|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Chintamani B God couponrxsms.com discountbole1, Dhaval O Mangukiya1, Ritu Kakkar-Kashikar2, Nilesh H Doctor1
Departments of Surgical Gastroenterology1 and Radiology,2
Jaslok Hospital and Research Centre,
GD Deshmukh Marg, Mumbai - 400026
Corresponding Author:
Dr. Nilesh H Doctor
Email: drnileshbela@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.226
48uep6bbphidvals|684 48uep6bbph|2000F98CTab_Articles|Fulltext Actinomyces are anaerobic gram positive filamentous bacteria known to cause chronic suppurative infections. The sites of infection are classified as cervicofacial, thoracic and abdominopelvic and rarely the central nervous system. Actinomycosis of the hepatobiliary system is rare and the clinical and radiological features often are confused with malignancy.[1-4] We report here two cases of actinomycosis involving the liver and the gall bladder which mimicked malignant tumors at presentation and the diagnosis of actinomycosis was established by histopathology of resected specimens.
Case reports
Case1
A 50-year-old lady on regular treatment for diabetes, presented with pain right hypochondriumsince 15 days.Prior to this the pain had been mild and intermittent for a year and wasrelieved by analgesics. There was no history of fever, vomiting, nausea, jaundice, anorexia or weight loss. On physical examination, she had mild tenderness in the right hypochondrium. She had a history of abdominal surgery 30 years ago, through a right subcostal incision, details of which were not available. Her liver function tests were normal.
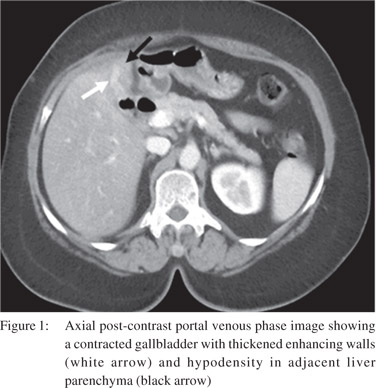
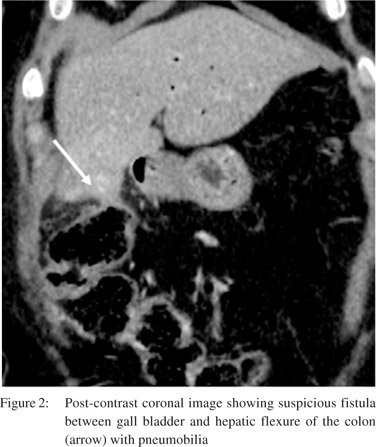
Ultrasound abdomenshoweda shrunken thick-walled gallbladder with calculi and focal thickening near the fundus with presence of pneumobilia. The common bile duct was prominent with 9 mm size. A contrast-enhanced CT scan of the abdomen confirmed the ultrasound findings and also showed a focal hypodensity in the adjacent liver parenchyma (Figure 1). There was also a suspicion of a cholecysto-colic fistula in view of the pneumobilia and the transverse colon appearingdensely adherent to the gall bladder fundus (Figure 2).
 The patient underwent exploratory laparotomy which showed a thick-walled shrunken gallbladder with adhesions to duodenum. The gallbladder and surrounding liver tissue was hard on palpation. There was a cholecysto-colic fistula between the gallbladder fundus and the transverse colon. There was an area of focal thickening around the fistula site. These features were highly suggestive of a malignant etiology, hence a frozen section was first sent from the gall bladder wall which showed benign tissue. Hence the fistula was disconnected and the colon was sutured primarily.Cholecystectomy was completed and the entire gallbladder was sent for a frozen section. There was no malignancy reportedin the frozen section and hence a radical resection was not performed.
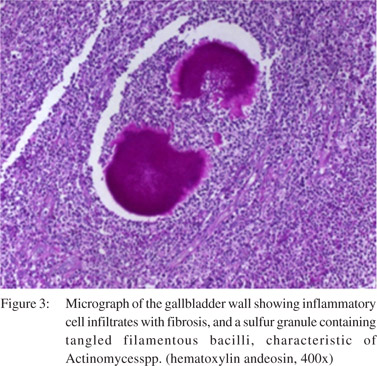
On histopathology of the gallbladder, features of chronic inflammation were seen with few sections showing actinomycotic granules with filamentous bacteria surrounded by inflammatory cells (Figure 3). There was no evidence of any dysplasia or malignancy.The patient was discharged on oral amoxicillin for six months.
The patient underwent exploratory laparotomy which showed a thick-walled shrunken gallbladder with adhesions to duodenum. The gallbladder and surrounding liver tissue was hard on palpation. There was a cholecysto-colic fistula between the gallbladder fundus and the transverse colon. There was an area of focal thickening around the fistula site. These features were highly suggestive of a malignant etiology, hence a frozen section was first sent from the gall bladder wall which showed benign tissue. Hence the fistula was disconnected and the colon was sutured primarily.Cholecystectomy was completed and the entire gallbladder was sent for a frozen section. There was no malignancy reportedin the frozen section and hence a radical resection was not performed.
On histopathology of the gallbladder, features of chronic inflammation were seen with few sections showing actinomycotic granules with filamentous bacteria surrounded by inflammatory cells (Figure 3). There was no evidence of any dysplasia or malignancy.The patient was discharged on oral amoxicillin for six months.
