48uep6bbphidvals|703
48uep6bbph|2000F98CTab_Articles|Fulltext
Gastrointestinal stromal tumors (GIST) in the pelvis can cause intestinal obstruction or symptoms mimicking benign prostatic hyperplasia.[1]
Case Report
A 32-year-old man presented with rectal bleeding and passage of fleshy pieces per rectum, for 4 months. He also had constipation, distension of abdomen and occasional vomiting. 5 months ago he had presented with fever, burning micturition and urinary retention at another hospital. Sonography and computed tomography of the abdomen had suggested a diagnosis of prostatic abscess. He thenunderwent transurethral drainage of 700 ml pus; and culture had shown a growth of E.coli.He had repeated episodes of retention of urine, which was relieved only by catheterization.
On presentation at our institution, he was afebrile, pale, hypotensive and had tachycardia. Foley’s catheter was in-situ in the urinary bladder. Abdomen revealed distension,no guarding or rigidity, a non-tender, hard lump in the hypogastrium, increased bowel sounds and no ascites. On digital rectal examination, a hugely enlarged prostatic mass was palpable; havinga defect through which the exploratory finger entered a cavity. The overlying rectal mucosa was fixed. Proctosigmoidoscopy was not possible because of the compromised rectal lumen,filled with soft-tissue pieces, which were sent for histopathological examination. Hemoglobin was 4.5 g/dL. Urine culture, TLC, fasting blood sugar, CEA, PSA and tests for HIV, were normal.
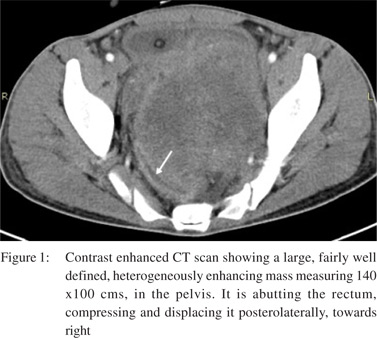
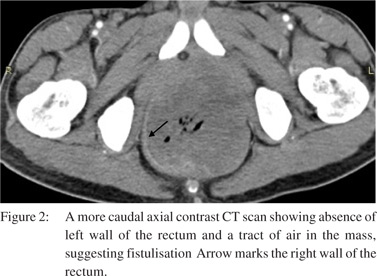
On transabdominal ultrasound, a solid-appearing, heteroechoic lesion was seen elevating the base of the urinary bladder. No cystic area or color flow was seen. Contrast enhanced CT revealed a large, heterogeneously enhancing solid lesion, inseparable from the base of the urinary bladder and compressing the rectum (Figure 1). The prostate gland and seminal vesicles could not be identified. There was absence of a part of the left rectal wall and air foci seen tracking into the lesion (Figure 2). Rounded, hypodense lesions in the liver; and pleural effusion with subpleural, enhancing, solid masses on the left side suggesting metastases, were also observed. The provisional diagnosis was prostatic leiomyosarcoma or rhabdomyosarcoma. A diverting loop transverse colostomy was made.
Histopathology revealed a normal rectal mucosa. Submucosa showed a mesenchymal tumor with large areas of necrosis and hemorrhage. No prostatic tissue was identified. Tumor showed positivity for CD117 and Vimentin; Epithelial membrane antigen was negative. A diagnosis of GIST was made based on histopathology and immunohistochemical studies. The patient was referred to an oncology center, where he has been prescribed Imatinib Mesylate.
Discussion
It is hypothesized that GISTs originate from mutations of the interstice of the Cajal cells, which are “pacemaker” cells from the gastrointestinal system. Recent studies have also revealed the presence of these cells inside the urinary tract’s interstice in smooth muscle cells from bladder, prostate and urethra.1 Prostatic GIST may present with dysuria, urinary retention, rectal fullness or urinary obstructive symptoms.[2] Rectal GISTs can result in altered intestinal function, rectal bleeding in case of ulceration, abdominal pain, and urinary symptoms attributable to bladder compression. When located in the anterior wall of the rectum in male patients, they might cause difficulties in urination along with pelvic and perineal pain, producing symptoms similar to prostatism.
References
- deCarvalho JPM, Rozado JPGM, Araujo AVG, de Carvalho PCN. Primary and confined gist of the prostate: Case report and review of literature. J Med Med Sci. 2010;1:185–7.
- Van der Aa F, Sciot R, Blyweert W, Ost D, Van Poppel H, VanOosterom A, Debiec-Rychter M, De Ridder D. Gastrointestinal stromal tumor of the prostate. Urol. 2005;65:388.