48uep6bbphidvals|443
48uep6bbph|2000F98CTab_Articles|Fulltext
Cysts of the mesentery are among surgical rarities.[1] The clinical
presentation is not characteristic and in addition, the
preoperative imaging although suggestive is not diagnostic.
In most cases, the diagnosis is confirmed after surgical
exploration and removal of the cyst. We report our experience
in managing 2 patients with these cysts.
Case 1
A 59 year old man presented with abdominal pain of 5 months
duration. The pain was of moderate intensity, localized to the
epigastric region. He had no other complaints and his physical
examination was unremarkable. His biochemical parameters
including serum amylase and lipase were within normal range.
He was evaluated with an ultrasound and subsequently a CT
scan of the abdomen which revealed a hypodense lesion of
fluid attenuation in the left upper abdomen, anterior to the left
kidney, close to the duodenojejunal flexure, separate from the
tail of the pancreas. With a provisional diagnosis of a mesenteric
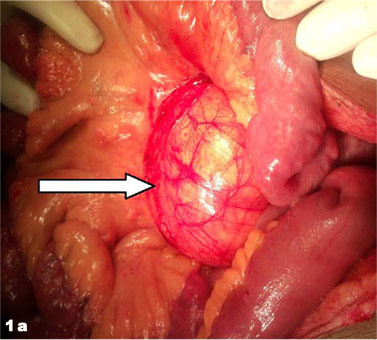
cyst, the patient was planned for surgery. On surgical
exploration, a 10cm × 10cm cyst was seen arising from the
mesentery of proximal jejunum (Figure 1a). Few dilated
lymphatic channels could be seen entering into the cyst. The
cyst was enucleated (Figure 1b) from the mesentery. The cyst
contained milky white fluid (Figure 1c) consistent with a
chylolymphatic cyst. The diagnosis was confirmed on
histopathology which revealed a cyst wall with lymphoid
aggregates. After 9 months of follow-up, the patient is doing
well and is symptom-free.
Case II
A 35 year old man presented with complaints of abdominal
distension and abdominal pain of 9 months duration. The pain
was localized to the epigastrium and was of moderate intensity.
Abdominal examination revealed a large cystic swelling in the
left upper abdomen. The patient had been operated for the
same complaint at a different hospital 3 months back, with a
diagnosis of pancreatic pseudocyst, and a drainage procedure
for the cyst had been performed. His symptoms however
persisted. He was evaluated with an ultrasound and
subsequently a CT scan of the abdomen which revealed 3 large
cysts in the abdomen, bulging from the anterior abdominal wall, separate from the adjacent viscera. However, the exact
site of origin of the cysts could not be determined. Hydatid
serology (by ELISA), cyst-fluid cytology, and cyst-fluid
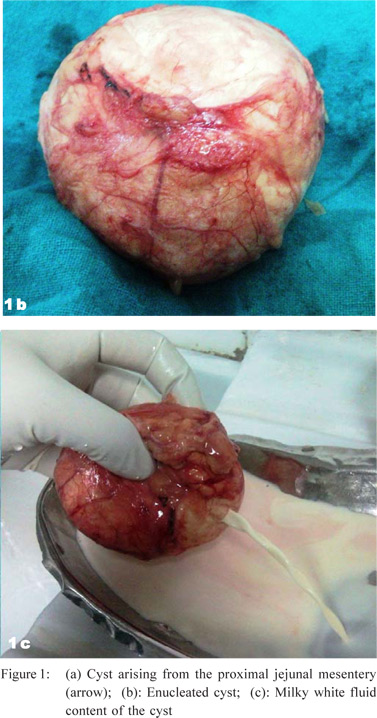
amylase were within normal limits. On surgical exploration, 3
large cysts were found arising from the mesentery of the
proximal jejunum, in close proximity to the superior mesenteric
artery. Aspiration of the cysts revealed milky-white fluid
(Figure 2a). The cysts were resected with a segment of the
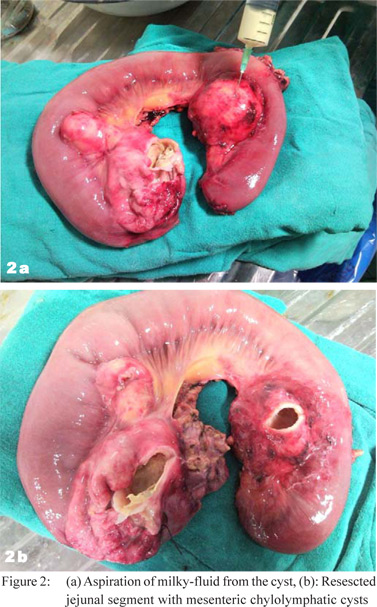
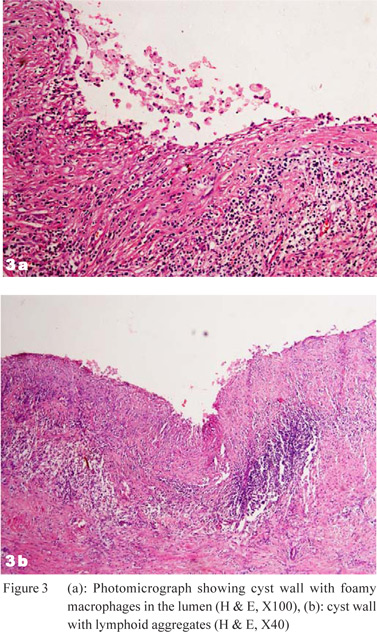
jejunum (Figure 2b). Histopathology revealed a cyst wall with
foamy macrophages and lymphoid aggregates (Figure 3a,3b).
