48uep6bbphidvals|635
48uep6bbph|2000F98CTab_Articles|Fulltext
Behçet’s disease (BD) is a multisystem immune mediated disorder mostly affecting young individuals. Although the disease can involve virtually any organ in the body, recurrent oro-genital ulcerations with or without skin and eye manifestations is the most common presentation. Gastrointestinal (GI) manifestations are relatively uncommon and are most frequently reported in Japanese patients. Ulceration is the most commonly described gastrointestinal manifestation and has been described in esophagus, stomach and intestines.
Case report
A 38-year-old lady presented to our Dermatology Department in January 2012, with recurrent oral and genital ulcerations of 8 months duration. The ulcers were multiple, small, painful and healed in about 1-2 weeks without leaving any scars. She also had knee joints arthritis as well as recurrent folliculitis. There was no ophthalmic or neurological involvement. Pathergy test was positive. With this constellation of features a diagnosis of BD was made and she was treated with topical steroids and oral colchicine. With symptomatic relief she stopped all medications after three months and was lost to follow-up.
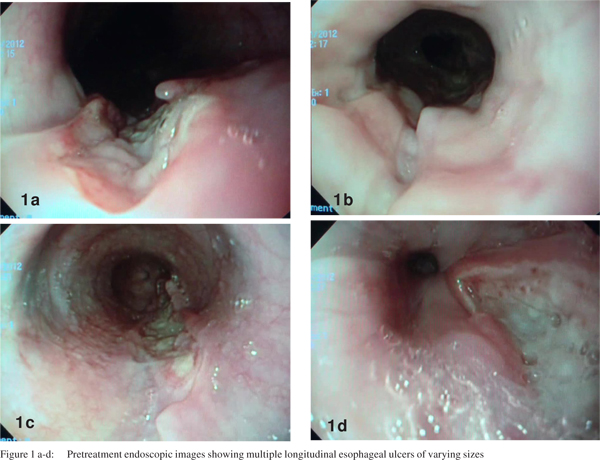
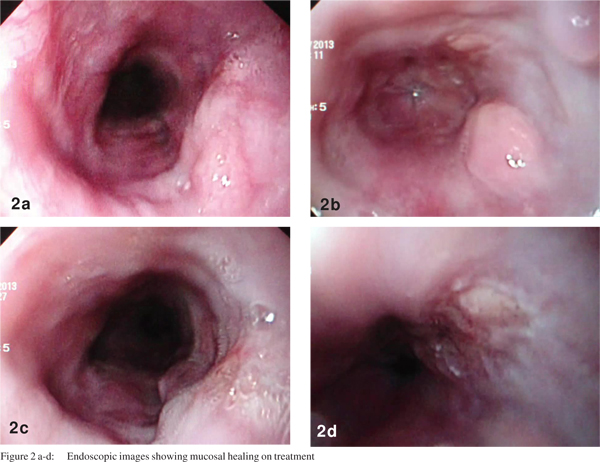
In December 2012 she presented to the Gastroenterology Department with dysphagia and odynophagia for both solids and liquids, of 10 days duration. She had no associated orogenital lesions, abdominal pain or gastrointestinal bleed. There was neither any history of medication intake preceding the onset of symptoms nor any history of food impaction. within normal limits. Routine hemogram and biochemical parameters were normal except for mild anemia. Upper gastrointestinal endoscopy revealed multiple longitudinal ulcerations of varying sizes with yellowish necrotic base in the esophagus (Figures 1a-d) with normal intervening mucosa. Gastric and duodenal mucosa were normal. Biopsies from the lesions revealed squamous epithelium with ulceration and subepithelial infiltration with lymphocytes and scanty neutrophils. There were no cellular atypia, malignant cells or any granulomas. Immuno-histochemical staining for cytomegalovirus and herpes viruses were negative. The patient was treated with sucralfate and mesalamine initially but had no significant improvement. After two weeks she was initiated on oral prednisolone (1mg/kg/day) with which she had symptomatic relief. The dose of steroid was subsequently tapered. Upper gastrointestinal endoscopy after three weeks of steroid therapy revealed excellent mucosal healing (Figures 2a-d).
 Discussion
Behçet’s disease, a chronic multisystem inflammatory disease, was first described by Hulusi Behçet in 1937. BD often affected young males and females along the ancient Silk Route from the Mediterranean region to Eastern Asia.[1,2] Males tend to have more severe disease than females. The exact etiopathogenesis of the syndrome is yet to be elucidated. Pathologically BD is characterized by vasculitis with infiltrating neutrophils and CD4 T cells. Multiple autoantibodies have been demonstrated in patient with BD including those directed against selenium binding protein as well as anti-Saccharomyces cerevisiae antibodies.[3] Genomic studies have demonstrated association with tumor necrosis factor-alpha (TNF-á) 1031C allele and HLAB51 allele.[3]
The hallmark features of this condition include oral and genital ulcerations. Oral ulcerations are most common, recurrent, painful, single or multiple, involving all parts of the oral cavity.[1] Painful genital ulcerations are less common but are more specific than oral ulcers. Cutaneous lesions occur in as high as 80% patients and include pseudofolliculitis, acneform nodules, erythema nodosum and infrequently Sweet’s syndrome, and pyoderma gangrenosum.[1] Ocular involvement occurs in around 50% of patients and includes anterior and posterior uveitis, optic neuritis and rarely retinal vascular occlusions. Arthralgias or arthritis and venous thrombosis occur in 30-50% patients. Rare manifestations include pulmonary artery vasculitis, neuro-Behçet’s disease and epididymitis.[1] BD often has a chronic course with remissions and exacerbations; common manifestations often being selflimited except for ocular attacks which may result in blindness. The severity and frequency of exacerbations tend to decrease over time.
