|
|
|
|
 |
 |
| |
 |
|
|
Original Articles |
|
|
|
|
|
Keywords :
Inflammatory bowel disease, ulcerative colitis, cryptitis |
|
|
Siddharth N Shah,1 Anjali D Amarapurkar,1 N Shrinivas,2 Rathi PM2
Department of Pathology1 and
Department of Gastroenterology2
TN Medical College & BYL Nair Charitable Hospital,
Mumbai, India.
Corresponding Author:
Dr. Anjali D Amarapurkar
Email: anjali1963@ gmail.com
DOI:
http://dx.doi.org/
Abstract
Introduction: The diagnosis of ulcerative colitis is based on combination of clinical, endoscopic and pathological findings. However cases have been reported showing atypical endoscopic and histological features in ulcerative colitis. Hence the objective of this study was to determine the atypical features of new onset ulcerative colitis in adult population.
Methods: A total 110 newly diagnosed cases of ulcerative colitis were enrolled in the study over a period of five years. The diagnosis of ulcerative colitis was made by correlating clinical, endoscopic and histological features. Biopsies from representative areas were processed routinely. Endoscopic and histological evaluation was carried out for atypical features.
Results: Majority of the patients (75.4%) were between 21-50 years of age with male to female ratio of 2.2:1. A significant number of patients showed atypical endoscopic findings in the form of rectal sparing in 12 (10.9%) and skip lesions in 24 (21.8%) patients. Atypical features noted on histology included normal surface epithelium in 8 (7.3%), predominant polymorphs in 42 (38%), predominant eosinophils in 7 (6.3%), normal crypt architecture in 1 (0.9%) and well preserved goblet cells in 30 (28%) cases.
Conclusion: A significant number of patients with new onset ulcerative colitis showed atypical pattern of disease endoscopically as well as histologically. Pathologists should be aware of these atypical findings in cases of ulcerative colitis so as to avoid misdiagnosis.
|
48uep6bbphidvals|417 48uep6bbph|2000F98CTab_Articles|Fulltext Introduction
Inflammatory bowel disease comprises the major proportion of non neoplastic lesions of colon and rectum. Incidence of inflammatory bowel disease worldwide is 0.5 to 24.5/100,000 inhabitants for ulcerative colitis and 0.1 to 16/100,000 inhabitants for Crohn’s disease.[1] In India the incidence of ulcerative colitis is 6.02/100,000 person per year.[2,3] Ulcerative colitis is characterized by erythema, friability of mucosa, loss of vascular pattern and/or ulceration on endoscopy, involving mainly distal colon in a continuous fashion. On histology it is characterized by mucosal ulceration, villiform or polypoidal surface, basal plamacytosis, crypt architectural abnormalities with loss of goblet cells. The final diagnosis of ulcerative colitis requires correlation between clinical, endoscopic and histological features.[4,5] However many times patients of ulcerative colitis can have atypical endoscopic or histological features.[6] In such cases there is a high possibility of misdiagnosis. Hence this study was aimed to determine atypical endoscopic and histological features of ulcerative colitis.
