|
|
|
|
 |
 |
| |
 |
|
|
Short Reports |
|
|
|
|
|
Keywords :
Tropics, helminthic infection, ascariasis |
|
|
Shivaram Prasad Singh*, Debasis Misra*, Mihir Kumar Mohapatra**, Omprakash Agrawal***, Chudamani Meher***
Department of Gastroenterology*,
and Department of Surgical
Gastroenterology**,
SCB Medical College, Department
of Radiology***,
Beam Diagnostics Centre,
Bajrakabati Road, Cuttack, Orissa,
India
Corresponding Author:
Dr. Shivaram Prasad Singh,
Email:scb_gastro_dept@hotmail.com
DOI:
http://dx.doi.org/10.7869/tg.254
Abstract
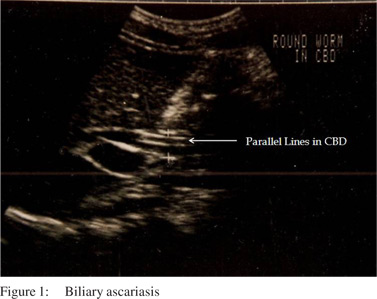
Introduction: Ultrasonographic demonstration of intrabiliary parallel lines or “inner tube sign” is considered diagnostic for biliary ascariasis in regions where ascariasis is endemic. Patients & methods: 148 patients with inner tube sign on ultrasonography were evaluated. In most, diagnosis was confirmed by ultrasonographic demonstration of restitution of normal appearance of bile duct with passage of round worms in vomitus or faeces.
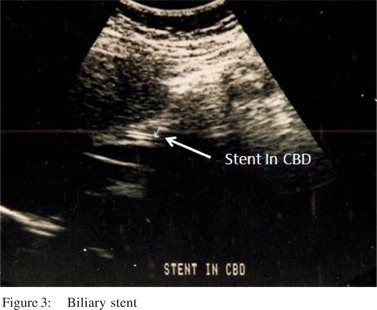
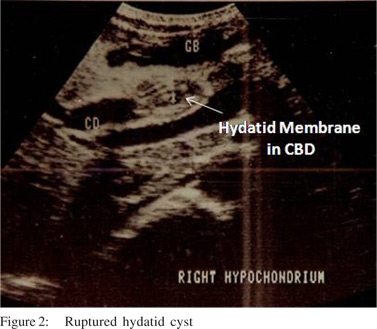
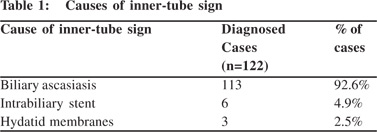
Results: Diagnosis was confirmed in 122 of 148 patients. 26 patients were lost to follow-up. Biliary ascariasis was responsible for the sign “parallel lines” in 113 patients. Of the remaining, intrabiliary stents were responsible for the “inner tube sign” in six whereas in three it was due to hydatid membranes following intrabiliary rupture of hydatid cyst.
Conclusion: Biliary ascariasis is the commonest cause of inner tube sign in the tropics. However, this sign can also be produced by biliary stents and hydatid membranes. Awareness of these possibilities is essential for sonologists in the tropics.
|
48uep6bbphidvals|713 48uep6bbph|2000F98CTab_Articles|Fulltext Ascariasis is the commonest helminthic infestation affecting the population around the world and more so in the tropics and in the low socioeconomic population.[1-3] Demonstration of intrabiliary parallel lines or inner tube sign is considered diagnostic for biliary ascariasis in the regions where ascariasis is endemic.[4-8] A similar picture of “inner tube” can also be present in patients with hydatid cysts of liver with biliary involvement following rupture of the cyst.[9] Another frequently encountered cause of intrabiliary parallel lines today is endoscopically placed biliary stents. Standard text books of radiology donot cover this subject adequately. The aim of this presentation is to highlight the differential diagnosis of “inner tube sign” in the bile duct observed during ultrasonography.
