|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
domperidone vidal domperidone eureka
Department of Radiology, Christian Medical College,
Vellore, Tamil Nadu – 632004, India
Corresponding Author:
Dr. Anuradha Chandramohan
Email: anuradhachandramohan@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.212
48uep6bbphidvals|636 48uep6bbph|2000F98CTab_Articles|Fulltext Accessory hepatic lobes are under-reported as they rarely cause clinical symptoms. They are often detected due to related complication such as torsion around its pedicle or incidentally as mass abdomen. We report a rare case of pedunculated accessory hepatic lobe in a young female patient causing extrahepatic portal venous obstruction and portal biliopathy. To the best of our knowledge there is only one previous report of a similar case in the literature.[1]
 Case report
A 25-year-old lady, 10 months post-partum, presented with history of increased bleeding per vagina for 6 months duration. She gave no history of abdominal pain, vomiting or jaundice. On examination she was hemodynamically stable and had a non-tender, firm, large mass in the right hypochondrium. No pelvic mass was palpable. Her initial blood investigations including hemoglobin, liver function test and serum creatinine were normal. Plain radiograph of the chest was normal. Per speculum examination showed no ulceration or visible varices. Pap smear showed heavily bloodstained cervical smears, negative for malignant cells. Transvaginal sonography was normal.
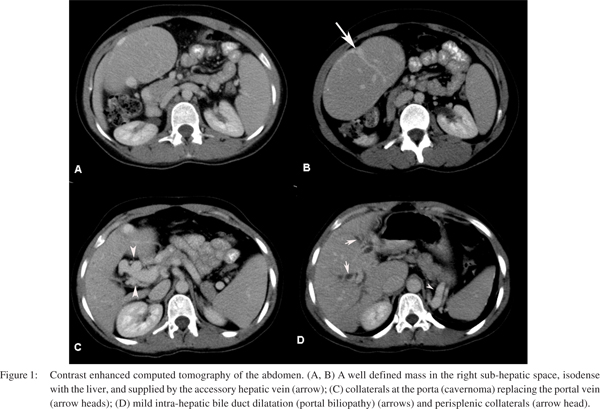
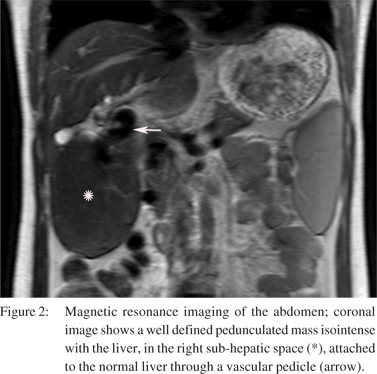
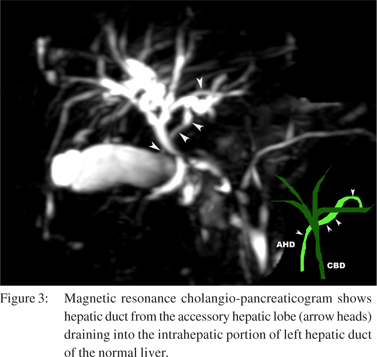
Contrast enhanced computed tomography (CECT) of the abdomen, magnetic resonance imaging (MRI) of the abdomen and magnetic resonance cholangiopancreaticography (MRCP) were done to further evaluate the abdominal mass. CT showed a well defined intra-peritoneal mass in the right upper outer quadrant with smooth margins, isodense with the liver, located in the right sub-hepatic space with a vascular pedicle connecting the mass to the left lobe of liver. The vascular pedicle contained left branch of portal vein, left hepatic artery and accessory hepatic vein. MRI showed similar findings (Figures 1A, 1B and 2). MRCP showed an anomalous hepatic duct extending from the mass and draining into the left hepatic duct. These imaging features are in keeping with the accessory hepatic lobe (Figure 3). The accessory hepatic lobe was causing extrinsic compression and occlusion of the main portal vein at the porta with cavernous transformation of the portal vein. There was mild central intra-hepatic bile duct dilatation (portal biliopathy). There were numerous perisplenic, perigastric collaterals and mild splenomegaly (Figures 1C and 1D). There were no changes characteristic of chronic liver disease and there was no ascites. There were dilated, tortuous vessels in the pelvis surrounding the uterus. Thus a diagnosis of accessory hepatic lobe causing portal vein obstruction and extra-hepatic portal hypertension was made. Patient’s bleeding per vagina settled with symptomatic treatment. Since she did not have any other symptoms directly related to portal hypertension or the accessory hepatic lobe, she was kept on follow-up.
Case report
A 25-year-old lady, 10 months post-partum, presented with history of increased bleeding per vagina for 6 months duration. She gave no history of abdominal pain, vomiting or jaundice. On examination she was hemodynamically stable and had a non-tender, firm, large mass in the right hypochondrium. No pelvic mass was palpable. Her initial blood investigations including hemoglobin, liver function test and serum creatinine were normal. Plain radiograph of the chest was normal. Per speculum examination showed no ulceration or visible varices. Pap smear showed heavily bloodstained cervical smears, negative for malignant cells. Transvaginal sonography was normal.
