|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
Ragesh B Tha offshorendassery1, Abdul Khaliq1, Rashi Kochhar1, Kim Vaiphei2, Kartar Singh1, Rakesh Kochhar1
Departments of Gastroenterology1 and Histopathology2,
Postgraduate Institute of Medical Education and Research.
Chandigarh- 160012, India.
Corresponding Author:
Dr. Rakesh Kochhar E
Email: dr_kochhar@hotmail.com
DOI:
http://dx.doi.org/10.7869/tg.136
48uep6bbphidvals|621 48uep6bbph|2000F98CTab_Articles|Fulltext Periampullary tumours are mostly malignant; however, benign lesions usually have a similar presentation. Isolated tuberculosis of the periampullary area is extremely rare, with only one case reported in the literature[1] Tuberculosis of the pancreatoduodenal and periampullary area is also a rare entity with only a few cases reported so far.[2–4] Occurrence of tuberculosis in the periampullary area is rare due to its high gastric acid content, continuous motor activity and relative scarcity of lymphoid follicles.[5] All the cases reported were diagnosed after resection and the treatment was surgery followed by anti-tubercular therapy. We report the first case of isolated periampullary tuberculosis in a patient diagnosed preoperatively by endoscopic biopsy and managed conservatively with 6 months of anti-tubercular therapy.
Case report
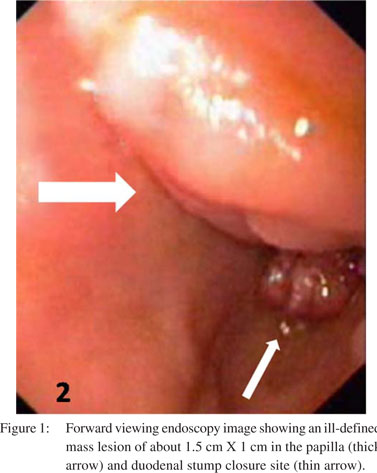
A 56-year-old man presented with a history of jaundice for 4 weeks which was progressively deepening associated with pruritus and clay-coloured stools. He also had dull aching epigastric pain associated with loss of appetite and fever for the same duration. He had a past history of recurrent epigastric pain due to duodenal ulcer for which 15 years ago he underwent distal gastrectomy with Bilroth II anastomosis and truncal vagotomy after which he was asymptomatic. On examination, he was febrile (102 OF) and had deep icterus. He had tense cystic gallbladder palabable. Routine investigations showed mildly elevated total leucocyte count (13,000 cells/cmm) and elevated erythrocyte sedimentation rate (ESR), [65 mm at 1 hour]. Liver function tests showed: total bilirubin level 16 mg/ dL with direct fraction of 12.5 mg/dL, aspartate transaminase 112 U/L, alanine transaminase 126 U/L and alkaline phosphatase 992 U/L. Chest X-ray was normal. Contrast-enhanced computed tomography (CECT) of the abdomen showed distented gallbladder with two calculi, dilated bilobar intrahepatic biliary radicals, dilated common bile duct (CBD) till lower end and dilated pancreatic duct (PD). A diagnosis of extrahepatic biliary obstruction was made and the patient was further investigated.Magnetic resonance cholangiopancreatography (MRCP) showed dilated bilobar intrahepatic biliary radicles, dilated and beaded CBD with distal tapering. The patient underwent sideviewing endoscopy which showed an ill-defined mass lesion of about 1.5×1 cm in the papilla (Figure 1). A provisional diagnosis of periampullary carcinoma was made and biopsy was done. Histopathological examination of biopsy from the periampullary mass showed granulomatous inflammation and acid-fast bacilli (Figure 2). A diagnosis of periampullary tuberculosis was made and the patient was put on antituberculosis treatment, with four drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) for the first 2 months followed by two drugs (isoniazid and rifampicin) for the next 4 months. The patient showed considerable improvement in fever and jaundice after 2 weeks, and complete resolution of symptoms in 6 weeks.
