|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
gastroesophageal reflux disease, pregnancy, diet |
|
|
Ramya RS,1 Jayanthi N,1 Alexander PC,2 Vijaya S,3 Jayanthi V2
Sivarajan Maternity Hospital,
Kanyakumari,1
Department of Gastroenterology
and Hepatology,
Stanley Medical College Hospitals,2
and Global Hospitals,3
Chennai, Tamil Nadu,
India
Corresponding Author:
Dr. V Jayanthi
Email: drjayanthi35@yahoo.co.in
DOI:
http://dx.doi.org/10.7869/tg.205
Abstract
Background: Gastroesophageal reflux (GER) symptoms are common in pregnancy. It often manifests for the first time in pregnancy during the first three months and ceases after delivery.
Aim: To study the prevalence of gastroesophageal reflux in each of the three trimesters by follow-up of pregnant women. To examine the association between dietary factors and GER in pregnancy
Methods: This was a prospective hospital-based study. Sixty four pregnant women in their first trimester attending an antenatal clinic were interviewed for symptoms of GER and for dietary details and followed up until term and delivery.
Results: Fifty women (83.4%) experienced either heartburn or regurgitation during pregnancy. GER was commoner in primi-gravida (69.3%) and 50% remained symptomatic until term. Regurgitation was more common than heartburn and was often associated with nausea / vomiting. Women with an antenatal history of GERD had 3.79 times the odds of developing symptoms in the third trimester. There was no difference in weight gain in those with and without GER. Spicy food significantly increased the risk of heartburn and green vegetables were protective.
Conclusions: The incidence of GERD decreased over three trimesters. Weight gain did not increase the prevalence of GERD. Spicy food aggravated while green vegetables protected against GERD.
|
48uep6bbphidvals|629 48uep6bbph|2000F98CTab_Articles|Fulltext Gastroesophageal reflux (GER) is estimated to occur in 30-50%[1-3] of pregnancies, with the incidence approaching 80% in certain population.[4-6] Rarely it represents an exacerbation of preexisting GERD during pregnancy. Not uncommonly, GER manifests in the first three months of gestation and ceases soon after delivery.[7,8]
The origin of GER in pregnancy is multifactorial, but the predominant factor is a decrease in lower esophageal sphincter pressure caused by progesterone. Mechanical factors play a minor role. Serious reflux complications during pregnancy are rare and seldom do these patients need investigation. Our recent cross sectional study found a prevalence of 45.5% GER in pregnancy.[9] There however has been no prospective study from India examining the natural history of symptomatic GER from the first to third trimester in women with different parity. This study was undertaken to elucidate the prevalence of GER in each trimester of pregnancy by prospective follow-up of pregnant women; and to examine the association of dietary factors with GER in pregnancy.
Methods
Sixty-four consecutive pregnant patients attending the antenatal clinic at Sivarajan Maternity Hospital, Kanyakumari, Tamil Nadu were followed up from their first trimester until a year after delivery. Data was collected in a standardized questionnaire, for typical and atypical symptoms of GER and associated factors including diet during each trimester until a year after delivery. The three-day dietary recall method was used for collecting dietary history. All patients were followedup for a minimum of 18 to 21 months from the time of enrollment. The study was completed in November 2010. Selection criteria included pregnant women with typical or atypical GER symptoms. Only those mothers who were available for followup until term and could be contacted for at least a year after delivery were included in the study. Chi square test, trend chi square, and odds ratio were employed for analysis. SPSS v16.0 was used for data analysis.
Results
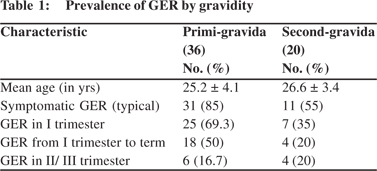
Sixty of the 64 pregnant women fulfilled the selection criteria and were followed-up from first trimester until a year after delivery. 36 (60%) women were primi-gravida, 20 (33%) were second-gravida, 3 (5%) were third-gravida and only one was 5th gravida. Fifty women (83.4%) had symptoms of either heartburn or regurgitation during pregnancy. 42 had typical symptoms and 8 complained of atypical symptoms. The prevalence of GER was significantly higher among the primigravida (85%) than second-gravida (55%) (p<0.05). 25 (69.3%) primi-gravida manifested GER in their first trimester and 18 (50%) continued to have symptoms until term. Of the 7 second-gravida (35%) women with GER, 4 (20%) remained symptomatic until term (p<0.05). Gravidity did not influence the onset of GER in the second or third trimesters (Table 1).