Contrast enhanced computed tomography (CECT) of the abdomen, magnetic resonance imaging (MRI) of the abdomen and magnetic resonance cholangiopancreaticography (MRCP) were done to further evaluate the abdominal mass. CT showed a well defined intra-peritoneal mass in the right upper outer quadrant with smooth margins, isodense with the liver, located in the right sub-hepatic space with a vascular pedicle connecting the mass to the left lobe of liver. The vascular pedicle contained left branch of portal vein, left hepatic artery and accessory hepatic vein. MRI showed similar findings (Figures 1A, 1B and 2). MRCP showed an anomalous hepatic duct extending from the mass and draining into the left hepatic duct. These imaging features are in keeping with the accessory hepatic lobe (Figure 3). The accessory hepatic lobe was causing extrinsic compression and occlusion of the main portal vein at the porta with cavernous transformation of the portal vein. There was mild central intra-hepatic bile duct dilatation (portal biliopathy). There were numerous perisplenic, perigastric collaterals and mild splenomegaly (Figures 1C and 1D). There were no changes characteristic of chronic liver disease and there was no ascites. There were dilated, tortuous vessels in the pelvis surrounding the uterus. Thus a diagnosis of accessory hepatic lobe causing portal vein obstruction and extra-hepatic portal hypertension was made. Patient’s bleeding per vagina settled with symptomatic treatment. Since she did not have any other symptoms directly related to portal hypertension or the accessory hepatic lobe, she was kept on follow-up.
 Discussion
An accessory hepatic lobe is very rare and reports of this entity are limited to case reports. There may not be any symptoms related to an accessory hepatic lobe or it may present with vague abdominal discomfort or mildly impaired liver enzymes.[2,3] They are often either under-diagnosed or incorrectly reported as non-descript mass abdomen.[3] They arise due to segmentation anomaly of the hepatic bud which originates from a nest of cells situated in the caudal portion of the foregut.[4] Accessory hepatic lobe is often associated with congenital defects of the anterior abdominal wall.[5] Accessory hepatic lobes have been classified as large (>30 g) or small accessory hepatic lobes (<30 g). It can be an ectopic accessory hepatic lobe when there is no connection with the liver. A microscopic accessory lobe is embedded in the gall bladder wall.[3] Three types of accessory hepatic lobe have been described based on their biliary drainage and nature of capsule.[6] In type I, the accessory lobe’s hepatic duct drains into an intra-hepatic bile duct of the normal liver while in type II the accessory duct drains into an extra-hepatic duct of the normal liver. In type III, a common capsule surrounds the accessory lobe and the normal liver and the accessory lobe drains into an extra-hepatic bile duct.[6]
Accessory hepatic lobes are liver attenuation masses which are usually attached to the normal liver through a vascular pedicle. They are predisposed to torsion and result in surgical emergency. The patient presents with acute abdomen, right sided abdominal pain, with or without a palpable mass. Radiological diagnosis with cross-sectional imaging is challenging in a setting of torsion because vascular compromise and necrosis changes the attenuation and enhancement characteristics of the accessory hepatic lobe. In chronic cases of torsion there have been reports of cystic degeneration, congestion and hypertrophy of the accessory hepatic lobe.[2]
Discussion
An accessory hepatic lobe is very rare and reports of this entity are limited to case reports. There may not be any symptoms related to an accessory hepatic lobe or it may present with vague abdominal discomfort or mildly impaired liver enzymes.[2,3] They are often either under-diagnosed or incorrectly reported as non-descript mass abdomen.[3] They arise due to segmentation anomaly of the hepatic bud which originates from a nest of cells situated in the caudal portion of the foregut.[4] Accessory hepatic lobe is often associated with congenital defects of the anterior abdominal wall.[5] Accessory hepatic lobes have been classified as large (>30 g) or small accessory hepatic lobes (<30 g). It can be an ectopic accessory hepatic lobe when there is no connection with the liver. A microscopic accessory lobe is embedded in the gall bladder wall.[3] Three types of accessory hepatic lobe have been described based on their biliary drainage and nature of capsule.[6] In type I, the accessory lobe’s hepatic duct drains into an intra-hepatic bile duct of the normal liver while in type II the accessory duct drains into an extra-hepatic duct of the normal liver. In type III, a common capsule surrounds the accessory lobe and the normal liver and the accessory lobe drains into an extra-hepatic bile duct.[6]
Accessory hepatic lobes are liver attenuation masses which are usually attached to the normal liver through a vascular pedicle. They are predisposed to torsion and result in surgical emergency. The patient presents with acute abdomen, right sided abdominal pain, with or without a palpable mass. Radiological diagnosis with cross-sectional imaging is challenging in a setting of torsion because vascular compromise and necrosis changes the attenuation and enhancement characteristics of the accessory hepatic lobe. In chronic cases of torsion there have been reports of cystic degeneration, congestion and hypertrophy of the accessory hepatic lobe.[2]
Most of these cases are thus diagnosed at the time of operation. Pre-operative evaluation with multi-slice CECT, multi-planar reconstruction and maximum intensity projection is very useful in determining the origin of the mass and also for reviewing the vascular anatomy prior to surgery. MRCP is useful in demonstrating the biliary anatomy.