Short Reports
Patients and methods
148 consecutive patients in whom ultrasonography demonstrated the “inner tube sign” during the period from June 1991 to June 1997 comprised the study population. The study group consisted of 98 male (66.2%) and 50 female (33.8%) patients. Children under 12 years constituted 40% of the total patient population. Ultrasonography was performed by a grey scale real-time scanner in a private clinic in coastal Orissa where biliary ascariasis is not uncommon. Real time ultrasonography of the liver, the biliary tree and the pancreas was performed using a convex 3.5 mHz transducer. The “inner tube sign” consists of the demonstration of two distinct echogenic parallel lines inside the biliary tree during realtime ultrasonography. The patients were evaluated clinically and by employing relevant investigations to come to a diagnosis. These patients were subsequently followed up with the help of sonography to determine the course and outcome of the disease. Very few patients needed surgery for relief or cure of their disease. In the majority, diagnosis of biliary ascariasis was confirmed by ultrasonographic demonstration of normal appearance combined with passage of roundworm in vomitus/feces.
Diagnosis of hydatid disease was confirmed by surgery in all the patients with this disease. Diagnosis of hepatic abscesses was confirmed by ultrasonography coupled with sonographyguided needle aspiration from the abscess and examination of the aspirate.
Results
In 148 patients, ultrasonography demonstrated “inner tube sign”. Diagnosis was confirmed in only 122 of these patients It was not possible in the remaining 26 patients who were lost to follow up. Biliary ascariasis was presumed responsible for the ‘sign’ in 113 patients out of the 122 patients on the basis of clinical assessment and ultrasonography. Only nine of these patients with biliary ascariasis underwent surgery for clearance of the biliary tree or associated abnormalities. Of these, five patients had associated hepatic abscess. Of the remaining nine patients, in 6 patients, endoscopically placed intrabiliary stents were responsible for the “inner tube sign”. In the other three, the appearance of the “inner tube sign” was due to hydatid membranes impacted in the common bile duct following intrabiliary rupture of the hydatid cysts in the liver. All the three patients who had associated hydatid cysts in the liver underwent surgery and the diagnosis of hydatid disease was confirmed during surgery.
Discussion
Ascariasis has a global distribution, with more than 1 billion people infected worldwide.[9-11] Biliary ascariasis is predominantly a disease of adult women.[5] Usually, the worms after infesting human beings reside in the upper jejunum. Sometimes, particularly if the worm load is high, the worms can migrate into the biliary channels and rarely into the pancreatic duct. Five distinct clinical presentations of hepatopancreatic ascariasis (HPA) have been reported including biliary colic, a calculou scholecystitis, acute cholangitis, acute pancreatitis, and hepatic abscess.[2,3,9,12-15] Ultrasonography (US) is the preferred imaging method in the diagnosis and post-treatment follow- up of hepatobiliary ascariasis. One of the first reports of biliary ascariasis demonstrated by US was described way back in 1982.[4,16] Various appearances of round worms in the biliary tract and gall bladder have been described. They are:
1. Inner tube sign – The round worm may be seen as a thick echogenic stripe with a central anechoic tube (gastrointestinal tract of the worms) in the gall bladder or common bile duct.
2. Stripe sign – Thin nonshadowing stripe without an inner tube within the gall bladder or common bile duct.
3. Spaghetti sign – Overlapping longitudinal interfaces in the main bile duct due to coiling of a single worm or several worms in the common bile duct.
Characteristic movement is occasionally observed.
Associated findings of HPA include biliary or pancreatic duct dilatation, pancreatic enlargement or gallbladder wall thickening, air in the biliary or pancreatic ducts, and intrahepatic abscess.[5,17] It has been noted that the ascaris parasite can sometimes be observed as a soft tissue mass in dilated biliary tracts, in which case it has to be differentiated from bile sludge, non-opaque bile stone and cholangiocarcinoma.[18] Biliary ascariasis is the commonest cause of “inner tube sign” in the tropics where round worm is endemic. However, this sign can also be produced by biliary stents introduced during endoscopy. This ultrasonologist and consulting physician should keep this in mind as such cases are going to increase with the increasing tribe of intervention endoscopists. Another albeit uncommon cause of the “inner tube sign” is the impaction of the common bile duct by hydatid membranes following intrabiliary rupture of hydatid cysts. Presence of a typical hydatid cyst in the liver helps in settling the diagnosis. However, the appearance of the hepatic lesion on ultrasonography may sometimes be ambiguous and can create problems making it difficult to decide whether we are dealing with a liver abscess or an infected biliary occlusion by hydatid membranes. Another differential diagnosis for pancreatic ductal dilatation with intraductal filling defects would include intraductal papillary-mucinous neoplasm because occasionally mucinous threads can appear linear.
