|
|
|
|
 |
 |
| |
 |
|
|
Case Report |
|
|
|
|
|
Keywords :
|
|
|
|
MR Sreevathsa, AH Harsha
Department of General Surgery,
M.S. Ramaiah Medical College and Hospitals,
Mathikere, M.S.R I.T Post,
M.S.R. Nagar, Bangalore,
Karnataka – 560054, India
Corresponding Author:
Dr Harsha AH
Email: harsha_huliyappa@yahoo.com
DOI:
http://dx.doi.org/10.7869/tg.137
48uep6bbphidvals|622 48uep6bbph|2000F98CTab_Articles|Fulltext Abdominal cocooning, otherwise called sclerosing/encapsulating peritonitis (SEP) or chronic encapsulating peritonitis, is a rare surgical disease s of uncertain aetiology, complex in presentation and would need a high index of suspicion for diagnosis.
Case report
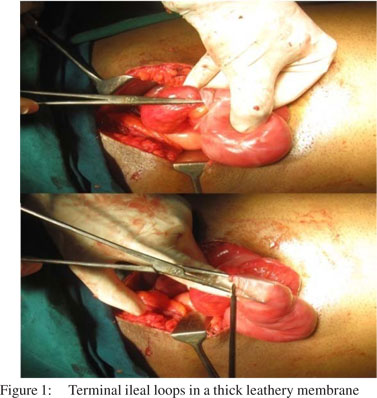
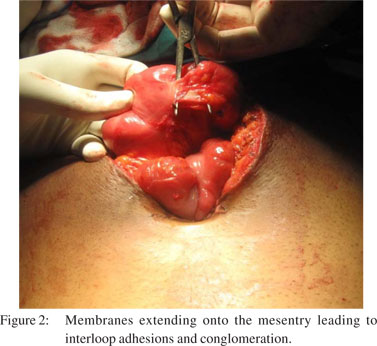
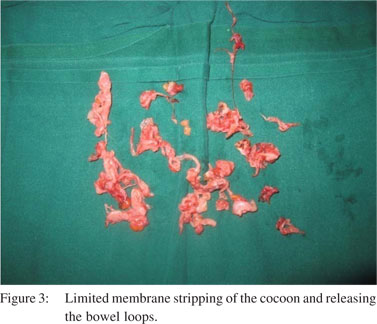
A 43-year-old man from South India presented in May 2011 with 2 weeks’ history of non-bilious vomiting, colicky central abdominal pain which would aggravate on food intake and relieved with passage of flatus. There was a history of similar attacks of vomiting and abdominal pain during the past 1 year. Erect X-ray abdomen showed distended ileal loops. Contrastenhanced CT (CECT) scan of the abdomen showed cocooned ileal loops with posteriorly displaced caecum Diagnostic laparoscopy was performed, which confirmed cocooned terminal ileal loops including ileocaecal junction. A trial release of the enclosing membrane was carried out laparoscopically; but was not effective and hence was converted. Thick membranous adhesions (Figure 1-3) between the terminal ileal loops measuring about 4 feet were releasedThe membrane was sent for histopathological examination, which confirmed fibrocollagenous tissue. Over the next 5 days, the patient returned to normal bowel movements and was discharged on day 7. The patient was followed up for 6 months and has no recurrence of obstruction.
 Two adolescent girls of 13 years (subject A) and 14 years (subject B) of age with similar clinical features presented during May 1993. Both the girls belonged to the Bedouin tribe of Southern Oman called the South Sharqia region, where the staple diet is rice and fish. Both girls presented with pain abdomen in the epigastric and umbilical region which was colicky in nature. Subject A presented with acute intestinal obstruction, though pain was being felt on and off since the past 1 year. Subject B presented with subacute obstruction with pain present for the past 6 months.. In both the cases, there was no ascitis; systemic examination was otherwise normal and the routine investigations were within normal limits. Chest X-ray did not show any evidence of active or quiescent tuberculosis. X-ray abdomen in both the cases showed multiple fluid levels with distended ileal and jejunal loops. Small bowel enema study in Subject B showed the terminal ileum morphologically resembling the colon. Both the patients were subjected to laparotomy.
