|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Srinivas M, Uthappa MC, Palaniappan S, Jayanthi V
Department of Gastroenterology, Global Health City,
Cheran Nagar, Perumbakkam, Chennai - 600100, India
Corresponding Author:
Dr. M Srinivas
Email: drsrinivasm@hotmail.com
DOI:
http://dx.doi.org/10.7869/tg.209
48uep6bbphidvals|633 48uep6bbph|2000F98CTab_Articles|Fulltext Visceral artery aneurysm (VAA) is often asymptomatic and discovered incidentally. Reports on ileocolic artery aneurysms (ICAA) are rare and mostly anecdotal. Therapeutic options include surgery or radiology-guided endovascular measures. We report a case of spontaneous ICAA where N-butyl cyanoacrylate (NBCA) glue was used to achieve embolisation percutaneously under ultrasound guidance.
Case report
An 81-year-old gentleman presented with two weeks history of lower abdominal pain. The pain was dull aching, continuous with no radiation or aggravation by food. There were no associated systemic symptoms like fever, loss of appetite or weight loss. Bowel and bladder habits were unaltered. He had chronic obstructive pulmonary disease and Parkinson’s disease. He was treated successfully by Heller’s cardiomyotomy for achalasia in 2008, with difficult endotracheal intubation prior to anaesthesia.
On examination, the patient was afebrile with other vital parameters being normal. On deep palpation tenderness was noted in the hypogastrium. There were no signs of gut obstruction or any palpable mass. Hemogram, urine examination, renal and liver function tests were normal. Ultrasound abdomen with Doppler (Figure 1A) showed a 3×3 cm pulsatile aneurysm. The origin of the aneurysm was unclear. The abdominal aorta, its bifurcation, the celiac and superior mesenteric arteries at their origins were all normal with no evidence of thrombosis. CT angiography (Figure 2) performed to identify the origin of the aneurysm, showed a 4.5×4 cm aneurysm filled with a partial thrombus originating from the ileocolic branch of superior mesenteric artery (SMA), with no other aneurysms elsewhere in the abdomen. The afferent artery was 2 mm in size. 2 ml NBCA was injected into the aneurysm percutaneously under ultrasound guidance with no complications. The patient improved symptomatically within 24 hours post-procedure. At 4 weeks follow-up the patient was asymptomatic and Doppler ultrasound showed complete embolisation of the aneurysm (Figure 1B).
Discussion
VAA are intra-abdominal aneurysms that affect the celiac, superior and inferior mesenteric, renal arteries and their branches. Identified mostly in older people (age >60) of either gender, aneurysms of jejunal, ileal and colic arteries put together account for only 3% of all VAAs. Aneurysms of the ileocolic branch (ICAA) of SMA are very uncommon and usually anecdotal.[1] Although predominantly asymptomatic and detected incidentally, ICAAs can present with abdominal pain or nausea. Aneurysm rupture may manifest with pain, gastrointestinal blood loss or intra-abdominal haemorrhage.[2] The only previous Indian report on ICAA was by Sharma et al who described a case following minor trauma which resolved spontaneously.[3] The pathogenesis of ICAAs is unclear but most occur due to septic emboli,[4,5] vasculitis, trauma, dissection, fibromuscular dysplasia or degeneration.[6] The last two causes were most likely responsible for the aneurysm in our patient.
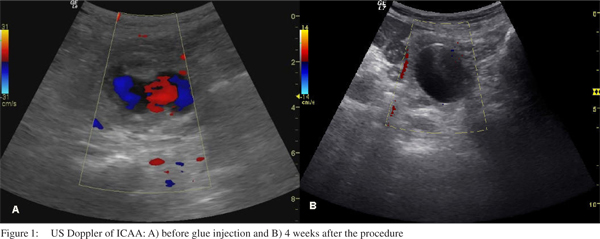
 Doppler ultrasound is the diagnostic modality of choice for suspected SMA aneurysms, but localization becomes difficult when one of its branches is involved.[7] Hence confirmation of the actual site and detection of other concomitant aneurysms is always performed by CT angiography,[8], as was done in our case. With the risk of rupture approaching 50%, treatment is indicated for most SMA aneurysms.[5] Treatment options include surgery or endovascular interventional techniques, depending on the patient’s hemodynamic status and surgical risk. Surgical options include aneurysmectomy, aneurysmorrhaphy or ligation (with or without arterial reconstruction). In view of the previous difficulties encountered at endotracheal intubation in our patient and his age, we decided against surgical intervention in this case. Endovascular measures involve stenting (“endovascular exclusion”) or using coils, thrombin or glue to embolise the aneurysm sac. Lagana et al[9] report a 10% reperfusion at one month after a single endovascular intervention (29 VAAs, 18.7 months mean follow-up), and no reperfusion after a second endovascular procedure. An American follow-up study[10] on 48 VAAs reported NBCA use in 19% procedures for persistent flow or multiple branches yielding good results. The choice of endovascular intervention is dictated by size of the vessel, presence of multiple feeders and local experience. We chose NBCA in our patient due to the small size of the efferent artery (not ideal for stenting), its lower cost and ease of preparation compared to thrombin. The percutaneous route was selected based on the estimation that the aneurysm was accessible through a safe, avascular plane under ultrasound guidance. While our patient’s abdominal pain resolved within 24 hours, total embolisation of the aneurysm was confirmed 4-week follow-up.
