|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Kundan Kumar*, Alakendu Ghosh**
Associate Specialist, Gastroenterology,*
Tata Main Hospital, Jamshedpur and
Professor, Dept of Internal Medicine**,
IPGMER, Kolkata, West Bengal, India
Corresponding Author:
Dr. Kundan Kumar
Email: kundanjip@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.249
48uep6bbphidvals|707 48uep6bbph|2000F98CTab_Articles|Fulltext Gastrointestinal manifestations of SLE are diverse and can involve the entire gastrointestinal system.[1] A syndrome of abdominal pain and diarrhoea in SLE can be due to pancreatitis, serositis, protein-losing enteropathy, gluten enteropathy, intestinal pseudo-obstruction, infection, and lupus enteritis/vasculitis. Lupus enteritis is defined as either vasculitis or inflammation of the small-bowel, with supportive image and/or biopsy findings (BILAG 2004).[2] Lupus enteritis is a rare complication of SLE, presumably mediated by immunecomplex deposition and complement activation, with subsequent submucosal edema. Abdominal computed tomography (CT) is the most useful diagnostic tool and is key
in leading to the correct diagnosis of lupus enteritis. We describe the case of a female patient presenting with recurrent intractable nausea, vomiting and diarrhoea in the absence of previously diagnosed SLE.
Case history
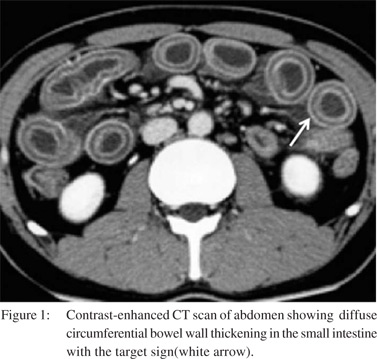
A 20 year-old-female patient was admitted to our hospital with severe nausea, vomiting and intractable watery diarrhea of one months’ duration (not responding to antibiotics, probiotics, fasting or antimotility agents) associated with abdominal pain, diminished urine output, and increased urinary frequency; Examination revealed pallor, dehydration, mild ascites and abdominal tenderness. She had three similar self-limiting episodes of nausea, vomiting and diarrhoea in the past two years, each requiring hospitalization and improved transiently with intravenous antibiotics and fluids over 3-4 week period. A history of occasional low grade fever was present in last two years. She had iron deficiency anaemia with a haemoglobin level of 7.2gm% and normal liver and renal function tests. 24 hour urinary protein estimation revealed proteinuria of 1.8g/day. Ultrasonography of whole abdomen revealed bilateral hydroureteronephrosis with edematous bladder wall and ascites. A contrast enhanced CT scan of the abdomen and pelvis showed diffuse circumferential bowel wall thickening in the small intestine (Target sign-Figure 1) in addition to ultrasonographic findings. Work up for auto immune parameters revealed antinuclear antibody- 1:160 (mixed homogenous and speckled pattern), anti-dsDNA antibody-91 u/ml (normal <55), complement C3-83.4 mg/dl (normal range 90- 180), lupus anticoagulant and anticardiolipin antibodies were negative. Upper GI endoscopy revealed mild erythema of gastric corpus and D2 biopsy was normal. Colonoscopy revealed diffuse mild erythema and edema of entire colonic mucosa with no ulcerations. In view of proteinuria, a renal biopsy was done.
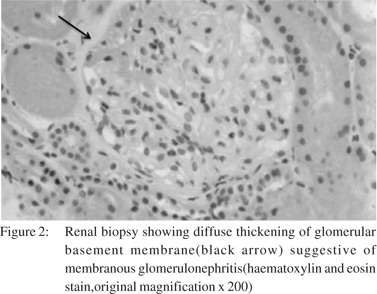
Histopathologic examination revealed membranous glomerulonephritis (Figure 2) and immunofluoroscence showed diffuse and granular IgG and C3 deposition suggestive of ISN/RPS[International Society of Pathology/Renal Pathology Society 2003] class V Lupus nephritis. She was treated with intravenous methylprednisolone (1g/ day) for three days followed by oral prednisolone (1mg/kg/ day), following which her symptoms resolved and hydroureteronephrosis subsided. In view of class v lupus nephritis she was also started on monthly pulse intravenous cyclophosphamide. Oral prednisolone was gradually tapered to a maintenance dose of 15 mg/day. Her proteinuria decreased on follow up and she remained asymptomatic till the last visit.
Discussion
The term lupus enteritis has been coined to describe a spectrum of intestinal inflammatory lesions in SLE. Lupus enteritis occurs in up to 53% of SLE patients.[3] Lupus enteritis is a potentially severe complication of SLE, stressing the need for swift diagnosis and adequate management. In a recent review of literature by Janssens et al[4] on 150 patients of lupus enteritis revealed abdominal pain (97%) as the most common symptom followed by vomiting (42%), diarrhea (32%) and fever (20%). 7% had complications in the form of intestinal necrosis or perforation, yielding a mortality rate of 2.7%. Half of the patients have proteinuria. Lupus enteritis is frequently associated with lupus cystitis.[5] Transient hydroureteronephrosis with obstructive urinary symptoms is the common manifestation with prompt resolution on steroid therapy. Untreated cases may evolve to intestinal necrosis and perforation leading to death. Adding with this an excellent steroid responsiveness, timely diagnosis becomes primordial for the adequate management of this rare entity.
Acknowledgment
To the patient and their family members who showed interest and gave permission for publication of their case.
References
- Hallegua DS, Wallace DJ. Gastrointestinal manifestations of systemic lupus erythematosus. Curr Opin Rheumatol. 2000;12:379–85.
- Isenberg DA, Rahman A, Allen E, Farewell V, Akil M, Bruce IN, et al: BILAG 2004. Development and initial validation of an updated version of the British Isles Lupus Assessment Group’s disease activity index for patients with systemic lupus erythematosus. Rheumatology (Oxford) 2005:44:902–6.
- Sultan SM, Ioannou Y, Isenberg DA. A review of gastrointestinal manifestations of systemic lupus erythematosus. Rheumatology. 1999;38:917–32.
- Janssens P, Arnaud L, Galicier L, Mathian A, Hie M, Sene D, et al. Lupus enteritis: from clinical findings to therapeutic management. Orphanet Journal of Rare Diseases 2013,8:67.
- Shimizu A, Tamura A, Tago O, Abe M, Nagai Y, Ishikawa O.Lupus cystitis: a case report and review of the literature. Lupus 2009;18:655–8.
|
|
|
 |
|
|