48uep6bbphidvals|392
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Bronchobiliary fistula (BBF), a rare disorder, is defined as the passage of bile in the bronchi leading to presence of bile in the sputum (biloptysis).[1] The diagnosis of BBF requires a high degree of suspicion. Although hydatid disease is still the leading cause of acquired BBF, various other etiologies are responsible for 20% of the reported cases.[1,2] We are reporting the first case of BBF in a patient of pulmonary tuberculosis, a poor responder to anti-tubercular therapy alone, treated successfully with anti-tubercular drugs and endoscopic therapy.
Case Report
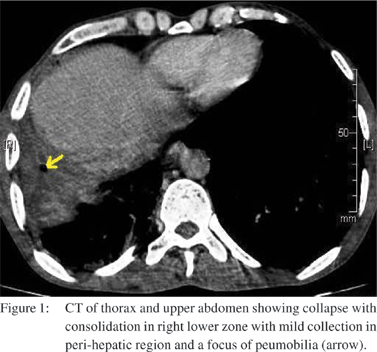
A 40 year old male, a chronic smoker presented with 1 month history of paroxysmal cough and yellow-green expectoration, low grade fever, anorexia and weight loss. He had tubercular right pleural effusion 15 years back. On examination, he had pallor. On chest examination, there were fine crepitations over right infra-scapular area. Blood analysis revealed hemoglobin of 11.5gm/dl with normocytic normochromic picture. Liver function tests were normal. Sputum was tested positive for acid fast bacilli (AFB) as well as bile salt and bile pigments. Chest radiograph revealed patchy consolidation in lower zone of right lung. Bronchoscopy revealed oozing of yellowish secretions coming from the right lower lobe. Hydatid and amoebic serological tests were negative. Ultrasonography abdomen showed mild hepatosplenomegaly. Computed tomography (CT) of thorax and upper abdomen (Figure 1) showed collapse with consolidation in right middle and lower zone with few small pre-tracheal, para-tracheal and sub-carinal lymph nodes and mild collection in peri-hepatic region with few foci of pneumobilia.
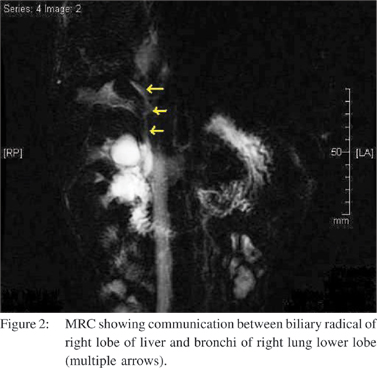
A diagnosis of pulmonary tuberculosis with BBF was made and antitubercular therapy (WHO category-I) was started. Two months later, the patient became afebrile, his appetite improved, he gained weight and sputum became negative for AFB, but he continued to have bilioptysis. Magnetic resonance cholangiography (Figure 2) showed communication between right biliary radical and bronchi of right lung lower lobe. In view of persistent bilioptysis, endoscopic retrograde cholangiography was done which showed communication between right hepatic duct and lung parenchyma. Endoscopic sphincterotomy with placement of a 7 FG, 12 cm double pigtail plastic stent was done. After two weeks of endoscopic therapy, bilioptysis was dramatically reduced and two months later, the patient became asymptomatic. He completed short course antitubercular therapy with no further complications.
Discussion
Tuberculosis is one of the most common causes of infectious fistulas in our country where tuberculosis has high prevalence. Published literature of BBF in relation to tuberculosis is very limited. We found 3 previous case reports of BBF in relation with hepatic tuberculosis and a case report of superimposed pulmonary tuberculosis in alveolar hydatid disease.[3,4,5,6] BBF described in hepatic tuberculosis were in relation with, ruptured tubercular macronodule, ruptured tubercular abscess and old calcified tuberculous hepatic granuloma.[3,4,5] We did not find any report about BBF caused by pulmonary tuberculosis. This is the first report that describes a case of BBF in a patient of pulmonary tuberculosis. This case of BBF is likely to be caused by pulmonary tuberculosis because of three reason: patient had extensive pulmonary involvement with positive AFB in sputum, no evidence of other known predisposing factors of BBF were identified and although virtually all cases of BBF have arisen because of pathology within the liver however, literature suggests that pulmonary involvement in alveolar hydatid disease can lead to BBF formation.[6]
The mechanism of transdiaphragmatic extension of BBF is controversial. The BBF in this case may be the result of erosions triggered by chronic granulomatous inflammatory reaction. BBF can be treated endoscopically or surgically.[1,7] Endoscopic sphincterotomy and biliary drainage have been used successfully for treatment of the fistula.[6,7] BBF described in relation with tuberculosis were treated successfully with antitubercular therapy.[3,4,6] However, our case was a poor responder to antitubercular therapy and endoscopic therapy was needed for the faster healing of fistula.
References
1. Gugenheim J, Ciardullo M, Traynor O, Bismuth H. Bronchobiliary fistulas in adults. Ann Surg. 1988;207:90–4.
2. Eryigit H, Oztas S, Urek S, Olgac G, Kurutepe M, Kutlu CA. Management of acquired bronchobiliary fistula: 3 case reports and a literature review. J Cardiothorac Surg. 2007;2:52.
3. Flemma RJ, Anlyan WG. Tuberculous Bronchobiliary Fistula. Report of an Unusual Case with Demonstration of the Fistulous Tract by Percutaneous Transhepatic Cholangiography. J Thorac Cardiovasc Surg. 1965;49:198–201.
4. Tsunoda T, Shiogama T, Koga M, Kohara N, Eto T, Motoshima K, et al. Tuberculous liver abscess with bronchobiliary and gastrobiliary fistulae—a case report. Jpn J Surg. 1991;21:100–4.
5. Chong CF, Chong VH, Jalihal A, Mathews L. Bronchobiliary fistula successfully treated surgically. Singapore Med J. 2008;49:e208–11.
6. Senturk H, Mert A, Ersavasti G, Tabak F, Akdogan M, Ulualp K. Bronchobiliary fistula due to alveolar hydatid disease: report of three cases. Am J Gastroenterol. 1998;93:2248–53.
7. Yilmaz U, Sahin B, Hilmioglu F, Tezel A, Boyacioglu S, Cumhur T. Endoscopic treatment of bronchobiliary fistula: report on 11 cases. Hepatogastroenterology. 1996;43:293–300.