48uep6bbphidvals|363
48uep6bbph|2000F98CTab_Articles|Fulltext
Introduction
Although bleeding occurs less often from gastric varices (GV) than from esophageal varices (EV), it has a poorer prognosis and is associated with more severe blood loss, a higher rebleeding rate, and a higher mortality rate.[1,2,3] However, limited data exists on the best treatment for GV hemorrhage (GVH).Endoscopic treatment for GVH includes injection of sclerosants or thrombin[4,5] and endoscopic band ligation.[6,7]
The success rate in controlling GVH by endoscopic injection of N-butyl-2-cyanoacrylate appears higher than for other sclerosants according to previous non-randomized trials.[8,9] Although endoscopic variceal ligation is regarded as the optimal endoscopic treatment for esophageal variceal haemorrhage, the safety and efficacy of this approach for the treatment of GVH is uncertain.[7,10] The re-bleeding rate of GV is variable and ranges from 10% to 42%.[11] There are two randomized trials published comparing EVL with cyanoacrylate injection for control of GVH with results in favor of cyanoacrylate injection.[12,13]
Junctional varix is defined as gastroesophageal varices type 1 which extends beyond the gastroesophageal junction and is always associated with esophageal varices. It usually appears
as a continuation of esophageal varices and extend 2-5 cm below the gastroesophageal junction along the lesser curve of the stomach. There is no sufficient data about the management
of junctional varices.
This randomized study was performed to compare the efficacy and safety of endoscopic variceal ligation versus endoscopic cyanoacrylate injection in the treatment of bleeding junctional varices .
Methods
Patient selection
This randomized control clinical trial was conducted at three endoscopy centers in upper Egypt: Assiut, Minya and Al-azhar university hospitals. From January 2008 to September 2009, 150 consecutive patients with active bleeding from junctional varices were recruited in this study. They were 108 males and 42 females. The inclusion criteria were: 1) Patients with portal hypertension based on results of clinical, laboratory and imaging studies; 2) Patients with clinical signs of hematemesis, melena or hematochezia; 3) Patients with active bleeding fom junctional vaices which was defined as active spurting or oozing of blood from the junctional varix; 4) Patients who gave informed written consent.
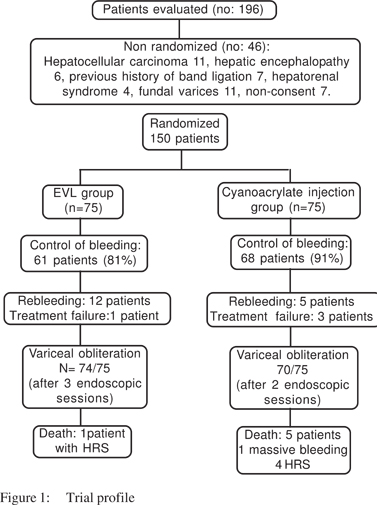
The exclusion criteria were: 1) Undetermined source of bleeding; 2) Previous history of sclerotherapy, band ligation or shunt operation; 3) Patients with hepatic encephalopathy or hepatorenal syndrome; 4) Associated advanced hepatocellular carcinoma, cerebral vascular accidents or other debilitating diseases; 5) Non-compliant patients or patients unwilling to sign an informed consent. In compliance with exclusion criteria, 46 patients had to be excluded (Figure 1). Severity of liver disease was assessed using Pugh modification of Child classification.
Design of the study
The study was approved by the hospital research and ethics committee of our hospitals.
Eligible patients were randomized into two groups using consecutively numbered opaque-sealed envelopes containing the treatment assignment to receive either endoscopic variceal ligation or endoscopic cyanoacrylate injection.
All patients were subjected to thorough clinical history and examination, laboratory investigations including liver function tests, blood urea, serum creatinine, hemoglobin and platelet count.
Standard therapy like blood and frozen plasma transfusion, fluid replacement, systemic antibiotics and lactulose were given whenever indicated. All patients received emergency upper endoscopy within 24 hours of admission. After establishment of the diagnosis of bleeding junctional varices, randomization was done by an assistant and the endoscopic therapy was applied at once with a well trained endoscopist.
