Pradeep Kakkadasam Ramaswami1, Harshad Vinay Joshi1, Rony Thomas1, Renu Thomas2, Charles Panackel1, Sunil K Mathai1
Departments of Gastroenterology1 and Pathology,2
Medical Trust Hospital, Ernakulam, Kerala, India
Corresponding Author:
Dr. Pradeep Kakkadasam Ramaswami
Email: drkrpradeep@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.214
48uep6bbphidvals|638 48uep6bbph|2000F98CTab_Articles|Fulltext IPSID, traditionally termed Mediterranean lymphoma or Alpha Heavy Chain Disease, is a B cell neoplasm that arises in small intestinal mucosa-associated lymphoid tissue (MALT). It is characterized by the production of an unusual IgA heavy chain protein, called á heavy chain, which is secreted by plasma cells and is detectable in various body fluids. Patients may present in the second and third decades of life with chronic diarrhea, malabsorption, weight loss and abdominal pain. Clubbing of the fingers and nutritional deficiencies are characteristic, and palpable abdominal masses may be present.[1,2] The most frequently affected sites are the duodenum and upper jejunum, but the pathology is diffuse with a mucosal cellular infiltrate involving large segments of the intestine and sometimes the entire length.[1]
Case report
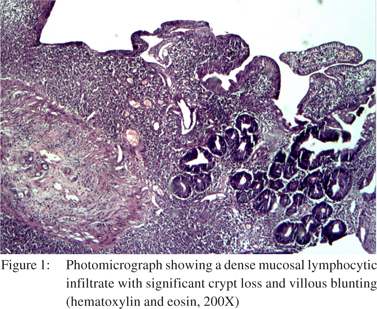
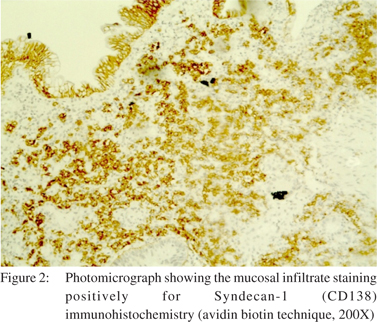
A 47-year-old male presented with a one week history of upper abdominal pain, vomiting and fever. He had lost 6 kilograms of weight over the previous one month. He did not have any comorbid illnesses. Neither did he smoke nor did he consume alcohol. Physical examination revealed that he was febrile, had tachycardia and clubbing. Abdominal examination revealed epigastric tenderness. Haemoglobin was 10.5 gm% and serum albumin was 3 gm%. An erect abdominal X-ray was normal. Contrast enhanced CT scan of the abdomen was also normal. In view of the persistent symptoms an upper GI enteroscopy was performed, which revealed multiple ulcers in the proximal jejunum with mucosal edema. Biopsies from the ulcers showed a cellular mucosal infiltrate with destruction of the crypts and a reduction in crypt density, villi were short and broad (Figure 1). Immunohistochemistry showed cells which were LCA (Leukocyte common antigen) positive, CD3 (T cell marker) negative, CD20 (B cell marker) focally positive, IHC for kappa and lambda light chains was negative, Ki 67 showed low expression, and Syndecan 1 (plasma cell marker) was positive (Figure 2). Based on these findings we made a diagnosis of early stage IPSID. Serum alpha heavy chain levels were not measured. He was started on oral tetracycline and has been on follow-up for more than six months and is asymptomatic.
 Discussion
IPSID accounts for 1.2% of all GI lymphomas in India[3] and 2% of malabsorption syndrome in adults.[4] The main pathologic feature is the presence of dense mucosal “centrocyte-like” infiltrates along with many plasma cells, involving long segments of the small bowel mucosa predominantly the proximal parts. The overlying epithelial cells are usually intact, the crypts are sparse, and the villi are short and broad. In the late stages, the villi are further broadened and may become completely effaced, crypts are fewer, and the immunoproliferation extends deeper. Over time the process evolves into overt lymphoma. Progression to higher grade large-cell lymphoplasmacytic and immunoblastic lymphoma is characterized by increased plasmacytic atypia with the formation of aggregates and later sheets of dystrophic plasma cells and immunoblasts invading into the submucosa and the muscularis propria.[5] Vaiphei et al evaluated various immunohistochemical markers for the diagnosis and prognosis of IPSID. They highlighted the utility of Syndecan 1 for the identification of early stage IPSID.[6]
References
Discussion
IPSID accounts for 1.2% of all GI lymphomas in India[3] and 2% of malabsorption syndrome in adults.[4] The main pathologic feature is the presence of dense mucosal “centrocyte-like” infiltrates along with many plasma cells, involving long segments of the small bowel mucosa predominantly the proximal parts. The overlying epithelial cells are usually intact, the crypts are sparse, and the villi are short and broad. In the late stages, the villi are further broadened and may become completely effaced, crypts are fewer, and the immunoproliferation extends deeper. Over time the process evolves into overt lymphoma. Progression to higher grade large-cell lymphoplasmacytic and immunoblastic lymphoma is characterized by increased plasmacytic atypia with the formation of aggregates and later sheets of dystrophic plasma cells and immunoblasts invading into the submucosa and the muscularis propria.[5] Vaiphei et al evaluated various immunohistochemical markers for the diagnosis and prognosis of IPSID. They highlighted the utility of Syndecan 1 for the identification of early stage IPSID.[6]
References
- Salem PA, Estephan FF. Immunoproliferative small intestinal disease: current concepts. Cancer J. 2005;11:374–82.
- Lecuit M, Abachin E, Martin A, Poyart C, Pochart P, Suarez F, et al. Immunoproliferative small intestinal disease associated with Campylobacter jejuni. N Engl J Med. 2004;350:239–48.
- Arora N, Manipadam MT, Pulimood A, Ramakrishna BS, Chacko A, Kurian SS, et al. Gastrointestinal lymphomas: pattern of distribution and histological subtypes: 10 years experience in a tertiary centre in South India. Indian J Pathol Microbiol. 2011;54:712–9.
- Ghoshal UC, Mehrotra M, Kumar S, Ghoshal U, Krishnani N, Misra A, et al. Spectrum of malabsorption syndrome among adults & factors differentiating celiac disease & tropical malabsorption. Indian J Med Res. 2012;136:451–9.
- Al-Saleem T, Al-Mondhiry H. Immunoproliferative small intestinal disease (IPSID): a model for mature B-cell neoplasms. Blood. 2005;105:2274–80.
- Vaiphei K, Kumari N, Sinha SK, Dutta U, Nagi B, Joshi K, et al. Roles of syndecan-1, bcl6 and p53 in diagnosis and prognostication of immunoproliferative small intestinal disease. World J Gastroenterol. 2006;12:3602–8.
|