|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Chronic pancreatitis, alcoholic chronic pancreatitis, tropical chronic pancreatitis, idiopathic chronic pancreatitis |
|
|
Gopalakrishna Rajesh, Banavara Narasimhamurthy Girish, Suprabha Panicker, Vallath Balakrishnan
Departments of Gastroenterology,
Amrita Institute of Medical
Sciences, Kochi
AIMS Ponekkara P.O.
Cochin – 682 041, Kerala,
India
Corresponding Author:
Vallath Balakrishnan
Email: vbalakrishnan@aims.amrita.
edu
DOI:
http://dx.doi.org/10.7869/tg.204
Abstract
Background: Recent reports indicate a decline in prevalence of classical tropical chronic pancreatitis (TCP). We studied the etiologies and risk factors over a 14-year period at a tertiary care university hospital.
Methods: We compared the etiology in chronic pancreatitis (CP) patients presenting and followed-up in our Pancreas Clinic over two time periods (2000-06 and 2007-13).
Results: Idiopathic chronic pancreatitis (ICP) was the predominant etiology seen over the two time periods. However an increase in prevalence of alcoholic chronic pancreatitis (ACP) during the latter time period suggests that it may be emerging as a dominant etiology over recent years. Hypertriglyceridemia and hyperparathyroidism were uncommon causes of nonalcoholic CP. Autoimmune pancreatitis was noted only during 2007-13, but remains a rare cause of CP. There are multiple risk factors for CP in our population.
Conclusions: The high prevalence of ICP indicates need closer examination of risk factors and ICP pathogenesis. ACP appears to be emerging as a dominant cause of CP which suggests a
need to reorient preventive strategies.
|
48uep6bbphidvals|628 48uep6bbph|2000F98CTab_Articles|Fulltext Chronic pancreatitis (CP) is a progressive inflammatory disease of the pancreas characterized by irreversible morphological changes typically causing pain and/or permanent loss of function. Tropical pancreatitis was first described in the 1950s and was the dominant etiology in Kerala. Tropical pancreatitis which has been reported in India especially in Kerala state, is characterized by abdominal pain, large intraductal calculi, diabetes mellitus, and is complicated by a high incidence of pancreatic cancer seen in young, non-alcoholic subjects.[1] While the traditional risk factors implicated in TCP included malnutrition, dietary toxins and environmental agents, there is emerging evidence about the role of genetics. However patients similar to those described as tropical pancreatitis comprised only 3.8% in a large multicentre study in India.[2] Improvements in healthcare and socioeconomic conditions have yielded better outcomes. There has been a rising trend of alcohol consumption in Kerala, which incidentally has the highest per capita consumption of alcohol among Indian states.[3] Improvements in socioeconomic conditions, lifestyle and dietary changes and an increase in alcoholism and smoking are some important factors influencing CP.[4] In this study we compared the etiological factors in CP patients over a 14 year period from January 2000 to December 2013.
Methods
We studied and compared the etiology of CP in patients enrolled and followed-up at our Pancreas Clinic over two time periods, spanning from 2000-2006 and 2007-2013. Chronic pancreatitis was diagnosed as per standard clinical and imaging criteria (employing US, CT, ERCP, MRCP, and/or EUS). Alcohol intake and smoking habits were assessed in detail using a standard proforma administered by a trained medical social worker. Alcoholic chronic pancreatitis (ACP) was diagnosed in CP patients who had been consuming >80 g alcohol/day for at least five years. Idiopathic chronic pancreatitis (ICP) was diagnosed if pre-existing conditions likely to cause CP (primary hyperparathyroidism, hypertriglyceridemia, hereditary pancreatitis, and excess alcohol consumption) were ruled out.
Autoimmune pancreatitis was diagnosed as per previously reported criteria. The etiological and risk factors for the two time periods were compared using the Chi-square test. A p value <0.05 was considered significant. Statistical analysis was performed using SPSS v11.0.
Results
The demographic features of CP patients over the two time periods are shown in Table 1. There was slight increase in prevalence of CP in the latter time period (594 patients vs. 524 in the earlier time period). The mean age at diagnosis was higher in the latter time period (37.59±15.26 years vs. 27.89±13.87 years, p=0.014). Pain was the dominant symptom across both time periods. Prevalence of exocrine and endocrine insufficiency was comparable.