Methods
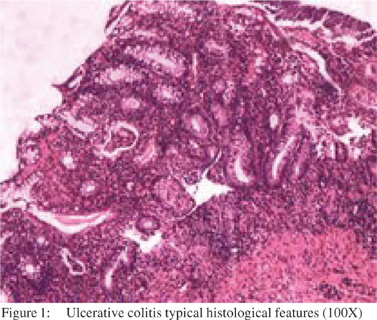
This is a retrospective analysis of newly diagnosed cases of ulcerative colitis over a period of five years. The diagnosis of ulcerative colitis was established by correlation of clinical, endoscopic and histological findings. The cases of infectious colitis or where the diagnosis of ulcerative colitis was uncertain were excluded from the study. Patients who had taken any specific medication for colitis or coexisting disease were also excluded. The patient medical records were retrieved form hospital data. Detailed endoscopic findings were analyzed, such as mucosal appearance, extent of disease, involvement of rectum, right sided colon and ileum. Skip lesions were also noted. All patients, in whom colonoscopic biopsies at the initial diagnosis were available, were included in the study. Colonoscopic biopsies were taken from representative areas before starting any specific therapy. In case of skip lesions, biopsies were taken from involved as well as uninvolved mucosa. Biopsy tissue was processed routinely and reported by two pathologists experienced in gastrointestinal pathology. Histological parameters assessed were, surface epithelial changes, lamina propria inflammation, lymphoid aggregates and crypt architectural abnormalities such as cryptitis, crypt abscesses, crypt shortening, bifurcation and loss of crypts. Goblet cell population was also observed and noted as focally or significantly decreased goblet cells or well preserved goblet cells. Muscularis mucosa was studied for the presence of hypertrophy. The slides were also reviewed for the presence of dysplasia or any unusual histopathological features. Each histological parameter was graded for its severity. Mucosal ulceration, villiform or polypoidal surface, basal plamacytosis, lymphoid hyperplasia, crypt architectural abnormalities (cryptitis, crypt abscess, shortening and branching of crypts) with loss of goblet cells and hypertrophy of muscularis mucosa were considered as characteristic features of ulcerative colitis (Figure 1). Special emphasis was given on atypical histological features of ulcerative colitis.
Results
Out of 110 cases, 76 (69%) were males and 34 (31%) females with a male to female ratio of 2.2:1. A majority (75.4 %) of the cases were between 21-50 years of age. The youngest patient was 15 years old while the eldest was 80 years of age (Table 1). The three most common symptoms amongst these patients were, bloody diarrhea present in all 110 (100%) cases, abdominal pain in 33 (30%) and fever in 14 (12.7%) cases. Other symptoms were non-specific. All these patients underwent colonoscopy with biopsy.
On colonoscopy left sided colitis with rectal involvement was seen in 73 cases (66.3%). Rectal sparing was seen in 12 (10.9%) cases. Continuous left sided disease with patchy right sided involvement was seen in 24 (21.8%). Entire colon right and left, continuous disease (pancolitis) was seen in 10 (9.3%) while skip lesions were present in 24 (21.8%) cases. There was not a single case showing only right sided colitis or endoscopically normal mucosa. (Table 2)
Surface epithelium was normal in 8 (7.3%) cases while it showed ulceration in 86 (78.2%), polypoidal configuration in 16 (14.5%) cases. Inflammation was mild in 1 (0.9%), moderate in 64 (58.1%) and severe in 45 (40.9%) cases. The predominant inflammatory cells in lamina propria were lymphocytes with basal plasmacytosis. Polymorphs were the predominant cells in 42 (38.1%) cases along with lymphocytes and plasma cells while eosinophils contributed as predominant cells in 7 (6.36%) cases along with plasma cells and lymphocytes. Lymphoid aggregates were present in 56 (50.9%) cases. Cryptitis was present in 106 (97.2 %) and crypt abscesses in 76 (69.7 %) cases. Chronic crypt architectural abnormality such as loss of crypts was observed in 43 (39.4%), and shortening of crypts in 31(28.4 %) cases. Goblet cells were well preserved in 30 (27.5%), focally reduced in 34 (31.2%) and significantly reduced in 46 (41.8%) cases. Muscularis mucosa hypertrophy was seen in 32 (29.1%) cases (Table 3).
