48uep6bbphidvals|611
48uep6bbph|2000F98CTab_Articles|Fulltext
Paragangliomas are rare extra-adrenal neoplasms of the neural crest origin.[1,2] The most common extra-adrenal location of these tumours is the retroperitoneum; other locations include the orbit, nose, carotid body, larynx, mediastinum, lungs, oesophagus, stomach, mesentery and urinary bladder.[1,2]
Paragangliomas in the head, neck and mediastinum are usually associated with the parasympathetic system, and are chromaffin-negative and non-functional. Extra-adrenal, retroperitoneal paragangliomas are usually associated with the sympathetic system, are chromaffin-positive, functional and more likely to be malignant.[2] So far only three cases of paraganglioma of the extra-hepatic bile duct have been reported.
Case report
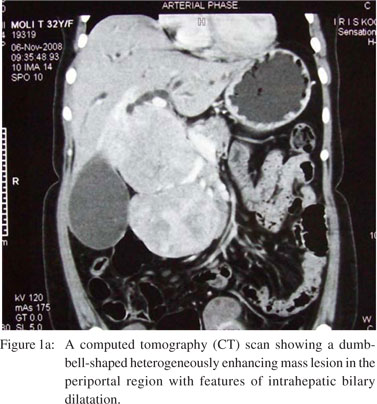
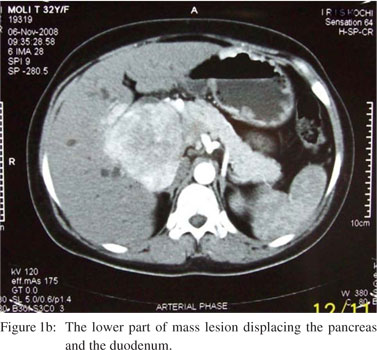
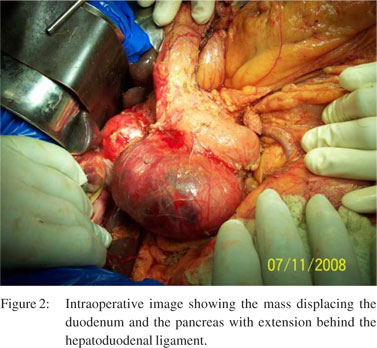
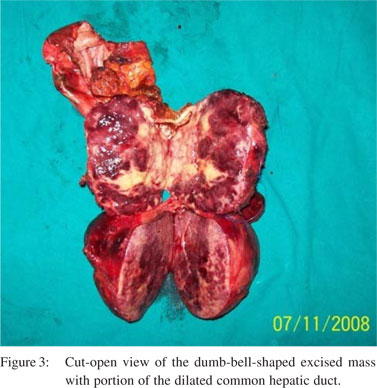
A 32-year-old woman presented with obstructive jaundice and weight loss of 3 weeks’ duration. She had no symptoms of headache, palpitation or family history of any malignancy. Physical examination revealed moderate icterus and a firm globular mass in the right upper quadrant of the abdomen moving with respiration. Serum conjugated bilirubin level was 8.5 mg/dL, aspartate transaminase (AST) level was 125 IU/L, alanine transaminase (ALT) level was 305 IU/L and serum alkaline phosphatase (SAP) level was 438 IU/L. A contrastenhanced computed tomography (CECT) scan of the abdomen revealed an intense heterogeneously enhancing lesion in the periportal region with dilatation of intrahepatic biliary radicals, common hepatic duct, cystic duct and a grossly distended gallbladder (Figure 1a). Common bile duct could not be separately visualized. An extension of the lesion behind the head of the pancreas (Figure 1b) displacing the superior mesenteric vessels and pushing the duodenum anteriorly was noted, suggesting the possibility of a neuroendocrine tumour. The patient was advised laparotomy. At surgery, a 15 cm × 7 cm dumb-bell shaped mass lesion was seen arising from the hepatoduodenal ligament occupying the space between the duodenum and the inferior vena cava (Figure 2). The mass was inseparable from the bile duct, stretching the bile duct and extending from the hilum of the liver up to the superior pole of the right kidney. There was a 0.5 cm-sized nodule in segment V close to the gallbladder. She underwent radical cholecystectomy, choledochectomy and en bloc resection of the mass with a Roux-en-Y hepaticojejunostomy (Figure 3). Histopathology revealed a malignant paraganglioma of the bile duct with metastasis to the liver. Her postoperative period was uneventful and she is currently on chemotherapy.
 Discussion
Common extra-adrenal sites of paragangliomas include the sympathetic ganglia at the neck, in the mediastinum, along the aorta, in the organ of Zuckerkandl, and in the pelvis.[3] So far paragangliomas have been reported in a variety of unusual locations, including the liver, gallbladder, oesophagus, periampullary area, pelvis and urinary bladder. Biliary system paragangliomas are predominantly seen in women and so far only three cases of paraganglioma arising from the hepatic ducts have been reported.[3]
Discussion
Common extra-adrenal sites of paragangliomas include the sympathetic ganglia at the neck, in the mediastinum, along the aorta, in the organ of Zuckerkandl, and in the pelvis.[3] So far paragangliomas have been reported in a variety of unusual locations, including the liver, gallbladder, oesophagus, periampullary area, pelvis and urinary bladder. Biliary system paragangliomas are predominantly seen in women and so far only three cases of paraganglioma arising from the hepatic ducts have been reported.[3]
Paraganglioma has unique pathological features wherein the tumour has well-defined nests of round or polygonal epitheloid cells arranged in a typical Zellballen pattern and surrounded by sustentacular cells in a delicate, fibrovascular stroma.[3,4] The tumour in our patient measured 15 cm × 7 cm and exhibited the above classic histological appearance. The clinical manifestation depends on the functionality of the tumour. Generally, functional tumours are chromaffinpositive and arise mostly from the adrenal medulla or organ of Zuckerhandl and along the peripheral sympathetic system.[2] However, most chromaffin-positive, retroperitoneal tumours appear to be functional as well. Symptoms are related to excess catecholamine production by the tumours, such as norepinephrine, epinephrine and dopamine. Non-functioning tumours are chromaffin-negative and usually arise from the head and neck or mediastinum. As a rule, biliary tract paragangliomas are non-functional.[1,3] All the gallbladder and hepatic duct paragangliomas reported so far were nonfunctional and presented with symptoms referred to biliary tract such as abdominal pain or obstructive jaundice.[3] Our patient did not have symptoms of catecholamine excess and presented only with obstructive jaundice.
Among the available tests, plasma-free metanephrine is considered the most sensitive to confirm excess catecholamine production.[3] Preoperative suspicion of paragangliomas mandates biochemical screening and prevention for perioperative hypertensive crisis. Imaging characteristics are not unique. They are usually large tumours with areas of haemorrhage or necrosis and heterogeneous enhancement after contrast injection.[3]
References
- Caceres M, Mosquera LF, Shih JA, O’Leary JP. Paraganglioma of the bile duct. South Med J. 2001;94:515–18.
- Rajabi M, Rajabi P, Heidarpour M, Raanai M. Paraganglioma of gallbladder: a case report. The Am J Case Rep. 2008;9:220–3.
- Wu TC, Wang JH, Shen SH, Chang CY. Malignant retroperitoneal paraganglioma: a case report and review of literature. Chin J Radiol. 2004;29:365–9.