Endoscopic procedures
Preparation: Midazolam 5mg IV as light sedation and antibiotic prophylaxis using 1gm ceftriaxone IV just before the procedure.
The technique for EVL was as follow: Ligation was performed using Pentax video endoscope 3440 and Wilson cook six shooter band ligator device. Full 360-degree contact between varix and the cylinder of the device was achieved. Suction was applied until endoscopic “red-out” occurred. At that point, gentle clockwise rotation of the crank at the biopsy port pulled the distal band forward and released it around tissue in the chamber. Discontinuing suction then released the freshly banded tissue out of the cylinder. An adjacent column of varices was sought and the process repeated.
The technique for cyanoacrylate injection was as follow: Using the endoscope, N-butyl-2-cyanoacrylate (Histoacryl Blue, Germany) was injected intravariceally, using 21-gauge disposable injection needle. Each aliquot contained 0.5 ml cyanoacrylate and 0.7 ml Lipiodol (Guebet laboratory, Aulnay- Sous-Bris, France).
To prevent the liquid tissue adhesive from adhering to the endoscope, a few milliliters of silicone oil were smeared over the tip of the endoscope and sucked through the working channel. To prevent Histoacryl from adhering to the catheter wall, lipiodol was injected into the catheter. Having localized the bleeding site, the bleeding varix was punctured at or in the vicinity of the rupture point in the usual manner for intravariceal injection. Paravariceal injection was avoided to prevent severe tissue ulceration.
Bleeding site was ligated or injected first and then the surrounding prominent varices were also ligated or injected as possible. For patients with concomitant esophageal varices, EVL was performed immediately after treatment of junctional varices for both groups during the same session. Treatment interval was similar to management of junctional varices until obliteration of esophageal varices. After band ligation and cyanoacrylate injection, all patients were given IV omeprazole 40mg every 12 hours for 48 hours.
Follow up
Endoscopic treatment was repeated every 2 weeks until variceal obliteration achieved. Endoscopy was performed 6 month later to detect recurrence of varices.
End points
The primary end point was initial hemostasis which was defined as cessation of bleeding for more than 72 hours. If re-bleeding occurred and proved to originate from junctional varices, repeat session of the previous treatment was performed. Secondary end points were survival time and complications or death.
Definitions
Junctional varices were defined according to Sarin classification3 as gastroesophageal varices type 1 which extend beyond the gastroesophageal junction and always associated with esophageal varices.
Active bleeding was seen when endoscopic findings showed active spurting or oozing of blood from junctional varices Variceal obliteration was considered when varices disappeared or reduced to grade 1 and /or when it was not possible to aspirate into the ligation chamber.
Re-bleeding was defined as new onset of hematemesis, hematochezia or melena with variceal bleeding within 24 hours of stable vital signs after endoscopic management. Treatment failure was defined as two or more rebleeding episodes from junctional varices or death.
Statistical Analysis
Results were expressed as mean ± standard deviation (SD) or number (%). Comparison was made between the mean values. Comparison between categorical data [n (%)] was done using Chi square test. SPSS computer program (version 11 windows) was used for data analysis. A p value equal to or less than 0.05 was considered significant; less than 0.01 was considered highly significant.
Results
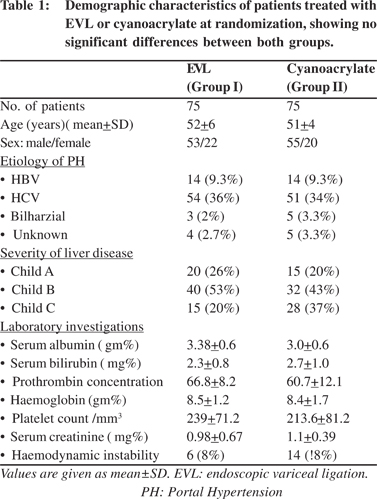
Both groups at the time of inclusion were similar with regard to demographic data, clinical and laboratory findings. They were 108 males (72%) and 42 females (28%). Their age ranged from 20 to 60 years with a mean + SD of 52.0+6.0 years (Table 1).