In conclusion, in tropical regions, the ‘inner tube sign’ can result from biliary ascariasis, hydatid membranes and biliary stents. The sentence would then become: " An awareness of these conditions is essential for the ultrasonologists working in the Tropics.
References
- Brandborg LL. Parasitic diseases. In: Sleisenger MH, Fordtran JS, eds. Gastrointestinal disease, Philadelphia: WB Saunders, 1978:1154–81.
- Khuroo MS, Zargar SA, Mahajan R. Hepatobiliary and pancreatic ascariasis in India. Lancet. 1990;335:1503–6.
- Khuroo MS. Hepatobiliary and pancreatic ascariasis. Indian J Gastroenterol. 2001;20:C28–32.
- Schulman A, Loxton AJ, Heydenrych JJ, Abdurahman KE. Sonographic diagnosis of biliary ascariasis. Am J Roentgenol. 1982;139:485–9.
- Khuroo MS, Zargar SA, Mahajan R, Bhat RL, Javid G. Sonographic appearance of biliary ascariasis. Gastroenterology. 1987;93:267–72.
- Kumar V, Shetty NM, Murthy VS. Sonography of biliary ascariasis. IJRI 1989;43:235–37.
- Singh SP, Meher C, Agrawal OP, Mohapatra MK. Hepatobiliary and pancreatic ascariasis in coastal Orissa. Indian J Gastroenterol. 1994;13:A98.
- Singh SP, Mohapatra MK, Agrawal OP, Meher C. Ultrasonographic demonstration of “inner tube sign”: a tropical dilemma. Indian J Gastroenterol 1997;16:A108.
- Khuroo MS. Ascariasis. Gastroenterol Clin North Am. 1996;25:553–77.
- Khuroo MS, Zargar SA, Yattoo GN,Javid G, Dar MY, Boda MI, et al. Worm extraction and biliary drainage in hepatobiliary and pancreatic ascariasis. Gastrointest Endosc. 1993;39:680–5.
- Sandouk F, Haffar S, Zada MM, Graham DY, Anand BS. Pancreatic-biliary ascariasis: experience of 300 cases. Am J Gastroenterol. 1997;92:2264–7.
- Shah OJ, Robanni I, Khan F, Zargar SA, Javid G. Management of biliary ascariasis in pregnancy. World J Surg. 2005;29:1294–8.
- Khuroo MS, Zargar SA. Biliary ascariasis: a common cause of biliary and pancreatic disease in an endemic area. Gastroenterology. 1985;88:418–23.
- Khuroo MS, Mahajan R, Zargar SA, Javid G, Sapru S. Prevalence of biliary tract disease in India: a sonographic study in adult population in Kasmir. Gut. 1989;30:201–5.
- Khuroo MS, Zargar SA, Yattoo GN, Koul P, Khan BA, Dar MY et al. Ascaris induced acute pancreatitis. Br J Surg. 1992;79:1335–8.
- Cerri GG, Leite GJ, Simoes JB, Correia Da Rocha DJ, Albuquerque FP, Machado MC, et al .Ultrasonographic evaluation of Ascaris in the biliary tract. Radiology. 1983;146:753–4.
- Ferreyra NP, Cerri GG. Ascariasis of the alimentary tract, liver, pancreas and biliary system: its diagnosis by ultrasonography. Hepatogastroenterology. 1998;45:932–7.
- Ali M, Khan AN. Sonography of hepatobiliary ascariasis. J Clin Ultrasound. 1996;24:235–41.
|
|
|
 |
|
|