48uep6bbphidvals|688
48uep6bbph|2000F98CTab_Articles|Fulltext
Liver abscess is a common clinical problem encountered in the tropics. In India, most cases are due to amebiasis or are pyogenic, secondary to portal pyemia. In appropriate clinical settings, anti-amebic therapy or empirical antibiotic therapy is instituted. If there is no clinical improvement, image guided abscess drainage or aspiration is done for microbiological analysis and treatment is modified accordingly. We describe two such patients who had failed to improve with initial empirical therapy for amebiasis or pyogenic liver abscess and were diagnosed to have melioidosis.
Case reports
Case 1
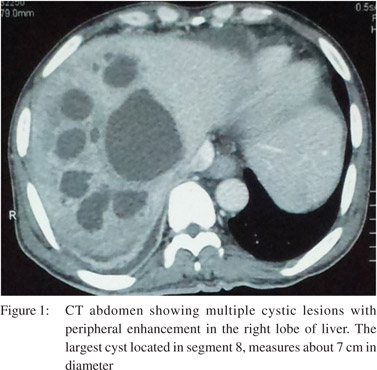
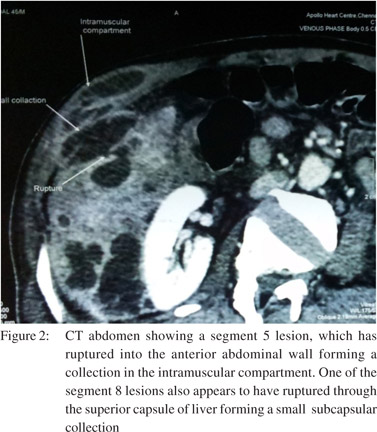
A 51-year-old diabetic man from Orissa presented with a history of low-grade fever, progressive left-lower-quadrant abdominal pain for three months. He was treated in another hospital for pyogenic liver abscess with intravenous piperacillin/tazobactam based on blood culture report positive for Pseudomonas spp. Abdominal examination revealed non-tender hepatosplenomegaly. Blood investigations revealed anemia (hemoglobin: 9gm/dl), normal WBC count (6,000/mm3), raised erythrocyte sedimentation rate (80 mm in 1 hr), hypoalbuminemia (2.5gm/dl), and elevated alkaline phosphatase (888U/L). Remaining liver function tests were within normal limits. The chest radiograph was normal. CECT abdomen showed the presence of multiple liver abscesses with subdiaphragmatic collections (Figures 1 & 2). Blood culture grew Burkholderia pseudomallei. Ceftazidime was instituted as per antimicrobial sensitivity. In view of the subdiaphragmatic collection, laparoscopic drainage of the liver abscesses was done. The patient gradually recovered and was discharged on cotrimoxazole for 6 months.
Case 2
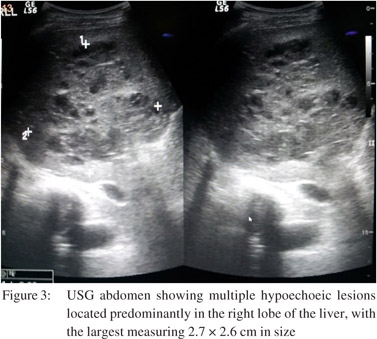
A 50-year-old farmer from Tirupathi, with diabetes mellitus, was admitted with fever, abdominal pain and vomiting for two months. He was treated at another hospital for liver abscess with intravenous metronidazole and USG guided abscess drainage was done with little improvement. On examination, he had tachycardia with hypotension and tenderness in the right hypochondrium. Investigations revealed anemia, leukocytosis, low platelet count, altered LFT (increased AST, GGTP and ALP, and hypoalbuminemia). Chest radiograph showed right lower zone non-homogenous opacity. USG abdomen showed a mixed echogenic heterogeneous lesion with multiple anechoic to hypoechoic areas within the right lobe of liver. Splenomegaly with portal and superior mesenteric venous thrombosis was also noted (Figure 3). USG guided aspiration of the liver lesion was sent for culture. He was initially resuscitated with intravenous fluids, inotropes,and empirical intravenous cefaperazone/ sulbactam. Pus culture grew Burkholderia pseudomallei. The antibiotic was changed to ceftazidime and cotrimoxazole. He gradually improved and was advised to continue cotrimoxazole for 6 months.