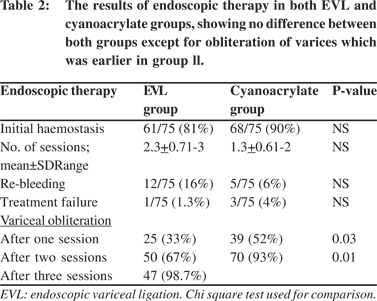
All patients received endoscopic therapy, either band ligation or endoscopic cyanoarylate injection. Control of active variceal bleeding was achieved in 61 patients in group I (81%) and in 68 patients in group II (91%). Although the initial haemostasis was observed at a higher frequency in patients of group II (68/75) than in patients of group I (61/75) but it was of no statistical significance (p=0.07). Re-bleeding was seen in total 17 patients: 12 patients (16%) in the EVL group and 5 patients (6%) in the cyanoacrylate group.
Treatment failure was encountered in total 4 patients; one patient in group I and 3 patients in group II. The number of sessions needed for obliteration of varices ranged from 1-3 (mean 2.3±0.7) in group I and from 1-2 (mean 1.3±0.6) in group II with no statistical significance. Variceal obliteration was achieved by one session in 25 patients in group I and in 39 patients in group II (p=0.03), while it was achieved after the second session in 50 patients in group l versus 70 patients in group ll (p=0.01). The remaining 24 patients in group I achieved eradication after 3 sessions (Table 2).
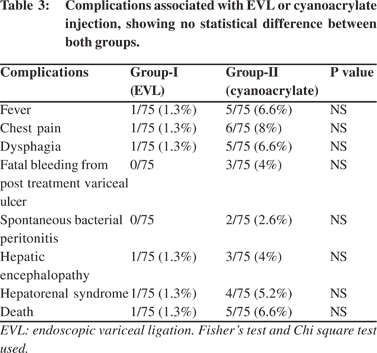
Complications
Fever, chest pain and dysphagia were observed more frequently in group II (31 patients) than in group I (6 patients) (p=0.001). Fatal bleeding from huge post sclerotherapy ulcer was seen in 1 patient in group II and in none in group I. Long term complications as spontaneous bacterial peritonitis, hepatic encephalopathy and hepatorenal syndrome (HRS) were also observed more frequently in patients of group II than group I, but with no statistical significance.
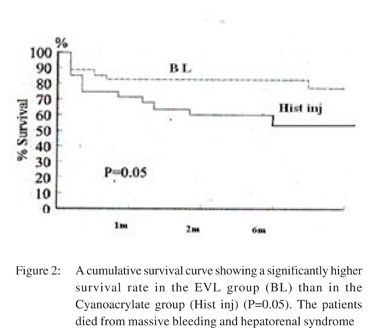
Death occurred in one case (1.3%) in group I due to HRS and in 5 cases (6.6%) in group II, 1 died from massive bleeding and 4 due to HRS (Table 3). The occurrence of complications and death increased according to severity of liver disease by Child classification. Among patients with Child A there was neither complications nor death in both groups, while in patients with Child B there were 12 patients with complications; 2 patients in group I and 10 patients in group II and only one case died in group II. In patients with Child C; 25 patients encountered complications; only 4 patients in group 1 and 21 patients in group II. Five patients with Child C died; 4 of them in group II and only one patient in group I. At six months , a significantly higher survival rate was seen in the group l than in group ll (Figure 2).