The specific findings were same in both the patients. The terminal ileal loops up to the ileocaecal junction were found enveloped in a tough leathery envelope which was whitish in colour. This ball of intestine was sitting over the caecum pushing it posteriorly. There were adhesions between the undersurface of the liver and the right colon with a thin membrane extending over the right lobe of the liver. In both the cases, the greater omentum was found stunted in size. Since it was difficult to incise the envelope to release the intestines without injuring them in the process, a limited ileocaecal resection was done. Both the patients had an uneventful recovery. Histopathology was consistent with encapsulating peritonitis. Both the patients were well after 2 years of follow-up.
Discussion
The abdominal cocoon is a rare condition that refers to total or partial encapsulation of the small bowel by a fibrocollagenous membrane leading to acute or chronic bowel obstruction.[1,2] Various synonyms of this rare disease are—”peritonitis chronica fibrosa incapsulata”, and “SEP”.[3] The aetiology and pathogenesis of abdominal cocoon syndrome are obscure. It can be primary/idiopathic or secondary. The secondary type of abdominal cocoon is due to long-term peritoneal dialysis with infections occurring through the infusate, orthotopic liver transplantation, sarcoidosis, tuberculosis, systemic lupus erythematosus (SLE), malignancy and in postoperative cases especially in abdominal wash-out with povidone iodine.[4] The prevalence of abdominal cocoon in patients undergoing continuous ambulatory peritoneal dialysis (CAPD) ranges from 0.5% to 2.8%. More than 50% of patients acquire the disorder within an average of 4 months after termination of CAPD therapy.[5,6] Basu et al., and Lalloo et al., have described that abdominal kochs was a rare causative factor.[7,8] These aetiological factors may predispose patients to peritoneal irritation and inflammation, which finally leads to peritoneal fibrogenesis.[9,10] SEP associated with practolol therapy was first described by Brown et al., and Cook and Foy.[11,12]
Primary abdominal cocoon occurs mainly in young women from the tropical and subtropical zones. Primary or idiopathic abdominal cocoon was first described by Foo et al., in 1978, among adolescent girls and was postulated to be due to retrograde menstruation with superimposed viral infection leading to the subclinical type of primary peritonitis leading to intestinal obstruction.13 But, from India, a 4-year-old girl was reported with abdominal cocoon14 and subsequently a similar premenarcheal case was reported from Saudi Arabia.15 One of our subjects (A) was also premenarchial. We postulate that poor perineal hygiene would have led to subacute bacterial infection when they are consummated after marriage. The retrograde spread of infection on reaching the peritoneum through the fallopian tubes results in encapsulating peritonitis of the ileum. The responsible microorganisms may be endemic and may have predilection for the genital tract.15 Whether a vasculitis in response to consumption of improperly cooked fish could be the inciting factor needs to be investigated. Both the subjects showed adhesions between the undersurface of the liver and the right colon which might also indicate the congenital origin of this membrane. Among girls reported till 1994 with spontaneous encapsulating peritonitis all except three were Asians and only one was an Arab from the Middle East.16 A Medline search for abdominal coccon from 1978 to 2007, yielded 14 male patients with idiopathic aetiology. Tuberculosis can also be a cause of abdominal cocoon syndrome in male patients.17,18 . Most cases of an idiopathic abdominal cocoon present as recurrent intestinal obstruction. The terminal ileal coiled up in a concertina-like fashion and enveloped in a thick leathery membrane with flimsy interloop adhesions are the characteristic operative findings. Gentle handling of the intestine, resection of the entire enveloping membranes and meticulous release of interloop adhesions is the surgical treatment of choice, which has a very low incidence of recurrence.