 Discussion
Burkholderia pseudomallei (formerly, Pseudomonas pseudomallei) is a bipolar-staining, Gram-negative aerobic bacillus and is found in the tropics, mainly between latitudes 20° north and 20° south.[1] It was first recognised in Burma in 1912 by Whitemore and Krishnaswami.[2,3] The organism enters the human host through a preexisting skin abrasion or by inhalation and ingestion. It resides in the soil and water in locations such ascultivated fields, drains, gardens and playgrounds.[4] Melioidosis occurs more frequently in patients with underlying diseases, such as diabetes mellitus, chronic renal failure, alcoholism, malignancy or haematological disorders, or thosewho are immunosuppressed as the result of either disease ortherapy. In patients without underlying disease, occupational exposure to soil is an important risk factor.[5,6] Both our patients were diabetic and farmers. The clinical manifestations of melioidosis range from acute localized forms, acute septicemia to chronic forms. Septicemia is the most common presentation. The lung is the most commonly affected organ.[1,5] The spleen is the most common intra-abdominal organ infected by melioidosis, followed by the liver and kidney.[6] Many reports of melioidosis with abscessesat unusual sites such as the neck[7] parotid,[8] have been published from India.Visceral organ abscesses appear on ultrasoundas multiple and small hypoechoic lesions, target lesions and multiloculated lesions.On CT, the “necklace sign” or the”honeycomb sign” with multiloculated lesions are characteristic of melioidotic abscesses.[9] Concurrent liver and splenic abscesses are more likely to be associated with melioidosis than other micro organisms. Definitive diagnosis is made by culture and isolation of the organism from blood or infected organ.[4,9] The treatment of choice is intravenous ceftazidime (or) meropenem 6-8 hourly followed by 3-6 months of co-trimoxazole (or) doxycycline therapy. The mortality rate in the acute septicemic form exceeds 50% if patients do not receive appropriate treatment.[4,6]
Discussion
Burkholderia pseudomallei (formerly, Pseudomonas pseudomallei) is a bipolar-staining, Gram-negative aerobic bacillus and is found in the tropics, mainly between latitudes 20° north and 20° south.[1] It was first recognised in Burma in 1912 by Whitemore and Krishnaswami.[2,3] The organism enters the human host through a preexisting skin abrasion or by inhalation and ingestion. It resides in the soil and water in locations such ascultivated fields, drains, gardens and playgrounds.[4] Melioidosis occurs more frequently in patients with underlying diseases, such as diabetes mellitus, chronic renal failure, alcoholism, malignancy or haematological disorders, or thosewho are immunosuppressed as the result of either disease ortherapy. In patients without underlying disease, occupational exposure to soil is an important risk factor.[5,6] Both our patients were diabetic and farmers. The clinical manifestations of melioidosis range from acute localized forms, acute septicemia to chronic forms. Septicemia is the most common presentation. The lung is the most commonly affected organ.[1,5] The spleen is the most common intra-abdominal organ infected by melioidosis, followed by the liver and kidney.[6] Many reports of melioidosis with abscessesat unusual sites such as the neck[7] parotid,[8] have been published from India.Visceral organ abscesses appear on ultrasoundas multiple and small hypoechoic lesions, target lesions and multiloculated lesions.On CT, the “necklace sign” or the”honeycomb sign” with multiloculated lesions are characteristic of melioidotic abscesses.[9] Concurrent liver and splenic abscesses are more likely to be associated with melioidosis than other micro organisms. Definitive diagnosis is made by culture and isolation of the organism from blood or infected organ.[4,9] The treatment of choice is intravenous ceftazidime (or) meropenem 6-8 hourly followed by 3-6 months of co-trimoxazole (or) doxycycline therapy. The mortality rate in the acute septicemic form exceeds 50% if patients do not receive appropriate treatment.[4,6]
In summary, melioidosis should be thought of and evaluated for in patients with underlying risk factors who present with multiple liver abscesses. If appropriate treatment is not instituted, there is high risk of mortality.
References
- Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416.
- Whitmore A. An Account of a Glanders-like Disease occurring in Rangoon. J Hyg (Lond). 1913;13:1–34.
- Whitmore A, Krishnaswami CS. An account of the discoveryof a hitherto underscribed infective disease occurring among the populationof Rangoon. Ind Med Gazette. 1912;47:262–7.
- Limmathurotsakul D, Peacock SJ. Melioidosis: a clinical overview. Br Med Bull. 2011;99:125–39.
- Currie BJ, Jacups SP, Cheng AC, Fisher DA, Anstey NM, Huffam SE, et al. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop Med Int Health. 2004;9:1167–74.
- Currie BJ, Ward L, Cheng AC. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoSNegl Trop Dis. 2010;4:e900.
- Mathew S, Perakath B, Mathew G, Sitaram V, Nair A, Lalitha MK, et al. Surgical presentation of melioidosis in India. Natl Med J India. 1999;12:59–61.
- Shivbalan S, Reddy N, Tiru V, Thomas K. Systemic melioidosis presenting as suppurativeparotitis. Indian Pediatr. 2010;47:799–801.
- Apisarnthanarak P, Thairatananon A, Muangsomboon K, Lu DS, Mundy LM, Apisarnthanarak A. Computed tomography characteristics of hepatic and splenic abscesses associated with melioidosis: a 7-year study. J Med Imaging Radiat Oncol. 2011;55:176–82.