Discussion
It is generally accepted that bleeding from gastric varices is less frequently encountered than from esophageal varices. Approximately 14% to 36% of acute variceal bleeding arises from gastric varices.[14,15] However, bleeding from gastric varices is usually more severe than from esophageal varices.[2,3] It is noted that the bleeding from gastric varices requires greater amount of blood transfusion and has greater fatality rate than esophageal variceal bleed.[16]Whereas injection sclerotherapy has been applied to treat active bleeding from GV, its use in GVH is associated with a high re-bleeding rate and a frequent need to resort to surgical intervention and thus is regarded as only a temporary hemostatic measure.[2,17] The success rate to control GVH by endoscopic injection of N-butyl-2- cyanoacrylate appeared higher than other sclerosants according to previous non-randomized trials.[8,9]
The endoscopic variceal ligation has been suggested as the treatment of choice for EVH.[18] The hematostatic effect of endoscopic variceal ligation (EVL) for GVH appeared promising, but evidence is still limited[6,7] However, a randomized trial was conducted to compare the efficacy of EVL versus cyanoacrylate injection on GVH, and its conclusions were against the use of EVL for the treatment of GVH.[12]In comparison with previous studies, this study included only patients with acute and active bleeding where urgent endoscopy was done within 24 hours of gastroesophageal bleeding. Also this study was restricted to patients with junctional variceal bleeding (gastroesophageal varices type1) only, and not all types of gastric varices. Further, the number of acute gastroesophageal bleeding patients enrolled by us, is a large cohort for a trial on active bleeding junctional varices.
The success rate in controlling active bleeding was 81% in the EVL group versus 91% in the cyanoacrylate group. Most previous studies were done for all types of gastric varices and not junctional varies alone. In a study done by Tan et al comparing band ligation versus cyanoacrylate injection in the treatment of acute gastric variceal bleeding, the success rate of cyanoacrylate and band ligtion to control bleeding was 93.3%. But in their study, the investigators recruited only a small number of cases with active bleeding (15 cases).[13] Another study by Lo et al included 13 patients with GOV1 treated with cyanoacrylate with control of active bleeding in 85% of cases(11/13), while only 7 patients were in the band ligation group with 43% success rate of controlling active bleeding.[12]In our study, re-bleeding occurred in 12 patients in EVL group (16%) versus 5 patients in cyanoacrylate group (6%). This rebleeding rate was similar or probably less than that reported in previous studies where it ranged from 18.5% to 31%.[9,12,19]
In our study, the risk of re-bleeding was lower than previous studies probably due to inclusion of only patients with junctional varices and exclusion of cases with advanced hepatocellular carcinoma which is a major risk factor of rebleeding.[20] A patient suffered from massive rebleed after cyanoacrylate injection and died owing to big ulcerations following the injection and it was not possible to control the bleed. This patient had been having severe active bleeding and was categorized as Child C liver cirrhosis. Otherwise all cases with re-bleeding were treated by the same previous method used for initial hemostasis except one case in the EVL group where cyanoacrylate was used as a rescue procedure to control bleeding.
The complications were more in the cyanoacrylate group. Fever was mild and low grade in both groups apart from the two cases with spontaneous bacterial peritonitis in cyanoacrylate group. Chest pain and dysphagia occurred more in the cyanoacrylate group. Other complications were comparable in both groups. Infectious complications were less than previous studies may be because of antibiotic prophylaxis.[21,22]
Variceal obliteration in EVL group was possible in 33.3% of patients in the first session and 67 % of patients after the second session and 99% of patients after three sessions, while variceal obliteration in cyanoacrylate group was achieved in 52% of patients after the first session and in 93% patients after the second session. Although variceal obliteration was earlier and with lower re-bleeding rate in the cyanoacrylate group, the variceal obliteration was 99% after 3 sessions and with lower complication rate in EVL group. No difference in mortality rate was observed between the two groups.
In summary, esophageal variceal ligation of bleeding junctional varices may be as effective as cyanoacrylate injection along with an advantage of lower complication rate in control of bleeding junctional varices. Although the re-bleeding rate was more in EVL group than cyanoacrylate group it was easily managed.
References
1. De Franchis R, Primignani M. Natural history of portal hypertension in patients with cirrhosis. Clin Liver Dis. 2001;5:645–63.
2. Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc. 1986;32:264–8.
3. Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–9.