GER and trimester of pregnancy
Heartburn
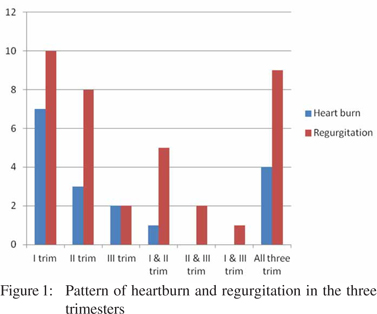
Of the twelve (20%) women who experienced heartburn in the first trimester, six remained symptomatic in their second and two in their third trimesters. Four (6.7%) patients developed heartburn for the first time in the second trimester and one of them continued to be symptomatic until her third trimester. Three women (5%) developed heartburn for the first time in the third trimester. Forty one women experienced no heartburn in any of the trimesters (Figure 1).
Regurgitation
Twenty five (41.7%) women suffered regurgitation in the first trimester, 24 (60%) in the second and 14 (23.3%) in the third. This included nine patients who experienced symptoms in all three trimesters. Figure 1 shows the number of patients who’s regurgitation progressed from one to any of the other two trimesters.
Heartburn and regurgitation
Six women (10%) had both heartburn and regurgitation in the first and second trimester, and in three of these patients the symptoms persisted until the third trimester.
 Trend of nausea and vomiting in GER
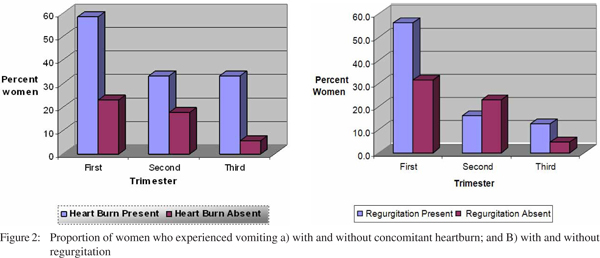
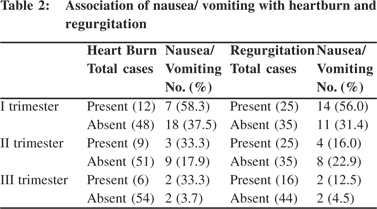
Amongst those with heartburn, 7 of 12 (58.6%) in the first trimester, 3 of 9 (33.3%) and 2 of 6 (33.3%) in second and third trimester respectively experienced nausea and vomiting. Compared to those without heartburn this proportion was higher in all the three trimesters (p<0.05 for first trimester).Of the 25 women with regurgitation in the first and second trimester, 14 (41.7%) and 4 (16%) women, respectively, had in addition nausea and vomiting. In the third trimester, of the 16 with regurgitation, only 2 (12.5%) had nausea and vomiting.
Trend of nausea and vomiting in GER
Amongst those with heartburn, 7 of 12 (58.6%) in the first trimester, 3 of 9 (33.3%) and 2 of 6 (33.3%) in second and third trimester respectively experienced nausea and vomiting. Compared to those without heartburn this proportion was higher in all the three trimesters (p<0.05 for first trimester).Of the 25 women with regurgitation in the first and second trimester, 14 (41.7%) and 4 (16%) women, respectively, had in addition nausea and vomiting. In the third trimester, of the 16 with regurgitation, only 2 (12.5%) had nausea and vomiting.
Although the overall proportion of women experiencing nausea/vomiting decreased from the first trimester through the second and third trimester (41.6% to 20% and 6.7%), the drop was not as rapid in those with GERD compared to those without (Figure 2A and 2B), (Table 2).
 Prepartum GERD and pregnancy
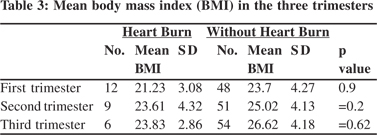
Thirty two (53.3%) women with an antenatal history of GERD were at a greater risk of developing symptoms in the third trimester (odds ratio: 3.79; 95% CI: 1.08-13.24). Three women (4.7%) continued to be symptomatic until one year after delivery (Table 3).
Atypical symptoms
Atypical symptoms during all three trimesters included hoarseness of voice and chest pain in six (10%) and five (8%) patients, respectively. Seven (12%) manifested water brash and 10 also experienced wheeze (14%) in the first trimester.
Prepartum GERD and pregnancy
Thirty two (53.3%) women with an antenatal history of GERD were at a greater risk of developing symptoms in the third trimester (odds ratio: 3.79; 95% CI: 1.08-13.24). Three women (4.7%) continued to be symptomatic until one year after delivery (Table 3).