References
Two adolescent girls of 13 years (subject A) and 14 years (subject B) of age with similar clinical features presented during May 1993. Both the girls belonged to the Bedouin tribe of Southern Oman called the South Sharqia region, where the staple diet is rice and fish. Both girls presented with pain abdomen in the epigastric and umbilical region which was colicky in nature. Subject A presented with acute intestinal obstruction, though pain was being felt on and off since the past 1 year. Subject B presented with subacute obstruction with pain present for the past 6 months.. In both the cases, there was no ascitis; systemic examination was otherwise normal and the routine investigations were within normal limits. Chest X-ray did not show any evidence of active or quiescent tuberculosis. X-ray abdomen in both the cases showed multiple fluid levels with distended ileal and jejunal loops. Small bowel enema study in Subject B showed the terminal ileum morphologically resembling the colon. Both the patients were subjected to laparotomy.
The specific findings were same in both the patients. The terminal ileal loops up to the ileocaecal junction were found enveloped in a tough leathery envelope which was whitish in colour. This ball of intestine was sitting over the caecum pushing it posteriorly. There were adhesions between the undersurface of the liver and the right colon with a thin membrane extending over the right lobe of the liver. In both the cases, the greater omentum was found stunted in size. Since it was difficult to incise the envelope to release the intestines without injuring them in the process, a limited ileocaecal resection was done. Both the patients had an uneventful recovery. Histopathology was consistent with encapsulating peritonitis. Both the patients were well after 2 years of follow-up.
Discussion
The abdominal cocoon is a rare condition that refers to total or partial encapsulation of the small bowel by a fibrocollagenous membrane leading to acute or chronic bowel obstruction.[1,2] Various synonyms of this rare disease are—”peritonitis chronica fibrosa incapsulata”, and “SEP”.[3] The aetiology and pathogenesis of abdominal cocoon syndrome are obscure. It can be primary/idiopathic or secondary. The secondary type of abdominal cocoon is due to long-term peritoneal dialysis with infections occurring through the infusate, orthotopic liver transplantation, sarcoidosis, tuberculosis, systemic lupus erythematosus (SLE), malignancy and in postoperative cases especially in abdominal wash-out with povidone iodine.[4] The prevalence of abdominal cocoon in patients undergoing continuous ambulatory peritoneal dialysis (CAPD) ranges from 0.5% to 2.8%. More than 50% of patients acquire the disorder within an average of 4 months after termination of CAPD therapy.[5,6] Basu et al., and Lalloo et al., have described that abdominal kochs was a rare causative factor.[7,8] These aetiological factors may predispose patients to peritoneal irritation and inflammation, which finally leads to peritoneal fibrogenesis.[9,10] SEP associated with practolol therapy was first described by Brown et al., and Cook and Foy.[11,12]
Primary abdominal cocoon occurs mainly in young women from the tropical and subtropical zones. Primary or idiopathic abdominal cocoon was first described by Foo et al., in 1978, among adolescent girls and was postulated to be due to retrograde menstruation with superimposed viral infection leading to the subclinical type of primary peritonitis leading to intestinal obstruction.13 But, from India, a 4-year-old girl was reported with abdominal cocoon14 and subsequently a similar premenarcheal case was reported from Saudi Arabia.15 One of our subjects (A) was also premenarchial. We postulate that poor perineal hygiene would have led to subacute bacterial infection when they are consummated after marriage. The retrograde spread of infection on reaching the peritoneum through the fallopian tubes results in encapsulating peritonitis of the ileum. The responsible microorganisms may be endemic and may have predilection for the genital tract.15 Whether a vasculitis in response to consumption of improperly cooked fish could be the inciting factor needs to be investigated. Both the subjects showed adhesions between the undersurface of the liver and the right colon which might also indicate the congenital origin of this membrane. Among girls reported till 1994 with spontaneous encapsulating peritonitis all except three were Asians and only one was an Arab from the Middle East.16 A Medline search for abdominal coccon from 1978 to 2007, yielded 14 male patients with idiopathic aetiology. Tuberculosis can also be a cause of abdominal cocoon syndrome in male patients.17,18 . Most cases of an idiopathic abdominal cocoon present as recurrent intestinal obstruction. The terminal ileal coiled up in a concertina-like fashion and enveloped in a thick leathery membrane with flimsy interloop adhesions are the characteristic operative findings. Gentle handling of the intestine, resection of the entire enveloping membranes and meticulous release of interloop adhesions is the surgical treatment of choice, which has a very low incidence of recurrence.