4. Heneghan MA, Byrne A, Harrison PM. An open pilot study of the effects of a human fibrin glue for endoscopic treatment of patients with acute bleeding from gastric varices. Gastrointest Endosc. 2002;56:422–6.
5. Yang WL, Tripathi D, Therapondos G, Todd A, Hayes PC. Endoscopic use of human thrombin in bleeding gastric varices. Am J Gastroenterol. 2002;97:1381–5.
6. Shiha G, El-Sayed SS. Gastric variceal ligation: a new technique. Gastrointest Endosc. 1999;49:437–41.
7. Lee MS, Cho JY, Cheon YK, Ryu CB, Moon JH, Cho YD, et al. se of detachable snares and elastic bands for endoscopic control of bleeding from large gastric varices. Gastrointest Endosc. 2002;56:83–8.
8. Ramond MJ, Valla D, Mosnier JF, Degott C, Bernuau J, Rueff B, t al. Successful endoscopic obturation of gastric varices with butyl cyanoacrylate. Hepatology. 1989;10:488–93.
9. Oho K, Iwao T, Sumino M, Toyonaga A, Tanikawa K. Ethanolamine oleate versus butyl cyanoacrylate for bleeding gastric varices: a nonrandomized study. Endoscopy. 1995;27:349–54.
10. Lo GH, Lai KH. Is endoscopic ligation therapy with large detachable snares and elastic bands really safe and effective? Gastrointest Endosc. 2003;57:438–40.
11. Sarin SK, Primignani M, Agarwal SR. Gastric varices. In: de Franchis R, editor. Portal Hypertension III. Proceedings of the third Baveno International Concensus Workshop on definitions, methodology and therapeutic strategies. Oxford:Blackwell Science;2001.p.76–94.
12. Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060–4.
13. Tan PC, Hou MC, Lin HC, et al. A randomized trial of endoscopic treatment of acute gastric variceal haemorrhage:N-Butyl-2- cyanoacrylate injection vs band ligation. Hepatology. 2006;43:690–7.
14. Teres J, Cecilia A, Bordas JM, Rimola A, Bru C, Rodés J. Esophageal tamponade for bleeding varices. Controlled trial between the Sengstaken Blakemore tube and the Linton Nachlas tube. Gastroenterology. 1978;75:566–9.
15. Korula J, Chin K, Young KO, Yamada S. The demonstration of two distinct subsets of gastric varices: observations during a seven-year study of endoscopic therapy. Dig Dis Sci. 1991;36:303–7.
16. Bretagne JF, Dudicourt JC, Morisot D. Is endoscopic variceal sclerotherapy effective for the treatment of gastric varices? Dig Dis Sci. 1986;31:A505S.
17. Gimson AE, Westaby D, Williams R. Endoscopic sclerotherapy in the management of gastric variceal haemorrhage. J Hepatol. 1991;13:274–8.
18. Laine LA. Endoscopic treatment of acute or active variceal bleeding. In: de Franchis R, editor. Portal Hypertension III. roceedings of the third Baveno International Concensus Workshop on definition, methodology and therapeutic strategies. Oxford:Blackwell Science; 2001.p.156–60.
19. Sarin SK, Jain AK, Jain M, Liu TT, Lee FY, Chang FY, et al. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol. 2002;97:1010–5.
20. Chen WC, Hou MC, Lin HC, et al. Feasibility and potential benefit of maintenance endoscopic variceal ligation in patients with unresectable hepatocellular carcinoma and acute esophageal variceal: a controlled trial. Gastrointest Endosc. 2001;54:18–23.
21. Bernard B, Grange JD, Khac EN, Lee FY, Yeh YY, Chang FY, et al. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a metaanalysis. Hepatology. 1999;29:1655–61.
22. Hou MC, Lin HC, Liu TT, Kuo BI, Lee FY, Chang FY, et al. Antibiotic prophylaxis after endoscopic therapy prevents rebleeding in acute variceal hemorrhage: a randomized trial. Hepatology. 2004;39:746–53.