|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Vivek Mangla1, Joseph George1, Prasenjit Das2, Nihar R Dash1, Sujoy Pal1, Tushar K Chattopadhyay3
Department of Gastrointestinal Surgery1 and Pathology2,
All India Institute of Medical Sciences, and
Department of Hepato-Pancreato-Biliary Surgery3, Institute of Liver & Biliary Sciences,
New Delhi, India.
Corresponding Author:
Dr Vivek Mangla
Email: mangla.vivek@gmail.com
DOI:
http://dx.doi.org/10.7869/tg.125
48uep6bbphidvals|610 48uep6bbph|2000F98CTab_Articles|Fulltext Cystic lesions of the pancreas are most commonly pseuodcysts, pancreatic abscesses or cystic neoplasms.[1] Isolated pancreatic tuberculosis is uncommon.[2] Tubercular pancreatic abscess is a rare entity and, therefore, not usually considered in the differential diagnosis of a cystic pancreatic lesion. We report a rare case of isolated tubercular pancreatic abscess diagnosed on the basis of a biopsy of the abscess wall.
Case report
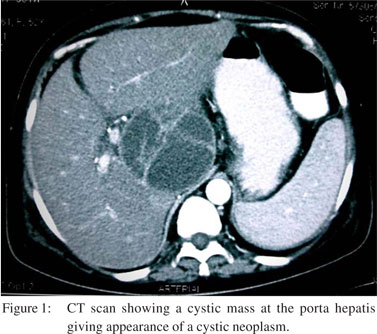
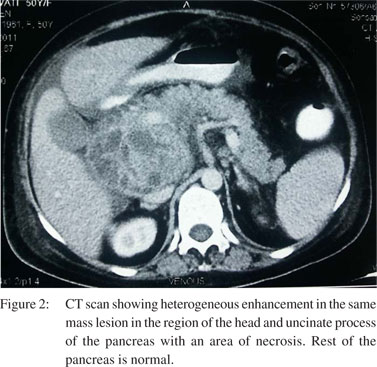
A 50-year-old woman presented with low-grade intermittent fever and upper abdominal discomfort for the past 2 months. She also complained of recurrent episodes of non-bilious vomiting, anorexia and weight loss of 20 kg. She did not give any history of upper abdominal pain during this time. She was malnourished, had mild pallor and generalized oedema. There was no peripheral lymphadenopathy. Examination of the chest did not reveal any abnormality. She had an ill-defined lump in the right hypochondrium and epigastrium. Investigations showed a low haemoglobin level (8 g/dL; reference range: 12– 15 g/dL), normal total leukocyte count (6700 cells/mm3; reference range: 4000–11000 cells/mm3) and raised erythrocyte sedimentation rate (55 mm in 1st hour; reference range: 0–20 mm in 1st hour). She had a normal serum bilirubin level (0.8 mg/ dL; reference range: 0.8–1 mg/dL), raised alkaline phosphatase level (547 IU/L; reference range: 80–240 IU/L) and a low serum albumin level (2.1 g/dL; reference range: 4–5.5 g/dL). Hydatid serology was negative. Chest X-ray was normal. Ultrasound abdomen showed a 13 cm × 7.6 cm heterogeneous collection with thick septae in the region of the head of the pancreas. Contrast-enhanced computed tomography (CECT) scan showed a large, septated cystic lesion replacing the head and uncinate process of the pancreas extending to the porta hepatis (Figure 1). The rest of the pancreas and liver were normal (Figure 2). The small bowel was normal and the mesenteric and retroperitoneal lymph nodes were not enlarged. There was no dilatation of the biliary or pancreatic ducts. With a working diagnosis of an infected cystic lesion of unknown aetiology, intravenous broad-spectrum antibiotics were started following which her symptoms improved but did not resolve. Ultrasoundguided diagnostic aspiration of the cystic lesion yielded purulent fluid. Stain for acid-fast bacilli (AFB) was negative. The amylase levels in the fluid were higher than the upper limit of the normal serum amylase levels (250 U/L; reference range: 0–95 U/L). Culture of the fluid was sterile for bacteria. Fluid cytology was non-contributory. Cyst fluid carbohydrate antigen (CA) 19–9 (25 U/mL; reference range: 0–37 U/mL) was not raised.
 In view of persistent symptoms and a doubt in diagnosis, the patient was planned for surgery. At laparotomy, there was 500 mL of straw-coloured fluid in the peritoneal cavity. There were no enlarged mesenteric lymph nodes or small bowel abnormality. There were dense adhesions in the right subhepatic space. Dissection in the subhepatic space revealed a tense cystic lesion in the region of the head of the pancreas.
In view of persistent symptoms and a doubt in diagnosis, the patient was planned for surgery. At laparotomy, there was 500 mL of straw-coloured fluid in the peritoneal cavity. There were no enlarged mesenteric lymph nodes or small bowel abnormality. There were dense adhesions in the right subhepatic space. Dissection in the subhepatic space revealed a tense cystic lesion in the region of the head of the pancreas.