There are many causes of extra-hepatic portal vein obstruction. However, accessory hepatic lobe causing mechanical compression of the extra-hepatic portal vein and causing portal cavernoma and portal biliopathy is extremely rare. There is only one report of extra-hepatic portal vein obstruction due to an accessory hepatic lobe in a child1 and this report is the second. To the best of our knowledge this is the first report in English literature of an accessory hepatic lobe causing portal vein obstruction and portal biliopathy in an adult patient. Extra-hepatic portal vein obstruction commonly present with upper gastrointestinal bleed due to varices of the rich porta-systemic anastomosis. Bleeding per vagina due to extra-hepatic portal hypertension is a known but uncommon complication. There are extensive venous plexuses around the uterus and vagina which decompress any increase in venous pressure. They communicate with the vesical and hemorrhoidal plexuses, but they seldom bleed. In the rare event where the plexuses are unable to contain the high venous pressure, there can be torrential vaginal bleeding.[7] Portal biliopathy and cholangiopathy with protein-losing enteropathy are also associated with extra-hepatic portal hypertension.[8] This is triggered by the mechanical compression of the bile ducts by portal cavernoma and secondly by ischemic injury to the bile duct wall leading to pericholedochal inflammation and fibrosis.[8,9] Our patient experienced increased bleeding per vagina which we thought to be either dysfunctional uterine bleeding or portal hypertension, since no other cause was found. The patient improved with treatment for dysfunctional uterine bleeding and she did not have any other symptoms directly related to portal hypertension. She was kept on close follow-up. Adult patients with chronic extra-hepatic portal vein obstruction can remain asymptomatic up till four to twelve years after the obstruction and commonly present with variceal bleeds.[10] Although there is imaging evidence of portal biliopathy in more than 80% patients with extra-hepatic portal vein obstruction, only a minority (5%) develop symptoms.[11]
Our patient did not have any symptoms related to portal biliopathy. In conclusion, accessory hepatic lobe is a rare cause of portal vein obstruction. Contrast enhanced CT, MRI and MRCP can help establish the diagnosis.
References
- Matley PJ, Rode H, Cywes S. Portal vein obstruction by ectopic liver tissue. J Pediatr Surg. 1989;24:1163–4.
- Jambhekar K, Pandey T, Kaushik C, Shah HR. Intermittent torsion of accessory hepatic lobe: An unusual cause of recurrent right upper quadrant pain. Indian J Radiol Imaging. 2010;20:135–7.
- Massaro M, Valencia MP, Guzman M, Mejia J. Accessory hepatic lobe mimicking an intra-abdominal tumor. J Comput Assist Tomogr. 2007;31:572–3.
- Rendina EA, Venuta F, Pescarmona EO, Martelli M, Ricci C. Intrathoracic lobe of the liver. Case report and review of the literature. Eur J Cardiothorac Surg. 1989;3:75–8.
- Elmasalme F, Aljudaibi A, Matbouly S, Hejazi N, Zuberi MS. Torsion of an accessory lobe of the liver in an infant. J Pediatr Surg. 1995;30:1348–50.
- Goor DA, Ebert PA. Anomalies of the biliary tree. Report of a repair of an accessory bile duct and review of the literature. Arch Surg. 1972;104:302–9.
- McHugh PP, Jeon H, Gedaly R, Johnston TD, Depriest PD, Ranjan D. Vaginal varices with massive hemorrhage in a patient with nonalcoholic steatohepatitis and portal hypertension: Successful treatment with liver transplantation. Liver Transpl. 2008;14:1538–40.
- Gauthier F. Recent concepts regarding extra-hepatic portal hypertension. Semin Pediatr Surg. 2005;14:216–25.
- Besa C, Cruz JP, Huete A, Cruz F. Portal biliopathy: a multitechnique imaging approach. Abdom Imaging. 2012;37:83–90.
- Sarin SK, Agarwal SR. Extrahepatic portal vein obstruction. Semin Liver Dis. 2002;22:43–58.
- Sarin SK, Sollano JD, Chawla YK, Amarapurkar D, Hamid S, Hashizume M, et al. Consensus on extra-hepatic portal vein obstruction. Liver Int. 2006;26:512–9.
|
|
|
 |
|
|