References
- Cambria RP, Shamberger RC. Small bowel obstruction caused by the abdominal cocoon syndrome: possible association with the LeVeen shunt. Surgery. 1984;95:501–3.
- Deeb LS, Mourad FH, El-Zein YR, Uthman SM. Abdominal cocoon in a man: preoperative diagnosis and literature review. J Clin Gastroenterol. 1998:26:148–50.
- Owtschinnikow PJ. Peritonitis chronic fibrosa incapsulata. Arch Klin Chir. 1907;83:623–4.
- Keating JP, Neill M, Hill GL. Sclerosing encapsulating peritonitis after intraperitoneal use of povidone iodine. Aust N Z J Surg. 1997;67:742–4.
- Kawanishi H, Kawaguchi Y, Fukui H, Hara S, Imada A, Kubo H, et al. Encapsulating peritoneal sclerosis in Japan: a prospective, controlled, multicenter study. Am J Kidney Dis. 2004;44:729–37.
- Chin AI, Yeun JY. Encapsulating peritoneal sclerosis: an unpredictable and devastating complication of peritoneal dialysis. Am J Kidney Dis. 2006;47:697–712.
- Basu A, Sukumar R, Sistla SC, Jagdish S. “Idiopathic” abdominal coccon. Surgery. 2007;141:277–8.
- Lalloo S, Krishna D, Maharajh J. Case report: abdominal cocoon associated with tuberculous pelvic inflammatory disease. Br J Radiol. 2002;75:174–6.
- Hasan MFM, Muhsin OMA, Abassi AA, Youssufani R. Abdominal cocoon: a report of three cases. The Middle East Journal of Emergency Medicine. 2007;7(2) Available from:http://www.hmc.org.qa/mejem/sept2007/ Edited/ case2.htm.
- Hosein HH, Quane LK, Cohen AJ. Abdominal cocoon. Applied Radiology Online. 2003;32.
- Brown P, Baddeley H, Read AE, Davies JD, McGarry J. Sclerosing peritonitis, an unusual reaction to a beta adrenergic blocking drug (practolol). Lancet. 1974;2:1477–81.
- Cook AI, Foy P. Sclerosing peritonitis and practolol therapy. Ann R Coll Surg Eng. 1976;58:473–5.
- Foo TK, Ng KC, Rauff A, Foong WC, Sinniah R. Unusual small intestine obstruction in adolescent girls: the abdominal cocoon. Br J Surg. 1978;65:427–30.
- Rao PL, Mitra SK, Pathak IC. ‘Abdominal cocoon’—a cause of intestinal obstruction in a 4-years old girl. Indian Pediatr. 1979;16:1047–8.
- Sieck JO, Coergill R, Larkworthy W. Peritoneal encapsulation and abdominal cocoon. Case reports and a review of the literature. Gastroenterology. 1983;84:1597–1601.
- Yip FW, Lee SH. The abdominal cocoon. Aust N Z J Surg. 1992;62:638–42.
- Pillai JR, Kumar SN, Praneena. Idiopathic abdominal cocoon. Ind J Radiol Imag. 2006;16:483–5.
- Serafimidis C, Katsarolis I, Vernadakis S, Rallis G, Giannopoulos G, Legakis N, et al. Idiopathic sclerosing encapsulating peritonitis (or abdominal cocoon), BMC Surgery. 2006;6:3.
|
|
|
 |
|
|