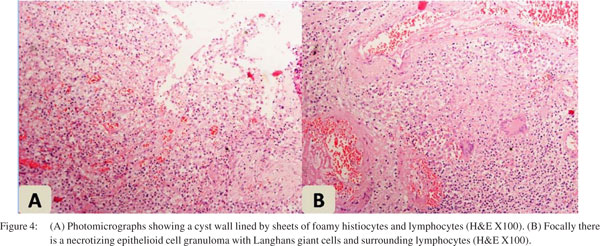
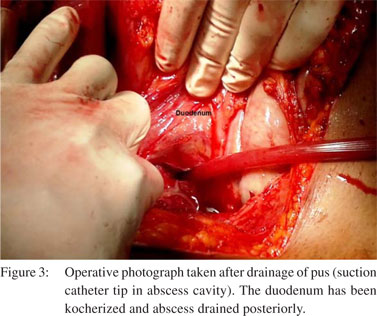
The head of the pancreas could not be identified separately. Needle aspiration of the lesion revealed pus. The abscess cavity was opened and the pus was drained (Figure 3). There were no hydatid membranes or daughter cysts. After thorough lavage, drains were placed in the abscess cavity and a biopsy of the abscess cavity was taken. Pus culture and stain for AFB were again negative. The patient’s symptoms improved after surgery. The amylase levels (950 U/L; reference range for serum amylase: 0–95 U/L) in the drain fluid were more than three times the upper limit of the normal serum amylase levels on postoperative day 3 suggesting a pancreatic fistula. Drainage gradually reduced over a week and the drain was removed. Biopsy of the cyst wall revealed necrotizing epithelioid cell granulomas with Langhans giant cells suggestive of tuberculosis (Figure 4). Stain for AFB was again negative. A diagnosis of tubercular pancreatic abscess was made and the patient was started on antitubercular therapy (ATT). After 4 months of follow-up, the patient made a good recovery and was asymptomatic. ATT is ongoing and a 9-month course is planned.
 Discussion
Pancreatic tuberculosis is infrequent even in areas endemic for tuberculosis. Isolated pancreatic involvement is even more uncommon.[3,4] It usually occurs in young patients who present with insidious onset of abdominal pain, often associated with fever, anorexia and weight loss with or without jaundice. These symptoms are difficult to differentiate from symptoms due to tumours in the head of the pancreas, which occur more commonly. CT scan findings include mass in the head of the pancreas with peripancreatic lymph nodes, which makes differentiation from pancreatic cancer difficult on imaging.[5] Diffuse or segmental, irregular enlargement of the head of the pancreas has also been reported.[6] There are only isolated case reports of tubercular pancreatic abscess,[7–9] where the diagnosis could be made on the basis of a positive AFB stain in the aspirated fluid. However, it is known that AFB may not be seen on staining of aspirated material or even on culture or cytology/histopathology if the bacterial load is low, as was in our case. Moreover, cytological examination of the aspirate in pancreatic tuberculosis is often dominated by acute or chronic inflammatory exudates.
Discussion
Pancreatic tuberculosis is infrequent even in areas endemic for tuberculosis. Isolated pancreatic involvement is even more uncommon.[3,4] It usually occurs in young patients who present with insidious onset of abdominal pain, often associated with fever, anorexia and weight loss with or without jaundice. These symptoms are difficult to differentiate from symptoms due to tumours in the head of the pancreas, which occur more commonly. CT scan findings include mass in the head of the pancreas with peripancreatic lymph nodes, which makes differentiation from pancreatic cancer difficult on imaging.[5] Diffuse or segmental, irregular enlargement of the head of the pancreas has also been reported.[6] There are only isolated case reports of tubercular pancreatic abscess,[7–9] where the diagnosis could be made on the basis of a positive AFB stain in the aspirated fluid. However, it is known that AFB may not be seen on staining of aspirated material or even on culture or cytology/histopathology if the bacterial load is low, as was in our case. Moreover, cytological examination of the aspirate in pancreatic tuberculosis is often dominated by acute or chronic inflammatory exudates.
Acknowledgement
Dr Vivek Mangla acknowledges the Council of Scientific and Industrial Research, New Delhi, India for their support.
References
- Bhansali SK. Abdominal tuberculosis. Experiences with 300 cases. Am J Gastroenterol. 1977;67:324–37.
- Planner AC, Anderson EM, Slater A, Phillips-Hughes J, Bungay HK, Betts M. An evidence-based review for the management of cystic pancreatic lesions. Clin Radiol. 2007;62:930–7.
- Leder RA, Low VH. Tuberculosis of the abdomen. Radiol Clin North Am. 1995;33:691–705.
- Denton T, Hossain J. A radiological study of abdominal tuberculosis in a Saudi population, with special reference to ultrasound and computed tomography. Clin Radiol. 1993;47:409–14.
- Saluja SS, Ray S, Pal S, Kukeraja M, Srivastava DN, Sahni P, et al. Hepatobiliary and pancreatic tuberculosis: a two decade experience. BMC Surg. 2007;7:10.
- Rana SS, Bhasin DK, Rao C, Singh K. Isolated pancreatic tuberculosis mimicking focal pancreatitis and causing segmental portal hypertension. JOP. 2010;11:393–5.
- Fenkel JM, Spodik M, Singu BS, Infantolino A, Deshmukh SP, Loren DE. Tubercular pancreatic abscess presenting as Fever and cystic pancreatic lesion with endoscopic management. Dig Dis Sci. 2010;55:2118–20.
- Lal R, Mishra B, Dogra V, Mandal A. Tubercular pancreatic abscess: a case report. Indian J Med Microbiol. 2003;21:61–2.
- D’Cruz S, Sachdev A, Kaur L, Handa U, Bhalla A, Lehl SS. Fine needle aspiration diagnosis of isolated pancreatic tuberculosis. A case report and review of literature. JOP. 2003;4:158–62.
|
|
|
 |
|
|