|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Sunil Taneja1, Manavwadhawan1, Subash Gupta2, Neeravgoyal2, Karisangal Vasudev Ramaswamy2, Abhideep Chaudhary2
Departments of Gastroenterology and Hepatology,1 and
Surgical Gastroenterology and Liver Transplantation,2
Centre for Liver and Biliary Surgery,
Indraprastha Apollo Hospital,
New Delhi – 110076, India
Corresponding Author:
Dr. Subash Gupta
Email: guptasubash@hotmail.com
DOI:
http://dx.doi.org/10.7869/tg.192
48uep6bbphidvals|651 48uep6bbph|2000F98CTab_Articles|Fulltext Congenital hepatic fibrosis (CHF) is a rare condition in which portal hypertension may present without overt signs or symptoms of liver disease. Association of CHF with hepatopulmonary syndrome (HPS) has been well described in literature,[1] however there are no reports of CHF with extrahepatic porto-systemic shunt presenting with HPS. We report here such a patient of CHF with extra-hepatic porto-systemic shunt presenting with HPS, who was successfully managed with liver transplantation.
Case report
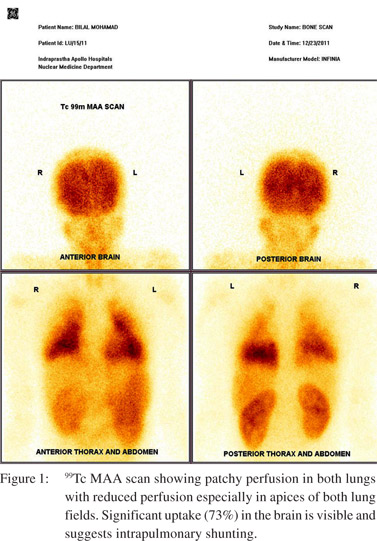
A 14-year-old boy presented to us with two years history of exertional dyspnea and easy fatigability. He also gave history of bluish discoloration of hands and lips for the last three months. There was no history of jaundice, ascites, gastrointestinal bleed or easy bruisability. Clinical examination revealed cyanosis, grade II clubbing and hepatomegaly. There was no jaundice and the remaining systemic examination was normal. Investigations revealed a hemoglobin of 11.8 gm%, a platelet count of 146,000/cu mm and a normal coagulogram. Liver and kidney function tests were normal except for hypoalbuminemia. Arterial blood gas analysis showed an oxygen saturation of 68% and a PaO2 of 37 mmHg. The patient underwent echocardiography to rule out congenital heart disease, which showed normal cardiac chambers, ejection fraction and pulmonary artery systolic pressure. However bubble contrast echocardiography was strongly positive after four beats, suggestive of HPS. Subsequently the patient underwent a macro-aggregate albumin scan which showed a shunt fraction of 73% suggestive of severe HPS (Figure 1).
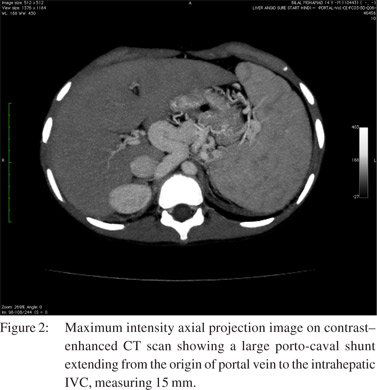
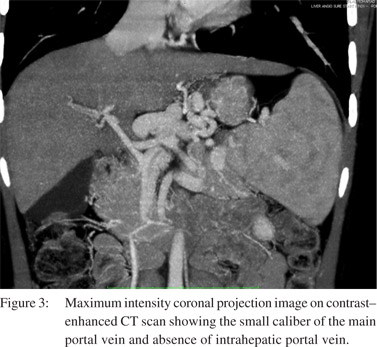
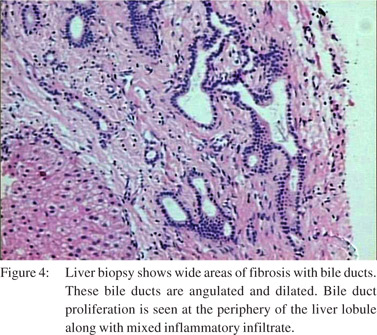
Conventional pulmonary angiography did not reveal any major shunts amenable to embolization. Ultrasound abdomen showed heterogeneous liver parenchyma with a small caliber main portal vein. CT angiography showed heterogeneous attenuation of liver, a small caliber portal vein and a large porto-caval shunt extending from the origin of portal vein to the intrahepatic IVC, measuring 15 mm, and accompanied by mild splenomegaly (Figures 2 & 3). Upper gastrointestinal endoscopy did not reveal any esophageal or gastric varices. Etiological work-up for liver disease including viral and autoimmune markers, iron studies, ceruloplasmin and alpha-1-antitrypsin were all found normal. Thus a liver biopsy was done which revealed features of congenital hepatic fibrosis (Figure 4). The child was evaluated for liver transplantation and the mother became the prospective donor. A standard right lobe graft liver transplantation was performed and the grafted right portal vein was anastomosed with the main portal vein of the recipient along with ligation of the major shunt. The patient needed prolonged postoperative ventilatory support and gradual improvement in oxygenation with PaO2 rising from 37 to 60 mmHg was observed by the end of two weeks. The patient was discharged on domiciliary oxygen therapy for four weeks. At follow-up after five months, the child is maintaining normal oxygenation at ambient oxygen levels and is back to his regular activities.