Discussion
Behçet’s disease, a chronic multisystem inflammatory disease, was first described by Hulusi Behçet in 1937. BD often affected young males and females along the ancient Silk Route from the Mediterranean region to Eastern Asia.[1,2] Males tend to have more severe disease than females. The exact etiopathogenesis of the syndrome is yet to be elucidated. Pathologically BD is characterized by vasculitis with infiltrating neutrophils and CD4 T cells. Multiple autoantibodies have been demonstrated in patient with BD including those directed against selenium binding protein as well as anti-Saccharomyces cerevisiae antibodies.[3] Genomic studies have demonstrated association with tumor necrosis factor-alpha (TNF-á) 1031C allele and HLAB51 allele.[3]
The hallmark features of this condition include oral and genital ulcerations. Oral ulcerations are most common, recurrent, painful, single or multiple, involving all parts of the oral cavity.[1] Painful genital ulcerations are less common but are more specific than oral ulcers. Cutaneous lesions occur in as high as 80% patients and include pseudofolliculitis, acneform nodules, erythema nodosum and infrequently Sweet’s syndrome, and pyoderma gangrenosum.[1] Ocular involvement occurs in around 50% of patients and includes anterior and posterior uveitis, optic neuritis and rarely retinal vascular occlusions. Arthralgias or arthritis and venous thrombosis occur in 30-50% patients. Rare manifestations include pulmonary artery vasculitis, neuro-Behçet’s disease and epididymitis.[1] BD often has a chronic course with remissions and exacerbations; common manifestations often being selflimited except for ocular attacks which may result in blindness. The severity and frequency of exacerbations tend to decrease over time.
GI involvement in BD often develops after onset of oral ulcerations.[4] The prevalence of GI involvement varies between different ethnic groups; seen most commonly amongst the Japanese and Koreans (50-60%) and less commonly among patients from Turkey and Israel (0-5%).[5] Ulcerations are the most common GI lesions and may occur anywhere along the gastrointestinal tract; most common site being ileocaecal region. Closely mimicking Crohn’s disease, BD can be associated with abdominal pain, altered bowel habits, bleeding, perforation, fistula formation and colonoscopy may reveal ileocaecal aphthoid ulcers.[1,4,6] Esophageal ulcers are uncommon in BD and since their first description by Brodie and Ochsner in 1973, less than 50 cases have been reported worldwide till date.[7] Esophageal lesions include ulcerations, fistulae, strictures and varices.[4] Esophageal ulcerations can be single or multiple and are often associated with ulcerations elsewhere in the GI tract. Rare gastrointestinal manifestations include portal vein thrombosis and Budd Chiari syndrome.[4]
Diagnosis of the condition is often clinical and the widely accepted criteria for BD were defined by the 1990 International Study Group for BD. Diagnosis requires the presence of recurrent oral ulcerations plus any two of the following criteria (1) recurrent genital ulcerations, (2) eye lesions, (3) skin lesions, and/or (4) positive pathergy test.[1-4] Investigations are often nonspecific and not diagnostic. Treatment options include topical glucocorticoids and colchicine for mucocutaneous disease. Thalidomide has been used as a second-line agent for treatment of oral and genital ulcers. Systemic steroids, cyclosporin, cyclophosphamide, azathioprine, and anti-TNF agents have been tried in severe and refractory cases. Sulfasalazine and systemic corticosteroids remain the mainstay of treatment of GI disease.[1]
Our patient was diagnosed with BD since she met the clinical diagnostic criteria. The background of BD and the lack of an alternate clinical or histological etiology to account for the ulcerations make it highly likely that the lesions were due to BD itself. The successful response to oral steroids also supports the diagnosis.
Conclusion
Esophageal involvement is uncommonly seen in BD. As seen in the remaining gastrointestinal tract, ulceration is the most common esophageal manifestation.
References
- Sakane T, Takeno M, Suzuki N, Inaba G. Behcet’s disease. N Engl J Med. 1999;341:1284–91.
- Ebert EC. Gastrointestinal manifestations of Behcet’s disease. Dig Dis Sci. 2009;54:201–7.
- Krause I, Weinberger A. Behcet’s disease. Curr Opin Rheumatol. 2008;20:82–7.
- Bayraktar Y, Ozaslan E, Van Thiel DH. Gastrointestinal manifestations of Behcet’s disease. J Clin Gastroenterol. 2000;30:144–54.
- Yurdakul S, Tuzuner N, Yurdakul I, Hamuryudan V, Yazici H. Gastrointestinal involvement in Behcet’s syndrome: a controlled study. Ann Rheum Dis. 1996;55:208–10.
- Cheon JH, Han DS, Park JY, Ye BD, Jung SA, Park YS, et al. Development, validation, and responsiveness of a novel disease activity index for intestinal Behcet’s disease. Inflamm Bowel Dis. 2011;17:605–13.
- Yi SW, Cheon JH, Kim JH, Lee SK, Kim TI, Lee YC, et al. The prevalence and clinical characteristics of esophageal involvement in patients with Behcet’s disease: a single center experience in Korea. J Korean Med Sci. 2009;24:52–6.