Atypical symptoms
Atypical symptoms during all three trimesters included hoarseness of voice and chest pain in six (10%) and five (8%) patients, respectively. Seven (12%) manifested water brash and 10 also experienced wheeze (14%) in the first trimester.
Weight gain, BMI in pregnancy and GER
Weight gain (± 2SD) throughout pregnancy was similar in those with or without GER (6.96 ± 1.66 kg vs. 7.67 ± 1.88 kg). Contrary to expectation, BMI was lower in women with GER (2.94 ± 0.91 vs. 3.14 ± 0.83) compared to those without (statistically insignificant).
Diet and GERD in pregnancy
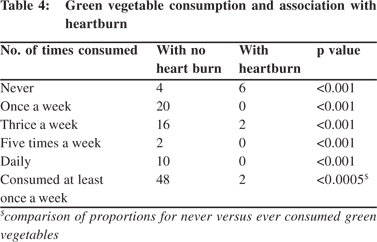
There was significant difference in consumption of coffee/tea, spicy food, green vegetables, fruits, fries and chocolates amongst the pregnant women with GER. 30 women (50%) reported that they never consumed spicy foods, 20 (33%) each said no to coffee/tea or chocolates, 10 (16%) and 8 (13%) women mentioned no to green vegetables and fruits, respectively. Almost all women (90%) used ginger in their diet. Spicy food significantly increased the risk of heartburn in the second trimester (OR: 3.5) when this was taken three or more times a week (p<0.05). Green vegetables protected against heartburn (RR: 15; 95% CI: 3.52-63.89) (Table 4) and higher consumption proportionally decreased the risk of GER (trend chi square <0.001), but had no effect on regurgitation.
 Discussion
Gastroesophageal reflux disease in pregnancy presents a special challenge for the clinician and is not uncommon in pregnancy, occurring in approximately 45% to 80% of pregnant women.[2,3] The reported prevalence of heartburn and/or acid regurgitation among western pregnant women is 48-96% and 62%, respectively.[10,11] Hey et al[12] in a pH study in pregnant women with and without GER found that reflux in pregnancy could be largely asymptomatic, and what is seen in day-to-day practice may just be the tip of the iceberg.
Discussion
Gastroesophageal reflux disease in pregnancy presents a special challenge for the clinician and is not uncommon in pregnancy, occurring in approximately 45% to 80% of pregnant women.[2,3] The reported prevalence of heartburn and/or acid regurgitation among western pregnant women is 48-96% and 62%, respectively.[10,11] Hey et al[12] in a pH study in pregnant women with and without GER found that reflux in pregnancy could be largely asymptomatic, and what is seen in day-to-day practice may just be the tip of the iceberg.
In an earlier study, we had shown that the overall prevalence of GER in pregnancy was 45.5%.[9] In the present study, however, the overall prevalence of GER was higher at 83.4% with the prevalence highest in first trimester and decreasing thereon, similar to that reported by Ho et al[10] from Singapore. Rey et al[4] found the incidence of GER similar across all three trimesters. Weight gain in pregnancy is expected to be associated with higher propensity for GER. Rey et al[4] found that cumulative weight gain during pregnancy was associated with higher risk in the third trimester. In our patients weight gain during pregnancy was similar irrespective of concomitant GER. This may be because there were no women with high BMI during the first trimester in our series.
It is well established that both heartburn and acid reflux can induce nausea and vomiting. The latter symptoms are noted in nearly 80% of pregnancies. Furthermore, they are likely to worsen in the presence of GERD. This was confirmed by Gill et al.[13] The authors for the first time used Pregnancy-Unique Quantification of Emesis (PUQE) score to assess severity of nausea, vomiting and retching over the previous 12 hours,[14] and proved that heartburn and acid reflux were associated with increased severity of nausea and vomiting. Nausea and vomiting was a common association with heartburn and regurgitation in our study as well. However, there were fewer women who reported nausea/vomiting in the first trimester (41.6%) which dropped to 20% and 6.67% in the second and third trimesters, respectively. This is comparable to the observations of Ho et al[10] where nausea alone and in combination with vomiting appeared in 100% women during the first trimester and subsided by the second trimester (85.7%). As a corollary to these observations it is likely that early management of heartburn or acid reflux could improve the severity of nausea and vomiting.