The patient had an uneventful recovery and at a follow-up of 6
months, the patient is symptom-free, without evidence of
recurrence.
Discussion
Mesenteric cysts were first described in the 16th century.[1] They
are one of the rarest abdominal tumors and the incidence varies
from 1 per 100,000 to 250,000 admissions.[2] Among these
uncommon cystic lesions of the mesentery, chylolymphatic
cysts are extremely rare.[3] These cysts arise in sequestered
lymphatic channels or ectopic lymphatic tissue in the small
bowel mesentery and enlarge by accumulating both lymph and
chyle. The accumulation of chyle and lymph is thought to
result from an imbalance between the inflow and outflow of
fluid across these channels.[4] The cysts may be asymptomatic
or may manifest with abdominal pain, distension, lump, or
intestinal obstruction.[5] Both the patients in the present series
were symptomatic with abdominal pain.
The definite diagnosis of these lesions is difficult prior to
surgical exploration as there are no pathognomonic symptoms
or characteristic imaging findings. Abdominal radiographs are
usually non contributory, however may reveal dilated bowel
loops with air-fluid levels in the very rare patients with intestinal
obstruction which may result from compression of the adjacent
bowel by the cyst[6] or by mesenteric volvulus. The diagnosis
may be suggested by an ultrasound of the abdomen, which
may reveal a cystic lesion in relation to the bowel loops, away
from the adjacent viscera. A fluid-fluid level has been reported
as a characteristic finding of these cysts which results from an
upper fluid level due to the chyle, and a lower fluid level due to
the heavier lymph.[7] CT scan demonstrates the fluid attenuation
of the lesion and its relationship with the adjacent viscera. A characteristic chyle-lymph fluid level has also been described.[8]
However, in the present series, although the ultrasound and
the CT scan were able to detect a cystic lesion in the region of
the duodeno-jejunal flexure, away from the adjacent viscera, a
definitive preoperative diagnosis of chylolymphatic cyst could
not be made. Management of these cysts involves their removal
which may or may not involve resection of the adjacent bowel.
Most cysts can be enucleated (as in the 1st patient); however,
in some this is not possible without sacrifice of the blood
supply to the adjacent bowel and hence necessitates resection
(as in the 2nd patient). Procedures like marsupialization and
drainage are associated with high recurrence rates (as was in
the 2nd case) and are best avoided.[9]
Histopathology of the resected specimen reveals either
unilocular or multilocular cysts.[10] The cysts are usually lined
with single layer of endothelium, and may contain lymphoid
tissue and foam cells.[4,10]
Acknowledgements
We thank Dr. Kiran Chikkanahalli Subbarao for reviewing the
pathology slides and Council of Scientific and Industrial
Research, New Delhi for their support.
References
- Moynihan BG. Mesenteric Cysts. Ann Surg. 1897;26:1–30.
- Liew SC, Glenn DC, Storey DW. Mesenteric cyst. Aust N Z J Surg. 1994;64:741–4.
- Beahrs OH, Judd ES Jr, Dockerty MB. Chylous cysts of the abdomen. Surg Clin North Am. 1950;30:1081–96.
- Engel S, Clagett OT, Harrison Eg Jr. Chylous cysts of the abdomen. Surgery. 1961;50:593–9.
- Rattan KN, Nair VJ, Pathak M, Kumar S. Pediatric chylolymphatic mesenteric cyst - a separate entity from cystic lymphangioma: a case series. J Med Case Reports. 2009;3:111.
- Ratan SK, Ratan KN, Kapoor S, Sehgal T. Giant chylolymphatic cyst of the jejunal mesentry in a child: report of a case. Surg Today. 2003;33:120–2.
- Fujita N, Noda Y, Kobayashi G, Kimura K, Watanabe H, Masu K, et al. Chylous cyst of the mesentery: US and CT diagnosis. Abdom Imaging. 1995;20:259–61.
- Phillips GW, Senapati A, Young AE. Chylolymphatic mesenteric cyst: a diagnostic appearance on computed tomography. Br J Radiol. 1988;61:413–4.
- Kurtz RJ, Heimann TM, Holt J, Beck AR. Mesenteric and retroperitoneal cysts. Ann Surg. 1986;203:109–2.
- Handelsman JC, Ravitch MM. Chylous cysts of the mesentery in children. Ann Surg. 1954;140:185–93.