 Discussion
We have described a patient presenting with extrahepatic bilary obstruction and periampullary mass that appeared malignant and the biopsy of which showed features suggestive of tuberculosis. Ampullary and periampullary tumors are rare but have a malignancy rate of more than 90%, most common being adenocarcinoma.[6] Other tumors in the ampullary and periampullary region include ampullary adenomas (villous or tubulovillous), hemangiomas, leiomyomas, leiomyofibromas, lipomas, lymphangiomas and neuroendocrine tumors.[6,7] Non neoplastic causes of ampullary obstruction include choledocholithiasis, chronic pancreatitis, dysfunction of the sphincter of Oddi and the presence of alterations in biliopancreatic drainage (periampullary diverticulum, choledochocele or pancreas divisum), foreign-body deposits, congenital lesions and granulomatous inflammations (such as sarcoidosis or tuberculosis). These periampullary nonneoplastic lesions are rare and often grouped as pseudotumors. Periampullary pseudotumors mimic pancreatic and periampullary carcinoma and often producing obstructive jaundice, bleeding and gastric outlet obstruction.[2] Up to 5% of pancreatectomies performed with the preoperative clinical diagnosis of carcinoma will prove to be non-neoplastic.[8] In India where tuberculosis is endemic periampullary involvement of tuberculosis has been reported previously.[2,3,4] The rarity of tuberculosis in gastroduodenal area is due to gastric acid, continuous motor activity and relative scarcity of lymphoid follicles.[5] The occurrence of tuberculosis in our case could be attributed to lower acid concentration in the afferent loop due to prior gastrojejeunostomy and relative stasis due to truncal vagotomy. The possible routes of infection include direct infection of the mucosa, hematogenous spread, or extension from a neighboring tuberculous lesion.[5] They are often associated with miliary tuberculosis with enlarged peripancreatic lymph nodes and occur more often in immunocompromized patients.[9]
Discussion
We have described a patient presenting with extrahepatic bilary obstruction and periampullary mass that appeared malignant and the biopsy of which showed features suggestive of tuberculosis. Ampullary and periampullary tumors are rare but have a malignancy rate of more than 90%, most common being adenocarcinoma.[6] Other tumors in the ampullary and periampullary region include ampullary adenomas (villous or tubulovillous), hemangiomas, leiomyomas, leiomyofibromas, lipomas, lymphangiomas and neuroendocrine tumors.[6,7] Non neoplastic causes of ampullary obstruction include choledocholithiasis, chronic pancreatitis, dysfunction of the sphincter of Oddi and the presence of alterations in biliopancreatic drainage (periampullary diverticulum, choledochocele or pancreas divisum), foreign-body deposits, congenital lesions and granulomatous inflammations (such as sarcoidosis or tuberculosis). These periampullary nonneoplastic lesions are rare and often grouped as pseudotumors. Periampullary pseudotumors mimic pancreatic and periampullary carcinoma and often producing obstructive jaundice, bleeding and gastric outlet obstruction.[2] Up to 5% of pancreatectomies performed with the preoperative clinical diagnosis of carcinoma will prove to be non-neoplastic.[8] In India where tuberculosis is endemic periampullary involvement of tuberculosis has been reported previously.[2,3,4] The rarity of tuberculosis in gastroduodenal area is due to gastric acid, continuous motor activity and relative scarcity of lymphoid follicles.[5] The occurrence of tuberculosis in our case could be attributed to lower acid concentration in the afferent loop due to prior gastrojejeunostomy and relative stasis due to truncal vagotomy. The possible routes of infection include direct infection of the mucosa, hematogenous spread, or extension from a neighboring tuberculous lesion.[5] They are often associated with miliary tuberculosis with enlarged peripancreatic lymph nodes and occur more often in immunocompromized patients.[9]