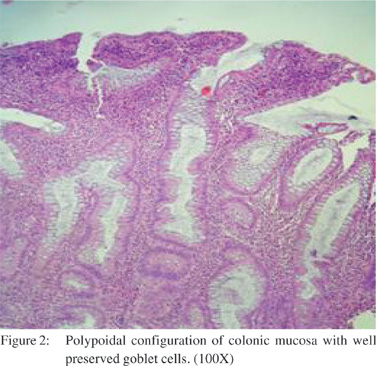
Amongst the unusual features seen in ulcerative colitis, endoscopic rectal sparing was seen in 12 (10.9%) and skip lesions in 24 (21.8%) cases. Cases in which rectal sparing was seen on endoscopy, did not show significant inflammation in rectum. Similarly in cases of skip lesions biopsies from normal looking areas on endoscopy showed near normal biopsy while from endoscopically involved areas showed evidence of ulcerative colitis. There was not a single case showing involvement of the ileum. On histopathological examination atypical features noted were normal surface lining epithelium in 8 (7.3%), predominant polymorphs in lamina propria in 42 (38%), predominant eosinophils in 7 (6.3%), normal crypt architecture in 1 (0.9%) and well preserved goblet cells in 30 (28%) (Table 4) (Figure 2).
Discussion
Conventional wisdom dictates that ulcerative colitis is a chronic mucosal disease affecting rectum and left sided colon and spreads proximally. The finding of rectal sparing or patchy involvement should raise the suspicion of Crohn’s disease.[7,8,9,10,11,12,13,14] These atypical features make pathological diagnosis more difficult which may delay in starting the treatment of patient. The atypical features are frequently noted in pediatric age group as compared to adults.[15,16] Various reasons have been documented for such features of ulcerative colitis, important being related to treatment. The therapy decreases inflammatory activity and results in patchy or discontinuous disease with preservation of goblet cells that closely resembles Crohn’s disease.[8,13]
Our results demonstrated that significant number of patients with new onset ulcerative colitis had atypical features. Classical colonoscopic findings such as loss of vascularity, edema, friable mucosa, erythema and ulcerations involving left sided colon were seen in 73 (66.3%) cases. Atypical features were rectal sparing in 12 (10.9%) and patchy lesions in 24 (21.8%) cases. Although rectal sparing and patchy disease suggest diagnosis of Crohn’s disease, colonoscopy with microscopic inflammatory changes of mucosa suggested the diagnosis of ulcerative colitis in our study. There are several reports in literature regarding rectal sparing and skip lesions. They have been attributed to either local use of steroids or they are the effects of oral treatment taken for the disease.[16,17,18,19,20,21,22,23] To avoid this, patients who did not receive any form of medical therapy prior to initial endoscopic procedure were included in this study.
Bernstein et al8 studied the prevalence of patchiness including rectal sparing in a group of 39 patients. Of these 17 (44%) had endoscopic evidence of patchiness including 5 (13%) with rectal sparing. However there was no correlation found between patchiness and rectal therapy. Also they have shown that these findings are neither related to rectal therapy nor it is restricted to those in remission. Kim et al[9] investigated the prevalence of endoscopic and histological patchiness and rectal sparing in treated cases of ulcerative colitis and correlated with treatment at time of endoscopy. Endoscopic patchiness was present in 11%, rectal sparing in 15% of sequential endoscopies. Sulfasalazine was the most common single treatment at the time of procedures. Also these changes did not seem to be related to any specific treatment (5 ASA or corticosteroids). Thus in patients of ulcerative colitis, pattern and extent of inflammation may vary significantly over period of time and treatment.
Considering histopathological changes of ulcerative colitis, in the present study, surface epithelium showed polypoidal appearances with ulceration in majority of cases. Normal surface epithelium which was considered as atypical feature was seen in 8 (7.3%) cases. The degree of inflammation varied, majority showing moderate to severe inflammation. Only in one case the inflammation was mild. Predominant inflammatory cells in lamina propria were lymphocytes and plasma cells with basal plasmacytosis. A significant number of cases 42 (38.1%) showed neutrophils as predominant inflammatory cells. In these cases it was difficult to differentiate the condition from acute infective colitis. It is a well known fact that in initial biopsies from acute phase of ulcerative colitis are difficult to differentiate from acute infective colitis. However accurate diagnosis of ulcerative colitis is possible if a detailed evaluation of biopsy is done with clinicopathological correlation.[17] In our 42 cases, acute inflammation was primarily based in epithelium rather than lamina propria and presence of associated chronic crypt injury served to distinguish ulcerative colitis from acute infective colitis. The diagnosis of ulcerative colitis in these cases was reached with the help of clinical and endoscopic correlation along with the histology. Coexisting bowel disease (enteric infections, ischemic colitis, diverticular disease and malignancy) may also alter the typical appearance of ulcerative colitis and hence such biopsies need to be reported carefully.