Unlike the report by Benamouzig et al[15] our study found a significant association between consumption of coffee/tea, spicy food, green leafy vegetables, fruits, fries and chocolates and GER in pregnant women. Spicy food significantly increased the risk of heartburn in the second trimester (OR: 3.5) especially when consumed three or more times a week (p<0.05). Green leafy vegetables were protective (RR: 15; 95% CI: 3.52-63.89) on the other hand. Also, higher consumption of vegetables further decreased the risk of GER. Benamouzig et al[15] reported that fat, volume of meal, osmolality, thickening, carbohydrates, fiber, protein, coffee, chocolate, tea, mint, carbonated beverages, spicy food and onions, were unassociated with any unequivocal protective or deleterious effect. In a similar study Song et al[16] found noodles, spicy foods, fatty meals, sweets, breads, carbonated drinks and caffeinated drinks aggravated symptoms of GERD. Similar findings were reported by Dall’Alba et al.[17] However, none of these studies examined the role of fruits and vegetables in their study.
In summary, south Indian pregnant women tend to manifest reflux symptoms at the onset of pregnancy, followed by disappearance as the pregnancy progresses. Our findings are similar to those reported from other south Asian countries. The decrease in symptoms was not influenced by the patient’s gravidity. Green vegetables were protective while spicy foods precipitated GER symptoms. Weight gain during pregnancy had no role in worsening of gastroesophageal reflux symptoms.
References
- Richter JE. Gastroesophageal reflux disease during pregnancy. Gastroenterol Clin North Am. 2003;32:235–61.
- Aro P, Ronkainen J, Storskrubb T, et al. Quality of life in a general adult population with gastro-esophageal reflux symptoms and/or esophagitis: a report from the Kalixanda study. Gastroenterology. 2003;124:A168.
- Shaw MJ, Adlis S, Beebe T, et al. When does heartburn become a disease? Gastroenterology. 1998;114:G1166.
- Rey E, Rodriguez-Artalejo F, Herraiz MA, Sanchez P, Alvarez- Sanchez A, Escudero M, et al. Gastroesophageal reflux symptoms during and after pregnancy: a longitudinal study. Am J Gastroenterol. 2007;102:2395–400.
- Ali RA, Egan LJ. Gastroesophageal reflux disease in pregnancy. Best Pract Res Clin Gastroenterol. 2007;21:793–806.
- Bor S, Kitapcioglu G, Dettmar P, Baxter T. Association of heartburn during pregnancy with the risk of gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2007;5:1035–9.
- Charan M, Katz PO. Gastroesophageal Reflux Disease in Pregnancy. Curr Treat Options Gastroenterol. 2001;4:73–81.
- Anton CR, Anton E, Stanciu C. [Gastroesophageal reflux disease in pregnancy]. Rev Med Chir Soc Med Nat Iasi. 2001;105:43–7.
- Ramu B, Mohan P, Rajasekaran MS, Jayanthi V. Prevalence and risk factors for gastroesophageal reflux in pregnancy. Indian J Gastroenterol. 2011;30:144–7.
- Ho KY, Kang JY, Viegas OA. Symptomatic gastro-oesophageal reflux in pregnancy: a prospective study among Singaporean women. J Gastroenterol Hepatol. 1998;13:1020–6.
- Bainbridge ET, Temple JG, Nicholas SP, Newton JR, Boriah V. Symptomatic gastro-oesophageal reflux in pregnancy. A comparative study of white Europeans and Asians in Birmingham. Br J Clin Pract. 1983;37:53–7.
- Hey VM, Cowley DJ, Ganguli PC, Skinner LD, Ostick DG, Sharp DS. Gastro—oesophageal reflux in late pregnancy. Anaesthesia. 1977;32:372–7.
- Gill SK, Maltepe C, Koren G. The effect of heartburn and acid reflux on the severity of nausea and vomiting of pregnancy. Can J Gastroenterol. 2009;23:270–2.
- Ebrahimi N, Maltepe C, Bournissen FG, Koren G. Nausea and vomiting of pregnancy: using the 24-hour Pregnancy-Unique Quantification of Emesis (PUQE-24) scale. J Obstet Gynaecol Can. 2009;31:803–7.
- Benamouzig R, Airinei G. Diet and reflux. J Clin Gastroenterol. 2007;41:S64–71.
- Song JH, Chung SJ, Lee JH, Kim YH, Chang DK, Son HJ, et al. Relationship between gastroesophageal reflux symptoms and dietary factors in Korea. J Neurogastroenterol Motil. 2011;17:54–60.
- Dall’Alba V, Fornari F, Krahe C, Callegari-Jacques SM, Silva de Barros SG. Heartburn and regurgitation in pregnancy: the effect of fat ingestion. Dig Dis Sci. 2010;55:1610–4.
|
|
|
 |
|
|