To the best of our knowledge this is the first Indian case report of spontaneous ICAA treated by ultrasound guided percutaneous primary glue embolisation. We suggest this treatment option as a feasible and effective modality for aneurysm embolisation in patients where surgery is deemed unsuitable and local expertise for endovascular stenting or coil embolisation are unavailable.
References
Doppler ultrasound is the diagnostic modality of choice for suspected SMA aneurysms, but localization becomes difficult when one of its branches is involved.[7] Hence confirmation of the actual site and detection of other concomitant aneurysms is always performed by CT angiography,[8], as was done in our case. With the risk of rupture approaching 50%, treatment is indicated for most SMA aneurysms.[5] Treatment options include surgery or endovascular interventional techniques, depending on the patient’s hemodynamic status and surgical risk. Surgical options include aneurysmectomy, aneurysmorrhaphy or ligation (with or without arterial reconstruction). In view of the previous difficulties encountered at endotracheal intubation in our patient and his age, we decided against surgical intervention in this case. Endovascular measures involve stenting (“endovascular exclusion”) or using coils, thrombin or glue to embolise the aneurysm sac. Lagana et al[9] report a 10% reperfusion at one month after a single endovascular intervention (29 VAAs, 18.7 months mean follow-up), and no reperfusion after a second endovascular procedure. An American follow-up study[10] on 48 VAAs reported NBCA use in 19% procedures for persistent flow or multiple branches yielding good results. The choice of endovascular intervention is dictated by size of the vessel, presence of multiple feeders and local experience. We chose NBCA in our patient due to the small size of the efferent artery (not ideal for stenting), its lower cost and ease of preparation compared to thrombin. The percutaneous route was selected based on the estimation that the aneurysm was accessible through a safe, avascular plane under ultrasound guidance. While our patient’s abdominal pain resolved within 24 hours, total embolisation of the aneurysm was confirmed 4-week follow-up.
To the best of our knowledge this is the first Indian case report of spontaneous ICAA treated by ultrasound guided percutaneous primary glue embolisation. We suggest this treatment option as a feasible and effective modality for aneurysm embolisation in patients where surgery is deemed unsuitable and local expertise for endovascular stenting or coil embolisation are unavailable.
References
- Roche-Nagle G, O’Donnell D, O’Hanrahan T. Visceral artery aneurysms: a symptomatic aneurysm of the ileocolic artery. Vascular. 2007;15:162–6.
- Chou TF, Chang S, Chuang CD, Chang H, Chang KJ, Hung CR. Aneurysm arising from the branch of the superior mesenteric artery. J Formos Med Assoc. 1991;90:853–6.
- Sharma AK, Mishra PK, Chibber S, Aditya. Spontaneous resolving of the aneurysm of ileocolic artery, branch of superior mesenteric artery - imaging findings. Indian J Radiol Imaging. 2006;16:559–62.
- Stone WM, Abbas M, Cherry KJ, Fowl RJ, Gloviczki P. Superior mesenteric artery aneurysms: is presence an indication for intervention? J Vasc Surg. 2002;36:234–7; discussion 7.
- Komori K, Mori E, Yamaoka T, Ohta S, Takeuchi K, Matsumoto T, et al. Successful resection of superior mesenteric artery aneurysm. A case report and review of the literature. J Cardiovasc Surg (Torino). 2000;41:475–8.
- Messina LM, Shanley CJ. Visceral artery aneurysms. Surg Clin North Am. 1997;77:425–42.
- Bates K, Sorrell K, Carpenter J. Superior mesenteric artery aneurysm identified by color duplex ultrasonography: two case reports. J Vasc Tech. 2001;25:226–30.
- Nosher JL, Chung J, Brevetti LS, Graham AM, Siegel RL. Visceral and renal artery aneurysms: a pictorial essay on endovascular therapy. Radiographics. 2006;26:1687–704.
- Lagana D, Carrafiello G, Mangini M, Dionigi G, Caronno R, Castelli P, et al. Multimodal approach to endovascular treatment of visceral artery aneurysms and pseudoaneurysms. Eur J Radiol. 2006;59:104–11.
- Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, et al. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45:276–83; discussion 83.
|
|
|
 |
|
|