Eosinophils were predominant in 7 (6.3%) cases along with lymphocytes and plasma cells. None of these cases showed peripheral eosinophilia. There has been increasing evidence about the involvement of eosinophils in the pathogenesis of inflammatory bowel disease. Eosinophils play an important role as pro-inflammatory and pro-motility agents thus producing diarrhea, tissue destruction and fibrosis.[18,19,20]
Crypt architectural abnormalities were seen in all 109 cases, which were in the form of cryptitis, crypt abscesses, loss of crypts and shortening of crypts. There was only one case in which crypts were normal. Reduced number of goblet cells is a very good marker and is well appreciated in acute phase of ulcerative colitis.[21] In this study 30 (27.5%) cases showed well preserved goblet cells which was considered an atypical feature. Wu et al[22] studied the effectiveness of Moxibustion on the morphology of colonic mucosa in ulcerative colitis before and after treatment. They have shown that goblet cells were markedly reduced before treatment and a significant improvement in goblet cells was seen after the treatment.
Zaitoun et al[23] performed morphometric measurements on rectal biopsy specimens from 10 normal control subjects and 33 patients with relapse of ulcerative colitis before and after treatment. They have shown that the ratio of goblet cells to epithelial cells increased after treatment with both steroid and 5ASA. Ajioka et al[24] have reported that in remission phase of ulcerative colitis inflammation is reduced and goblet cell mucus is restored however, evidence of past inflammation such as irregular crypts, paneth cell metaplasia and muscularis mucosa hypertrophy can still be well appreciated. As against this Zhong et al[25] did not show any effect of treatment on goblet cell depletion.
Levine et al[10] evaluated rectal biopsy specimens from a prospective group of 24 asymptomatic patients with an established diagnosis of ulcerative colitis along with 10 normal rectal biopsy specimens as control subjects. [11] (46%) of the 24 patients had a rectal biopsy that was devoid of characteristic findings on which a diagnosis of ulcerative colitis could be made. They concluded that a normal rectal biopsy may occur in longstanding colitis. Kleer et al[12] analyzed sequential sets of biopsies of 41 patients to recognize the great variability in the histological and endoscopic appearances of ulcerative colitis. Endoscopic skip lesions developed in 5 (12%) patients. They found that there was lack of endoscopic and histological correlation in 1/3 rd cases. The results of their study stressed that the finding of normal rectal mucosa both endoscopic and histological is not uncommon in patients of ulcerative colitis either at the beginning or later in the course of the disease.
Also their study emphasized that ulcerative colitis may show variability in endoscopic and histological appearance with skip areas and non diffuse distribution of inflammatory changes. In conclusion, a significant number of patients with new onset ulcerative colitis showed atypical pattern of the disease. Pathologist should be aware of these atypical histological and endoscopic appearances in ulcerative colitis so as to avoid misdiagnosis.
References
- Lakatos PL. Recent trends in epidemiology of inflammatory bowel disease: up or down? World J Gastroenterol. 2006;12:6102–8.
- Sood A, Midha V. Epidemiology of inflammatory bowel disease in Asia. Indian J Gastroenterol. 2007;26:285–9.
- Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–7.
- Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterology. 2007;133:1670–89.
- Ghosh S, Shand A, Ferguson A. Ulcerative colitis. BMJ. 2000;320:1119–23.
- Finkelstein SD, Sasatomi E, Regueiro M. Pathologic features of early inflammatory bowel disease. Gastroenterol Clin N Am. 2002;31:133–45.