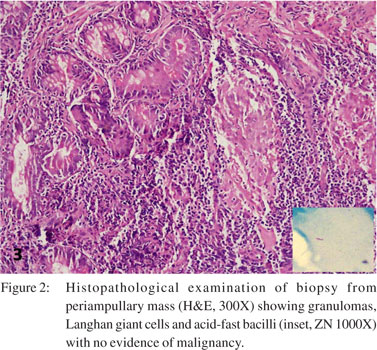 A chest X-ray may show evidence of pulmonary tuberculosis in up to 20% of cases.[2] Acid-fast bacilli are rarely recovered from the biopsy material, although fine-needle aspiration cytology may have a higher yield.[2] Mycobacteria are only rarely cultured from gastric lavage samples.[4] Polymerase chain reaction amplification of mycobacterial DNA may improve the rate of detection.[10] However, false negatives are reported in 40-65% of cases.[11] Preoperative endoscopic biopsy rarely reveals granulomas because these lesions are predominantly submucosal, and endoscopic biopsies often fail to include the submucosa. In a review of 27 patients who underwent endoscopic biopsies for duodenal tuberculosis, granulomas were found in only 7 patients although 20 had images of non-specific duodenitis.[4] Rao et al showed that only 2 of 20 patients with gastroduodenal tuberculosis had positive endoscopic biopsies.[2] All the patients with periampullart tuberculosis described in literature so far underwent surgical resection (two cases underwent triple bypass[1,3] and other two underwent Whipples resection2). In all these cases the diagnosis of tuberculosis was made after the surgery and antitubercular treatment was given post operatively. In our case diagnosis of periampullary tuberculosis could be established before surgery and it could thereby avoid surgery.[2]
Conclusion
Periampullary pseudotumors need to be considered and ruled out in all patients with suspected malignancy in periampullary area. Prompt diagnosis of periampullary tuberculosis can avoid extensive resection and antitubercular treatment alone can lead to complete resolution of symptoms.
References
A chest X-ray may show evidence of pulmonary tuberculosis in up to 20% of cases.[2] Acid-fast bacilli are rarely recovered from the biopsy material, although fine-needle aspiration cytology may have a higher yield.[2] Mycobacteria are only rarely cultured from gastric lavage samples.[4] Polymerase chain reaction amplification of mycobacterial DNA may improve the rate of detection.[10] However, false negatives are reported in 40-65% of cases.[11] Preoperative endoscopic biopsy rarely reveals granulomas because these lesions are predominantly submucosal, and endoscopic biopsies often fail to include the submucosa. In a review of 27 patients who underwent endoscopic biopsies for duodenal tuberculosis, granulomas were found in only 7 patients although 20 had images of non-specific duodenitis.[4] Rao et al showed that only 2 of 20 patients with gastroduodenal tuberculosis had positive endoscopic biopsies.[2] All the patients with periampullart tuberculosis described in literature so far underwent surgical resection (two cases underwent triple bypass[1,3] and other two underwent Whipples resection2). In all these cases the diagnosis of tuberculosis was made after the surgery and antitubercular treatment was given post operatively. In our case diagnosis of periampullary tuberculosis could be established before surgery and it could thereby avoid surgery.[2]
Conclusion
Periampullary pseudotumors need to be considered and ruled out in all patients with suspected malignancy in periampullary area. Prompt diagnosis of periampullary tuberculosis can avoid extensive resection and antitubercular treatment alone can lead to complete resolution of symptoms.
References
- Tewari M, Mishra RR, Kumar V, Kar AG, Shukla HS. Isolated tuberculosis of the ampulla of vater masquerading as periampullary carcinoma: a case report. JOP. 2009;10:184–6.
- Rao YG, Pande GK, Sahni P, Chattopadhyay TK. Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg. 2004;47:364–8.
- Desai CS, Lala M, Joshi A, Abraham P, Desai D, Deshpande RB, et al. Co-existence of peri-ampullary carcinoma with peripancreatic tuberculous lymphadenopathy. JOP. 2004;5:145–7.
- Chaudhary A, Bhan A, Malik N, Dilawari JB, Khanna SK. Choledocho-duodenal fistula due to tuberculosis. Indian J Gastroenterol. 1989;8:293–4.
- Gupta B, Mathew S, Bhalla S. Pyloric obstruction due to gastric tuberculosis: an endoscopic diagnosis. Postgrad Med J. 1990;66:62–5.
|
|
|
 |
|
|