 Discussion
There are very few reports on the association of congenital hepatic fibrosis with hepatopulmonary syndrome and extrahepatic porto-systemic shunts. Currently liver transplantation is the only successful treatment for HPS, since no effective medical therapy is available.[2] However, postoperative mortality is high and resolution of arterial hypoxemia is often delayed in patients with severe HPS.[3] These patients usually have a longer hospital stay and may take months to recover from hypoxemia.[4]
The strongest predictors of death include a preoperative partial pressure of oxygen of 50 mmHg or less and a lung scan with brain uptake of 20% or more.[5] Our patient had a favorable outcome despite suffering from severe HPS and a significant brain uptake of 73%. Such association of CHF with extra- hepatic porto-systemic shunt and HPS precludes shunt ligation alone as a therapeutic option. Liver transplantation itself is technically demanding given the small caliber of the portal vein making portal vein anastomosis difficult. In our patient the anastomosis was successful and a good inflow was obtained after shunt ligation. The patient had an uneventful surgery but required domiciliary oxygen therapy for one month before complete recovery.
References
Discussion
There are very few reports on the association of congenital hepatic fibrosis with hepatopulmonary syndrome and extrahepatic porto-systemic shunts. Currently liver transplantation is the only successful treatment for HPS, since no effective medical therapy is available.[2] However, postoperative mortality is high and resolution of arterial hypoxemia is often delayed in patients with severe HPS.[3] These patients usually have a longer hospital stay and may take months to recover from hypoxemia.[4]
The strongest predictors of death include a preoperative partial pressure of oxygen of 50 mmHg or less and a lung scan with brain uptake of 20% or more.[5] Our patient had a favorable outcome despite suffering from severe HPS and a significant brain uptake of 73%. Such association of CHF with extra- hepatic porto-systemic shunt and HPS precludes shunt ligation alone as a therapeutic option. Liver transplantation itself is technically demanding given the small caliber of the portal vein making portal vein anastomosis difficult. In our patient the anastomosis was successful and a good inflow was obtained after shunt ligation. The patient had an uneventful surgery but required domiciliary oxygen therapy for one month before complete recovery.
References
- Nagral A, Nabi F, Humar A, Nagral S, Doctor N, Khubchandani SR, et al. Reversal of severe hepato-pulmonary syndrome in congenital hepatic fibrosis after living-related liver transplantation. Indian J Gastroenterol. 2007;26:88–9.
- Rodriguez-Roisin R, Krowka MJ. Is severe arterial hypoxaemia due to hepatic disease an indication for liver transplantation? A new therapeutic approach. Eur Respir J. 1994;7:839–42.
- Taille C, Cadranel J, Bellocq A, Thabut G, Soubrane O, Durand F, et al. Liver transplantation for hepatopulmonary syndrome: a ten-year experience in Paris, France. Transplantation. 2003;75:1482–9; discussion 46–7.
- Philit F, Wiesendanger T, Gille D, Boillot O, Cordier JF. Late resolution of hepatopulmonary syndrome after liver transplantation. Respiration. 1997;64:173–5.
- Arguedas MR, Abrams GA, Krowka MJ, Fallon MB. Prospective evaluation of outcomes and predictors of mortality in patients with hepatopulmonary syndrome undergoing liver transplantation. Hepatology. 2003;37:192–7.
|
|
|
 |
|
|