- Robert ME, Skacel M, Ullman T, Bernstein CN, Easely K, Goldblum J. Patterns of colonic involvement at initial presentation in ulcerative colitis. a retrospective study of 46 newly diagnosed cases. Am J Clinical Pathol. 2004;122:94–9.
- Bernstein CN, Shanahan F, Anton PA, Weinstein WM. Patchiness of mucosal inflammation in treated ulcerative colitis: a prospective study. Gastrointest Endosc. 1995;42:232–7.
- Kim B, Barnett JL, Kleer CG, Appelman HD. Endoscopic and histological patchiness in treated ulcerative colitis. Am J Gastroenterol. 1999;94:3258–62.
- Levine TS, Tzardi M, Mitchell S, Sowter C, Price AB. Diagnostic difficulty arising from rectal recovery in ulcerative colitis. J Clin Pathol. 1996;49:319–23.
- Geboes K. Pathology of inflammatory bowel diseases: variability with time and treatment. Colorectal Dis. 2001;3:2–12.
- Kleer CG , Appelman HD. Ulcerative colitis: patterns of involvement in colorectal biopsies and changes with time. Am J Surg Pathol. 1998;22:983–9.
- Geboes K, Dalle I. Influence of treatment on morphological features of mucosal inflammation. Gut. 2002;50:37–42.
- Singh B, Warren BF. The effects of treatment on histology inflammatory bowel disease. European Gastroenterology Review. 2005;September:34–6; (Reference Section) 1–6.
- Glickman JN, Bousvaros A, Farraye FA, Zholudev A, Friedman S, Wang HH, et al. Paediatric patients with untreated ulcerative colitis may present initially with unusual morphologic findings. Am J Surg Pathol. 2004;28:190–7.
- Robert ME, Tang L, Hao LM, Reyes-Mugica M. Patterns of inflammation in mucosal biopsies of ulcerative colitis: perceived differences in pediatric populations are limited to children younger than 10 years. Am J Surg Pathol. 2004;28:183–9.
- Nostrant TT, Kumar NB, Appelman HD. Histopathlogy differentiates acute self-limited colitis from ulcerative colitis. Gastroenterology. 1987;92:318–28.
- Uzunismail H, Hatemi I, Doðusoy G, Akin O. Dense eosinophilic infiltration of the mucosa preceding ulcerative colitis and mimicking eosinophilic colitis: report of two cases. Turk J Gastroenterol. 2006;17:53–7.
- Lampinen M, Rönnblom A, Amin K, Kristjansson G, Rorsman F, Sangfelt P, Eosinophil granulocytes are activated during the remission phase of ulcerative colitis. Gut. 2005;54:1714–20.
- Al-Haddad S, Riddell RH. The role of eosinophils in inflammatory bowel disease. Gut. 2005;54;1674–5.
- Jenkins D, Balsitis M, Gallivan S, Dixon MF, Gilmour HM, Shepherd NA, Guidelines for the initial biopsy diagnosis of suspected chronic idiopathic inflammatory bowel disease. The British Society of Gastroenterology Initiative. J Clin Pathol. 1993;50:93–105.
- Wu HG, Zhou LB, Shi DR, Liu SM, Liu HR, Zhang BM, Morphological study on colonic pathology in ulcerative colitis treated by moxibustion. World J Gastroenterol. 2000;6:861–5.
- Zaitoun AM, Cobden I, al Mardini H, Record CO. Morphometric studies in rectal biopsy specimens from patients with ulcerative colitis: effect of oral 5 amino salicylic acid and rectal prednisolone treatment. Gut. 1991;32:183–7.
- Ajioka Y, Nishikura K, Watanabe G. Pathomorphology of ulcerative colitis. Nippon Rinsho. 2005;63:763–9.
- Zhong YQ, Huang HR, Zhu ZH, Chen QK, Zhan J, Xing LC. Effects of sulfasalazine on biopsy mucosal pathologies and histological grading of patients with active ulcerative colitis. World J Gastroenterol. 2005;11:4435–8.
|
|
|
 |
|
|