Case 2
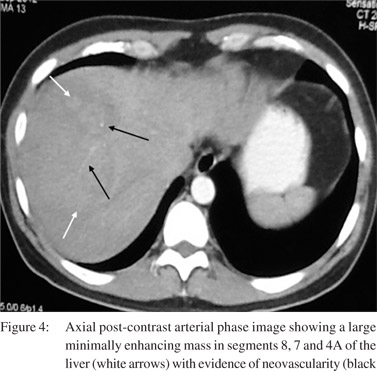
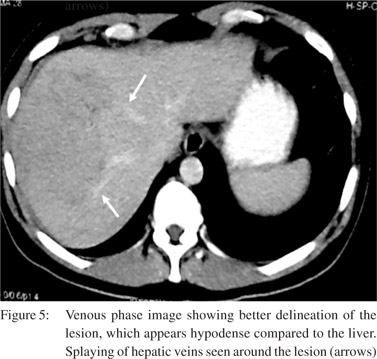
A 42-year-old gentleman presented withanorexia, low grade fever and weight loss of 20kg over three months. He had no previous medical or surgical history and had no addictions. Ultrasound detected a solid hypoechoic lesion in the right lobe of the liver.A contrast-enhanced CT scan showed during thepost-contrast arterial phase,a large minimally enhancing mass in segments 8, 7 and 4a of the liver with evidence of neovascularity (Figure 4). The venous phase showed better delineation of the lesion, which appearedhypodense as compared to the liver (Figure 5). Splaying of hepatic veins was seen around the lesion.In view of the above imaging features, the possibility of hepatocellular carcinoma was regarded.
Serum alpha fetoprotein level wasnormal. The patient underwent a CT guided biopsy which showed only inflammatory cells. CT volumetry suggested inadequate remnant left lobe volume. Hence, right portal vein embolization was performed along with transarterial chemoembolisation of the tumour. A repeat CT scan after 4 weeks confirmed left lobe hypertrophy and shrinkage of the lesion.
He underwent alaparotomy which showed a firm mass in the right lobe of the liver with adhesions to the diaphragm. There was no evidence of pus on aspiration of the lesion. Though a frozen section examination done from the lesion showed no evidence of malignancy, a formal right hepatectomy was performed in view of the strong suspicion of hepatocellular carcinoma. The post-operative course was uneventful. The final histopathology showed actinomycotic involvement of the liver.The patient received injection penicillin G for two weeks and was then given oral amoxicillin for six months. He has currently completed eight months follow-up and is symptomatic with no new liver lesions confirmed by imaging.
Discussion
Primary actinomycosis involving the hepatobiliary system is rare. Literaturere view reveals only sporadic case reports and small case series. The predisposing factors include previous upper abdominal surgery, perforation peritonitis and abdominal wall trauma.[2] Some studies have shown a higher risk of infection following biliary and pancreatic stenting.[5,6] Hepatic actinomycosis predominantly affects males in the age group of 40 to 60 years.[2-5] Although it was previously thought to be more common in immunosuppressed patients, recent reviews suggest that most patients are immunocompetent.[2,4] The exact etiology cannot be found in most cases, but prior bowel surgery may be associated.[3] Radiological investigations most commonly show a hypoechoic mass in the liver on ultrasound with cystic areas. A CT scan may show heterogenous mass in the liver, which is solitary in about 2/3rd of cases. The mass commonly shows peripheral enhancement with central hypodense areas suggestive of necrosis.[2-4] The mass is poorly demarcated from the surrounding liver parenchyma indicating local invasion mimicking a malignancy. Actinomycosis of the gall bladder is an extremely rare condition and to our knowledge, there are less than 30 reported cases in the literature. It usually occurs after the age of 50 years with no obvious gender predilection.[6]
The most common symptom is pain in right upper quadrant of abdomen. Some cases may also present as acutecholecystitiswith pain, fever and tenderness. Ultrasound findings in most cases include a thickened gallbladder with or without features ofcholecystitis. Treatment with antibiotics is as important as surgery since actinomycosis is prone to recurrences. Penicillin G is the drug of choice and has to be given over a prolonged period of 2 to 6 weeks followed by oral amoxicillin or penicillin to be continued for 6 months to 1 year. Doxycycline, minocycline, tetracycline, clindamycin, erythromycin, and cephalosporinshave also been shown to be effective.[6]
References
- Kyle Anderson, MD, Joseph M. Scherger, MD.Actinomycosis. First Consult. Elsevier.Jan–2012.
- Wayne MG, Narang R, Chauhdry A, Steele J. Hepatic actinomycosis mimicking an isolated tumor recurrence. World J Surg Oncol. 2011;9:70.
- Hayashi M, Asakuma M, Tsunemi S, Inoue Y, Shimizu T, Komeda K, et al. Surgical treatment for abdominal actinomycosis: A report of two cases. World J Gastrointest Surg. 2010;2:405–8.
- Lai AT, Lam CM, Ng KK, Yeung C, Ho WL, Poon LT, et al. Hepatic actinomycosis presenting as a liver tumour: case report and literature review. Asian J Surg. 2004;27:345–7.
- Kanellopoulou T, Alexopoulou A, Tanouli MI, Tiniakos D, Giannopoulos D, Koskinas J, et al. Primary hepatic actinomycosis. Am J Med Sci. 2010;339:362–5.
- Acevedo F, Baudrand R, Letelier LM, Gaete P. Actinomycosis: a great pretender. Case reports of unusual presentations and a review of the literature. Int J Infect Dis. 2008;12:358–62.
|
|
|
 |
|
|