacent soft tissue, and hence determination of invasion is difficult. Magnetic resonance imaging (MRI) and CT colonography are considered superior to CT scan.[2]
secretagouges, especially the prostaglandin E2 (PGE2) is thought to induce the goblet cells in VAs leading to excess mucus secretion. As these lesions are mostly situated distally, presence of very less absorptive mucosa beyond the lesion may result in diarrhoea and loss or sodium and potassium.[5] Unless there is infiltration of rectal wall resulting in edema and rigidity, intestinal obstruction is not usual presentation in GVA.[2] As any adenomas of GI tract have malignant potential, they should be removed endoscopically. However GVA is difficult to remove endoscopically and require segmental excision by parasacral approach or anterior mucosal eversion techniques. Trans-anal endoscopic microsurgery is effective in some cases, but may lead to stenotic lesion if the GVA is circumferential, like the index case.[5]
References
- Yaðmurdur MC, Alevli F, Gür G, Haberal N, Moray G, Boyacioðlu S, et al. Giant villous adenoma case mimicking right colon carcinoma. Turk J Gastroenterol 2004;15:270–73.
- Cubuk R, Tasali N, Arslan G, Midi A, Manukyan MN, Guney S.A Giant Villous Adenoma: Case Mimicking Rectosigmoid Malignancy; Radiological Survey to Diagnosis. Prague Medical Report 2010;1:76–81.
- Miles LF, Wakeman CJ, Farmer KC. Giant villous adenoma presenting as McKittrick–Wheelock syndrome and pseudoobstruction. MJA 2010;192:225–7.
- Shah PR, Joseph A, Haray PN, Kiberu S. Giant villous adenoma in an incarcerated rectal prolapse: A clinical conundrum! Indian J Surg 2005;67:100–1.
- Roriz-Silva R, Andrade AA, Ivankovics IG. Giant rectal villous adenoma: Surgical approach with rectal eversionand perianal coloanal anastomosis. Int J Surg Case Reports 2014;5:97– 99.
|
|
|
 |
|
|