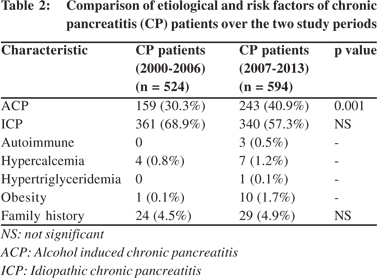
The etiological and risk factors are compared in Table 2. A significant finding was the increase in ACP prevalence during the latter time period. Rare causes showed no statistical difference between the two time periods except for autoimmune pancreatitis. While there were no significant differences in hereditary causes or family history, high prevalence of obesity in our patients drew attention and could be a novel risk factor.

Discussion
The first large series reported by Geevarghese reported a high prevalence of CP in Kerala.[5] A field survey in Kollam district of Kerala involving 28,567 inhabitants (6,079 families) reported the prevalence to be 1 in every 793 individuals.[6] This study also showed a female predominance (M:F ratio: 1:1.8) unlike hospital data. Tropical pancreatitis is now reported from most parts of India, and the Asia–Pacific survey (2004) showed prevalence of 114–200 per 100,000 population in India.[7] The nationwide IPANS study showed that ICP comprised about two-thirds and ACP nearly one-third of CP patients in India.[2] In western countries, alcohol remains the most frequent factor associated with CP. A multi-centre study from Italy[8] reported alcohol consumption as the principal factor in 34% of CP cases while the same figure approached 44% in the United States.[9] Surveys from Japan report ACP in ~60% of CP cases.[10] A study on drinking habits in alcoholic pancreatitis patients in Japan revealed gender and age differences.[11] It was observed that female patients developed alcoholic pancreatitis at a younger age, over shorter duration and with smaller cumulative amounts of alcohol consumption than the male patients. Male smokers developed alcoholic pancreatitis at younger age than non-smokers.
In this study we observed an increase in ACP cases over time. The rise possibly reflects an increase in alcoholism. This disturbing trend needs appropriate intervention. However unlike many series of CP from other countries, the Indian IPANS study showed that ICP comprised the major proportion (60%) of CP cases. Pezzilli commented that the high prevalence of ICP reported in the IPANS study represents a “black hole” in recently published surveys.[12] The high prevalence of ICP in India, and Kerala in particular, warrants close examination of putative etiopathogenic factors.
Early series of TCP comprised of patients typically presenting with pain in childhood, diabetes in adolescence and death during prime of life. A significant finding in our study was the delayed age of onset especially during the latter (2007-2013) time period. This trend seems to be associated with the increase in prevalence of ACP and the change in natural history of ICP with later age of presentation and a milder course of illness. Alcoholism over several years is necessary to produce ACP. However, there is no threshold below which the disease does not occur. In most patients, at least 5 years of alcohol intake exceeding 80 g/day tends to instigate the development of chronic pancreatitis. Only 5–15% of alcoholics develop CP suggesting the role of genetics or associated factors. Proposed cofactors include high-fat, high-protein diet, relative deficiency of antioxidants and/or trace elements, and smoking. However, the definite etiopathogenesis of TCP remains unresolved. A recent study[13] suggests the interaction of multiple genetic and environmental factors. Oxidative stress and antioxidant depletion appears to be a common pathogenetic mechanism in chronic tissue inflammation and injury. Micronutrient deficiency could impact pancreatic function as some of these appear to be vital though are poorly characterized for pancreatic function. Alternatively, micronutrient deficiency could be implicated in production of oxidative stress which is known to occur in CP.[14]
Our data suggest an emerging shift in CP etiology. Previous studies with predominant non-alcoholic ICP patients now appear to be replaced by many ICP patients who consume alcohol albeit in small quantities.[15] The classical tropical pancreatitis is seldom seen now. In the IPANS study, this entity comprised only ~4% of CP patients.[2] A rise in prevalence of smoking has also been noted which is a risk factor for disease progression, development of early calcification and is an independent risk factor for pancreatic cancer.
Besides alcohol and smoking, we are also witnessing increased consumption of fat, high caloric foods, refined sugar, junk food and non-vegetarian food. An alarming rise in metabolic syndrome has been noted across age groups in the general population. High BMI and related metabolic factors are present in the background of a subset of CP patients today. We found obesity (BMI >30) in ~2% of our patients over the latter study period. We have reported this emerging problem previously as well.[16] Lifestyle interventions are likely to be beneficial and may find a place in the management of CP. While prevalence of DM was comparable there was a rise in prevalence of PEI during the latter time period. There was no significant increase in proportion of rare causes of CP. However, autoimmune pancreatitis was first observed during 2007-2013. It is likely that increased awareness and regular screening are likely for higher detection. The high prevalence of ICP needs closer examination of its risk factors and pathogenesis of. ACP appears to be emerging as a dominant etiology of CP and merits better preventive strategies.
References
- Balakrishnan V, Kumar H, Sudhindran S, Unnikrishnan AG, editors. Chronic pancreatitis and pancreatic diabetes in India. Kochi: Indian Pancreatitis Study Group; 2005.
- Balakrishnan V, Unnikrishnan AG, Thomas V, Choudhuri G, Veeraraju P, Singh SP, et al. Chronic pancreatitis. A prospective nationwide study of 1,086 subjects from India. JOP.2008;9:593–600.
- Veena AB, Rajesh G, Varghese J, Sundaram KR, Balakrishnan V.Alcoholic chronic pancreatitis and alcoholic liver cirrhosis: differences in alcohol use habits and patterns in Indian subjects. Pancreas. 2012;41:703–6.
- Balakrishnan V, Nair P, Radhakrishnan L, Narayanan VA. Tropical pancreatitis - a distinct entity, or merely a type of chronic pancreatitis? Indian J Gastroenterol. 2006;25:74–81.
- Geevarghese PJ, Pitchumoni CS, Nair SR. Is protein malnutrition an initiating cause of pancreatic calcification? J Assoc Physicians India. 1969;17:417–9.
- Balaji LN, Tandon RK, Tandon BN, Banks PA. Prevalence and clinical features of chronic pancreatitis in southern India. Int J Pancreatol. 1994;15:29–34.
- Garg PK, Tandon RK. Survey on chronic pancreatitis in the Asia- Pacific region. J Gastroenterol Hepatol. 2004;19:998–1004.
- Frulloni L, Gabbrielli A, Pezzilli R, Zerbi A, Cavestro GM, Marotta F, et al. Chronic pancreatitis: report from a multicenter Italian survey (PanCroInfAISP) on 893 patients. Dig Liver Dis. 2009;41:311–7.
- Yadav D, Whitcomb DC. The role of alcohol and smoking in pancreatitis. Nat Rev Gastroenterol Hepatol. 2010;7:131–45.
- Otsuki M. Chronic pancreatitis in Japan: epidemiology, prognosis, diagnostic criteria, and future problems. J Gastroenterol. 2003;38:315–26.
- Masamune A, Kume K, Shimosegawa T. Sex and age differences in alcoholic pancreatitis in Japan: a multicenter nationwide survey. Pancreas. 2013;42:578–83.
- Pezzilli R. Etiology of chronic pancreatitis: has it changed in the last decade? World J Gastroenterol. 2009;15:4737–40.
- Midha S, Khajuria R, Shastri S, Kabra M, Garg PK. Idiopathic chronic pancreatitis in India: phenotypic characterisation and strong genetic susceptibility due to SPINK1 and CFTR gene mutations. Gut. 2010;59:800–7.
- Rajesh G, Girish BN, Vaidyanathan K, Balakrishnan V. Diet, nutrient deficiency and chronic pancreatitis. Trop Gastroenterol. 2013;34:68–73.
- Rajesh G, Veena AB, Menon S, Balakrishnan V. Clinical profile of early-onset and late-onset idiopathic chronic pancreatitis in South India. Indian J Gastroenterol. 2014;33:231–6.
- Rajesh G, Kumar H, Menon S, Balakrishnan V. Pancreatitis in the setting of the metabolic syndrome. Indian J Gastroenterol. 2012;31:79–82.
|
|
|
 |
|
|